Abstract
Interstitial cystitis (IC) is a symptom complex of urinary urgency, frequency and pelvic pain. Multimodality behavioral and phamacologic treatment is often effective in treating IC. Unfortunately, some patients with IC are refractory to standard treatments. Neuromodulation has been shown to be effective in treating voiding dysfunction. Small studies have demonstrated improvement in pelvic pain and IC symptoms during temporary sacral nerve stimulation. This current study demonstrates that patients refractory to traditional therapies for IC can respond well to sacral nerve stimulation and maintain improvement in symptoms after permanent implantation of a neurogenerator. The technique used to place the neurostimulator can impact on the degree of the response and the complication rate. Sacral neurostimulation continues to evolve and should be in the armamentarium available to treat voiding dysfunction.
Key words: Interstitial cystitis, Neuromodulation, Pelvic pain, Sacral nerve
Interstitial cystitis (IC) is a symptom complex of urinary urgency, frequency, and pelvic pain. Many patients with IC will respond to multimodality therapy, including behavioral and pharmacologic treatments. Unfortunately, a subset of IC patients continues to suffer from the disease despite having tried all standard therapies. Not only is IC associated with urinary frequency and pelvic pain, but many IC patients complain of urinary hesitancy, intermittent stream, irritable bowel symptoms, and vaginal pain. IC may be a primary bladder disease in some patients; in others, however, it becomes a diffuse pelvic syndrome that may not respond to therapies directed to the bladder or to other end organs.1
Nerves are involved in all motor and sensory functions of the body, and an abnormal upregulation of these nerves from chronic stimulation can lead to pathologic conditions. Thus, it appears logical to investigate neuromodulation as a means to treat the symptoms of IC. The first reports on the use of electric stimulation to treat IC involved transcutaneous electrical nerve stimulation (TENS) and intravaginal stimulation.2 There are, however, no good controlled trials on electrostimulation for IC. Several studies have been published looking at various modes of stimulation to treat IC, including acupuncture, TENS, intravaginal or intrarectal routes, or tibeal nerve stimulation.3–5 However, the long-term success has been poor.
Sacral Nerve Stimulation
The direct stimulation of sacral nerve roots to treat voiding dysfunction has been studied for many years.6,7 Recently, transforaminal sacral nerve stimulation with an implantable neuroprosthetic device (Interstim®, Medtronic, Inc., Minneapolis, MN) was approved by the U.S. Food and Drug Administration (FDA) for refractory, nonobstructive urinary retention, urinary frequency, urgency, and urge incontinence. With this procedure, the clinical response is assessed by placing a lead through the S3 foramen and the patient wearing a temporary external stimulator for several days while the voiding parameters are being measured. If the patient responds to the test stimulation, a permanent lead and generator can be implanted and programmed for chronic stimulation. Sacral nerve modulation has not been approved specifically for IC, but recent studies have been published showing improvement in typical IC symptoms with a temporary test stimulation.8,9 In addition, studies have demonstrated an improvement in chronic, intractable pelvic pain with sacral nerve modulation.5,10
The objective of this current study was to assess the efficacy of sacral nerve modulation in treating refractory IC. The response to test stimulation and permanent implantation was assessed prospectively. Factors that might influence the clinical response were also addressed, along with the complications associated with sacral nerve modulation therapy.
Methodology
In this study, patients with refractory IC elected to undergo sacral nerve modulation to assess the clinical response. The patients completed voiding diaries and pain scores before the initial test and during the stimulation period. A positive response was defined as at least a 50% improvement in the most bothersome symptoms and the patient’s desire to undergo a permanent implantation. Two distinct procedures were used for the initial test and permanent implantation (Interstim).
The initial description and subsequent FDA approval for assessing the efficacy of sacral nerve modulation involved placement of a percutaneous lead through a needle that was passed in the sacral foramen.11,12 This lead was secured to the skin and connected to an external generator, which was worn for several days while measuring voiding function. The lead was then removed, and if the patient responded a permanent lead was placed in the operating room along with a subcutaneous generator. Unfortunately, use of this temporary lead was fraught with many problems, including a low response rate, which may have been due to limitation in programming capabilities and lead migration.
In 1997 Janknegt and colleagues13 described a staged procedure for assessing response to sacral nerve modulation, but the complexity of placing the permanent lead limited this approach to only those patients who have failed a traditional percutaneous procedure. Recently, Chai and Mamo14 described a minimally invasive approach to placing a permanent lead. We combined both of these strategies into our staged procedure and modified the technique by ensuring that the sensory component was always assessed prior to securing the permanent lead and that we consistently placed the lead in the S3 foramen by always finding the S2 foramen and documenting leg rotation with stimulation.
Traditional Test and Permanent Implant
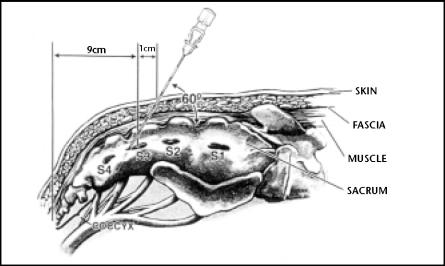
In an outpatient procedure room, patients were placed in the prone position, and the buttocks were taped open to view the anus and perineal area. Bony landmarks were palpated, and the presumed S3 foramen was marked. The skin was prepped and draped, and lidocaine 1% was injected into the skin, subcutaneous tissues, and periosteum. A needle was advanced into the sacral foramen and stimulated with an external generator (Figure 1). Motor and sensory responses were assessed. If good anal bellows and greater toe movement were seen, and the patient felt a comfortable tapping or vibrating sensation in the rectal or vaginal area, this was considered good placement. A temporary lead was advanced through the foramen needle, and the needle was removed. This procedure was then repeated on the opposite side. Each lead was then tested to confirm the motor and sensory responses and secured to the patient’s back with Tegaderm dressings. Sacral x-rays were performed to confirm that the placement was correct. The patients were instructed on how to use the external stimulation box and were restricted from bending, reaching, or showering for the next 5 to 7 days. The patients kept voiding diaries and pain scores and returned to review the results and have the test wires removed.
Figure 1.
Insertion of a foramen needle through the S3 sacral foramen in preparation for testing the motor and sensory responses.
Responders underwent a permanent implant under a general anesthetic in the operating room. Bony landmarks were palpated, and the presumed S3 foramen marked. A large midline sacral incision was made and dissected laterally to the sacral foramen. The dorsolumbar fascia was opened and the spinous muscle spread, exposing the periosteum. A needle was advanced into the sacral foramen, and motor responses were assessed. If adequate anal bellows were achieved, the foramen was dilated with a hemostat, and the permanent lead was advanced directly through the foramen. Each of the 4 stimulation sites on the permanent lead was tested to confirm the motor response, but no sensory response was assessed. The lead was secured to the periosteum using a prolene suture and the attached anchor. The dorsolumbar fascia was closed, and the proximal lead was brought through the fascial incision. A site on the ipsilateral buttock was chosen for the placement of the generator. A transverse skin incision was made, and a subcutaneous pocket was created. The proximal lead was tunneled to this buttock incision, and the generator was connected to the lead in the standard fashion. The incisions were closed, and the patient returned in 2 weeks for the programming of the generator.
Staged Test and Permanent Implantation
For the staged test, patients in the operating room were placed under conscious sedation (with midazolam and propofol) and a local anesthetic, and a permanent lead was placed and used during the test period. Fluoroscopy was employed to mark the midline of the sacrum and the sacral iliac junction. This intersection is the area of the S3 foramen. A mark was made 2 cm lateral and superior to the intersection; this was the skin insertion site for the foramen needle. Lidocaine was instilled in the subcutaneous tissue, and a needle was advanced into the S3 foramen with fluoroscopic guidance. A current was applied to the needle, and the motor response was noted. To be certain of the S3 foramen placement, another needle was always passed superior to the first needle, and a leg rotation was noted that confirmed the S2 interspace. After the S3 foramen placement was confirmed, a small vertical incision was made above and below the needle insertion site and carried down to the dorsolumbar fascia with a sharp dissection. A prolene suture (2-0) was passed through the fascia along each side of the needle. Next, the hub of the needle was removed with wire cutters, and under fluoroscopic control, a 14-gauge angiocath was advanced over the needle and into the foramen (Figure 2). The angiocath sheath was advanced, and the foramen needle and angiocath needle were removed (Figure 3). Next, the permanent lead was advanced through the sheath, and the angiocath was removed (Figure 4). Fluoroscopy was used to confirm that all 4 stimulation points lay beneath the sacral bone plate. Motor responses were then tested with each lead to be certain there were good anal bellows, sacral flattening, and minimal toe movement. The “twist-lock” anchor was advanced over the lead and secured to the fascia with the previously placed prolene sutures.
Figure 2.
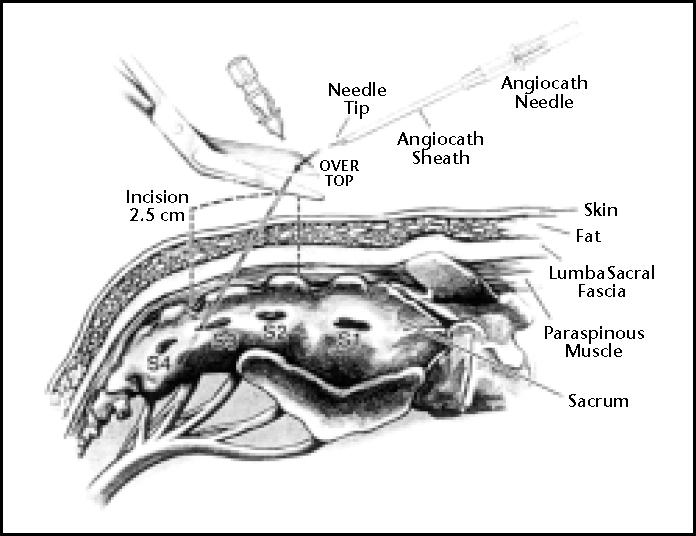
Removal of the hub of the foramen needle and advancement of a 14-gauge angiocath over the needle and into the sacral foramen.
Figure 3.
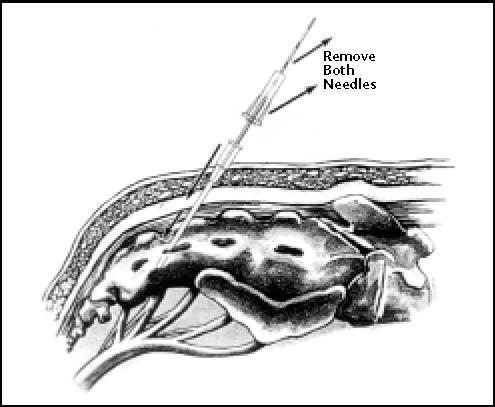
The angiocath sheath is left in the foramen while both the foramen needle and angiocath needle are removed.
Figure 4.
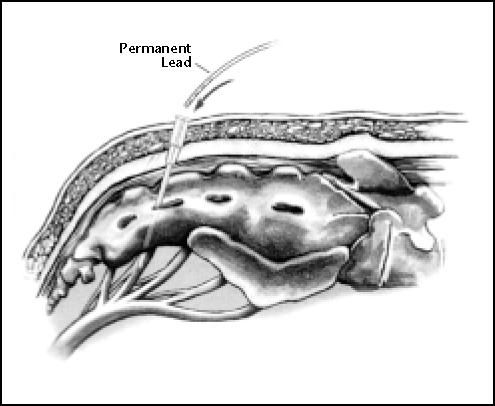
The permanent lead is advanced through the angiocath sheath and below the bone plate. The sheath is then removed, and the lead is secured with the “twist-lock” device after the motor and sensory responses are assessed.
Before the lead was locked in place, the patient was awakened, and the sensory response was assessed with the stimulation of each lead. Adequate sensory response was considered a comfortable stimulation in the rectal, vaginal, or perineal area. If the patient felt pain with stimulation, the lead was adjusted. After a good lead placement was confirmed, the anchor was locked. A site on the ipsilateral upper buttock was chosen where a future permanent generator would be placed if the patient responded to therapy. A small (2 cm) transverse incision was made, and a subcutaneous pocket was created. The proximal end of the lead was then tunneled to this pocket. The permanent lead was then connected to a temporary extension wire, and the distal end of the wire was tunneled to the contralateral upper buttock and externalized (Figure 5).
Figure 5.
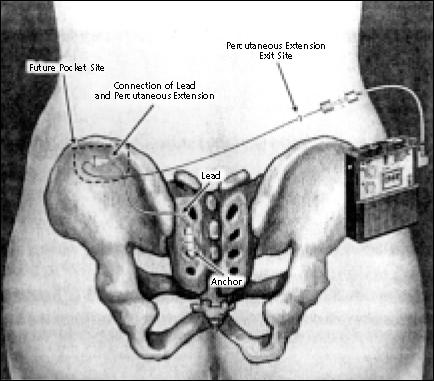
Stage I implant showing the permanent lead secured to the dorsolumbar fascia and the proximal end tunneled to a subcutaneous pocket on the ipsilateral side. The lead is then connected to a temporary extension lead, which is tunneled to the contralateral side and externalized. The external generator is then connected to this extension lead.
The patients were discharged with the standard external programmer, which was worn for 2 weeks. The permanent lead allows for 4 different points of stimulation along the nerve. Using the external programmer, the leads that are on can be adjusted along with the rate, pulse width, and current. The patients monitored their voiding symptoms and pelvic pain. After 2 weeks they returned to the operating room either to have the leads removed if they did not respond or to have a permanent generator implanted. The generator was placed by extending the incision in the upper buttocks, creating a larger subcutaneous pocket, removing the temporary extension lead, connecting the generator, and closing the incision (Figure 6). Before the patient leaves the operating room, the implanted generator can be programmed to the identical settings that the patient responded to with the external generator, and stimulation is initiated.
Figure 6.
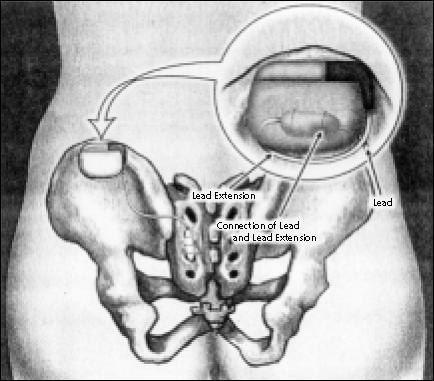
Stage II implant showing the extension lead removed, the ipsilateral subcutaneous pocket extended, and the generator placed. The generator is then programmed to the settings that gave a good clinical response during the test phase.
Data Analysis
Descriptive data were determined by a chart review, and clinical data were collected prospectively with questionnaires and voiding diaries. A statistical analysis was generated by the paired t test and supported by the Wilcoxon signed rank test (nonparametric). Significance was set at P < 0.05.
Outcomes of the Traditional Test
A total of 21 patients with refractory IC underwent a traditional percutaneous test. Of the 21 patients, 14 (67%) had a positive response. Further, 11 of the 14 responders (79%) elected to have a permanent implant placed, resulting in a test-to-implant rate of 52% (11 out of 21 patients tested).
Of the 11 patients who chose to have a permanent implant after the traditional test, 7 underwent a traditional permanent implantation under a general anesthetic without having the sensory response assessed. A reoperation was required in 3 out of the 7 patients (43%). Two patients required a lead adjustment because of sensory discomfort, and 1 needed a revision of the generator pocket. The remaining 4 patients had their permanent implants placed when they were under conscious sedation, and the sensory response was determined before securing the permanent lead. No reoperations were required in this group of 4 patients.
Outcomes of the Staged Test
Twelve refractory IC patients underwent a staged implant, using the permanent lead that was placed in the patients under conscious sedation during the test period. The sensory response was assessed prior to securing and externalizing the lead. Of the 12 patients tested, 11 (92%) had a positive response, and all 11 of these responders (100%) elected to undergo generator placement, resulting in a test-to-implant rate of 92%. No reoperations were required in this group.
Outcomes of the Permanent Implant
A total of 22 patients with refractory IC (11 from the traditional test group and 11 from the staged test group) underwent a permanent implantation of an Interstim device. The mean age of the patients was 45.5 years (range, 17–68 years of age ); 23% were male and 77% were female. All patients had undergone a cystoscopy with hydrodistension and demonstrated glomerulations. The mean bladder capacity was 710 cc, and 18% had Hunner’s ulcers. The patients on average had failed 6 previous IC treatments prior to the Interstim testing. Questionnaires were sent to all patients who had a permanent implant, and 21 (95%) of the 22 questionnaires were returned. The mean follow-up time from the implant was 5.2 months.
The overall improvement in IC symptoms was 56%. As many as 95% of the patients reported that they would undergo the implant again and would recommend the therapy to a friend. Significant improvements were seen in the number of day voids (44%) and nocturia (55%) (Table 1).
Table 1.
Change in the Number of Voids in IC Patients After Implantation of a Neuroprosthetic Device (Interstim)
| Baseline | Postimplant | % Change | P-Value | |
|---|---|---|---|---|
| Day voids (n) | 19.0 | 10.5 | 44% | <.001 |
| Nocturia (n) | 5.6 | 2.5 | 56% | <.001 |
| 24-hour voids (n) | 25.0 | 13.0 | 48% | <.001 |
The patients were asked to rate various symptoms associated with IC since they had the stimulator placed as markedly worse, moderately worse, slightly worse, the same, slightly improved, moderately improved, or markedly improved. A response of moderately or markedly improved was considered a positive response (>50% improvement). The majority of patients reported at least a 50% improvement in frequency (71%), urgency (62%), pelvic pain (65%), pelvic pressure (80%), quality of life (72%), incontinence (69%), and vaginal pain (54%) (Table 2). No patients showed >50% worsening in any symptom. The overall reoperation rate was 3 (13.6%) out of 22 patients, and there have been no reoperations since the permanent lead was placed under conscious sedation and the sensory response was assessed. No infections or explantations have occurred.
Table 2.
Percentage of Patients with IC with at Least a 50% Improvement in Symptoms (Positive Response) After Implantation of a Neuroprosthetic Device (Interstim)
| Moderately | Markedly | Total | |
|---|---|---|---|
| Improved | Improved | Positive Response | |
| Urinary frequency | 38% | 33% | 71% |
| Urinary urgency | 38% | 24% | 62% |
| Pelvic pain | 35% | 30% | 65% |
| Pelvic pressure | 40% | 40% | 80% |
| Quality of life | 34% | 38% | 72% |
| Incontinence | 38% | 31% | 69% |
| Bowel movements | 34% | 5% | 39% |
| Vaginal pain | 31% | 23% | 54% |
Study Discussion: Traditional Versus Staged Procedures
Sacral nerve modulation has been shown to be effective in the treatment of urinary urgency and frequency, urge incontinence, and nonobstructive urinary retention. Because of this relationship, we hypothesized that this therapy might also be effective in the treatment of IC, which is often refractory to standard therapies. Many patients with IC can be managed with multimodality therapy, including behavioral, dietary, and oral or intravesical pharmaceuticals. Unfortunately, no therapy has been shown to be consistently effective in treating severe IC. Therefore, many patients remain refractory to treatment, and they rely on high doses of narcotics to manage their pain.
The results of our study show that sacral nerve modulation appears to be effective in treating refractory IC. The response to therapy, however, is dependent on the technique used to test the efficacy. In this study, the traditional percutaneous test resulted in a 67% positive response rate and a test-to-implant rate of only 52%. In contrast, a staged test resulted in a 92% positive response rate, and all responders went on to receive a permanent implantation.
Several reasons are likely to account for the difference in response to the two tests. First, the traditional test was performed with a lead that had a single point of stimulation at its distal end compared to the staged test that used the permanent lead that has 4 different stimulation sites along its length. Each of these stimulation points or a combination of all can be tested. Second, the traditional lead was taped to the skin surface and had a greater likelihood of migrating during the test period compared to the staged lead, which is secured to the dorsolumbar fascia with suture. Third, the time period for the traditional test was only 5–7 days because of the difficulty in limiting activity, preventing lead migration, and imposing significant restrictions, such as no showering. The staged test lasted up to 14 days, allowing for more time to assess the response to therapy and to adjust the programming.
Reoperations occurred only in patients who had a traditional permanent implant after a successful percutaneous test. Several factors led to poorer outcomes. First, the implant was placed under a general anesthetic, without the benefit of fluoroscopy and sensory input during the lead placement. The group that had an implant placed under a general anesthetic had a 43% reoperation rate compared to a 0% rate among those who had the lead placed under sedation and a sensory input assessment. Fluoroscopy can help assure that the lead is placed in the S3 foramen, and this can be confirmed by always finding and testing the S2 nerve root. Second, the electrode placed during a traditional test is removed, and a permanent electrode is put in place during future surgery. It is difficult to be certain whether the permanent electrode is in an area that will give as good a response as that in the previous test. In contrast, the staged procedure uses the permanent electrode during the test period. Thus, once a positive response is found, the lead is never moved, and the sensory and motor responses continue as before, once the generator is placed. Third, patients who responded to a traditional test often had to wait weeks before a permanent implant could be placed and then several weeks until programming was performed. This created a hardship in those who had a significant clinical response to the test lead. During a staged test, however, the responder has a generator put in place 2 weeks after the implantation of the lead, and the settings found on the external generator test box can be programmed into the implantable generator and stimulation continued without interruption in therapy.
Conclusions
Our study found that sacral nerve modulation is effective in treating patients with refractory IC. The IC patients who had a permanent implant had been refractory to an average of six previous therapies. However, this challenging patient population responded well to sacral nerve modulation. The quality of life significantly improved, and 95% of the IC subjects stated that they would undergo an implant again.
The improvement in severe IC symptoms resulting from sacral nerve modulation gives us an insight into the pathophysiology of the disease. What might start as a primary bladder disease can progress into abnormal upregulation of the sacral nerve and lead to pelvic-floor dysfunction, which can affect the bladder, rectum, and genitalia. If electric stimulation overrides the abnormal signals coming from the nervous system, the underlying dysfunction might be corrected. The staged procedure in our study yielded a greater response rate and a lower reoperation rate than the traditional percutaneous test procedure did. Therapy with a neuroprosthetic device should be in the urologists’ armamentarium to offer relief to those suffering from voiding dysfunction.
Main Points.
Interstitial cystitis (IC) is a symptom complex of urinary urgency, frequency, and pelvic pain, and although many patients with IC will respond to multimodality treatment, a subset of IC patients remains refractory to all standard therapies.
The current study assessed the efficacy of sacral nerve modulation in treating patients with severe refractory IC. Two distinct procedures were used for the initial test and the permanent implantation of a neuroprosthetic device: a traditional test and a staged test followed by the implantation.
After the placement of a permanent stimulator, the majority of patients reported >50% improvement in frequency, urgency, pelvic pain, and quality of life.
The study found that sacral nerve modulation is effective in treating patients with refractory IC, depending on the technique used to test the efficacy. Compared with the traditional test, the staged test resulted in a significantly higher positive response rate and in the number of responders who received a permanent implantation.
References
- 1.Baskin LS, Tanagho EA. Pelvic pain without pelvic organs. J Urol. 1992;147:683–686. doi: 10.1016/s0022-5347(17)37348-2. [DOI] [PubMed] [Google Scholar]
- 2.Fall M, Carlsson CA, Erlandson BE. Electrical stimulation in interstitial cystitis. J Urol. 1980;123:192–195. doi: 10.1016/s0022-5347(17)55850-4. [DOI] [PubMed] [Google Scholar]
- 3.Geirsson G, Wang YH, Lindstrom S, Fall M. Traditional acupuncture and electrical stimulation of the posterior tibial nerve: a trial in chronic interstitial cystitis. Scand J Urol Nephrol. 1993;27:67–70. doi: 10.3109/00365599309180416. [DOI] [PubMed] [Google Scholar]
- 4.Fall M. Transcutaneous electrical nerve stimulation in interstitial cystitis: update in clinical experience. Urology. 1987;29(4 suppl):40–42. [PubMed] [Google Scholar]
- 5.Everaert K, Devulder J, De Muynck M, et al. The pain cycle: implications for the diagnosis and treatment of pelvic pain syndromes. Int Urogynecol J. 2001;12:9–14. doi: 10.1007/s001920170087. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt RA, Bruschini H, Tanagho EA. Urinary bladder and sphincter responses to stimulation of dorsal and ventral sacral roots. Invest Urol. 1979;16:300–304. [PubMed] [Google Scholar]
- 7.Schmidt RA, Tanagho EA. Feasibility of controlled micturation through electrical stimulation. Urol Int. 1979;34:199–230. doi: 10.1159/000280267. [DOI] [PubMed] [Google Scholar]
- 8.Chai TC, Zhang C, Warren JW, Keay S. Percutaneous sacral third nerve root neurostimulation improves symptoms and normalizes urinary HB-EGF levels and antiproliferative activity in patients with interstitial cystitis. Urology. 2000;55:643–646. doi: 10.1016/s0090-4295(00)00476-3. [DOI] [PubMed] [Google Scholar]
- 9.Maher CF, Carey MP, Dwyer PL, Schluter PL. Percutaneous sacral nerve root neuromodulation for intractable interstitial cystitis. J Urol. 2001;165:884–886. [PubMed] [Google Scholar]
- 10.Siegel S, Paszkiewicz E, Kirkpatrick C, et al. Sacral nerve stimulation in patients with chronic intractable pelvic pain. J Urol. 2001;166:1742–1745. [PubMed] [Google Scholar]
- 11.Thon WF, Baskin LS, Jonas U, et al. Neuromodulation of voiding dysfunction and pelvic pain. World J Urol. 1991;9:138–141. [Google Scholar]
- 12.Siegel SW. Management of voiding dysfunction with an implantable neuroprosthesis. Urol Clin North Am. 1992;19:163–170. [PubMed] [Google Scholar]
- 13.Janknegt RA, Weil EHJ, Eerdmans PHA. Improving neuromodulation for refractroy voiding dysfunctions: two-stage implant. Urology. 1997;49:358–362. doi: 10.1016/S0090-4295(96)00506-7. [DOI] [PubMed] [Google Scholar]
- 14.Chai TC, Mamo GJ. Modified techniques of S3 foramen localization and lead implantation in S3 neuromodulation. Urology. 2001;58:786–790. doi: 10.1016/s0090-4295(01)01326-7. [DOI] [PubMed] [Google Scholar]