Abstract
Nonpharmacologic treatment for erectile dysfunction (ED) includes sex therapy, the use of vacuum erection devices, penile prosthesis implantation, and penile vascular surgery. Sex therapy is indicated for psychogenic ED and is at times a useful adjunct for other treatments in men with mixed psychogenic and organic ED. Vacuum erection devices produce usable erections in over 90% of patients; however, patient and partner acceptability is an issue. Three-piece inflatable penile prostheses create flaccidity and an erection that comes close to that which occurs naturally. Penile vascular surgery has shown greatest efficacy in young men with vasculogenic ED resulting from pelvic or perineal trauma.
Key words: Impotence, Sex therapy, Vacuum erection device, Penile prosthesis, Penile vascular surgery
Today, the man with erectile dysfunction (ED) has available to him a wider variety of treatment options than ever before. For nearly all of these men, a trial with a systemic agent such as sildenafil citrate will be the first option chosen. If this fails or is contraindicated, other pharmacologic treatments such as penile injections or intraurethral medication are available but are less attractive than systemic therapy and may either prove ineffective or be rejected. This review will discuss the remaining, nonpharmacologic treatments for ED. They include sex therapy, the use of vacuum erection devices, penile prosthesis implantation, and penile vascular surgery.
Sex Therapy
Psychogenic ED was defined by the International Society of Sex and Impotence Research as the persistent inability to achieve or maintain an erection satisfactory for sexual performance, owing predominantly or exclusively to psychologic or interpersonal factors.1 This broad disorder has been subdivided according to immediate and remote causes. Immediate causes include performance anxiety, lack of adequate stimulation, and relationship conflicts. Remote causes include childhood sexual trauma, sexual identity issues, unresolved partner or parental attachments, and religious or cultural taboos.2
Rosen2 divided treatment for psychogenic ED into four types: anxiety reduction and desensitization, cognitive-behavioral interventions, increased sexual stimulation, and interpersonal assertiveness and couples’ communication training. The first treatment type, anxiety reduction and desensitization, is designed to reduce performance anxiety by avoiding intercourse in early treatment and using relaxation techniques. Instead of having coitus, the couple follows a series of nongenital, nondemand, sensate focus exercises popularized by Masters and Johnson.3 In cognitive-behavorial interventions, attempts are made to dispel sexual ignorance and to overcome unrealistic sexual expectations. Increased sexual stimulation may be necessary for the older male to attain and maintain an erection. Giving the couple this knowledge and providing permission for the partner to become more actively involved is frequently helpful. Finally, through interpersonal and systemic interventions, issues concerning status and dominance, intimacy and trust, and loss of sexual attraction may be addressed.2
Sex therapy by itself may resolve psychogenic ED, and because psychological factors are so often significant contributors to all types of organic ED, some form of sex therapy or counseling as an adjunct to pharmacologic and other nonpharmacologic treatment for organic ED is often helpful.
Vacuum Erection Device Therapy
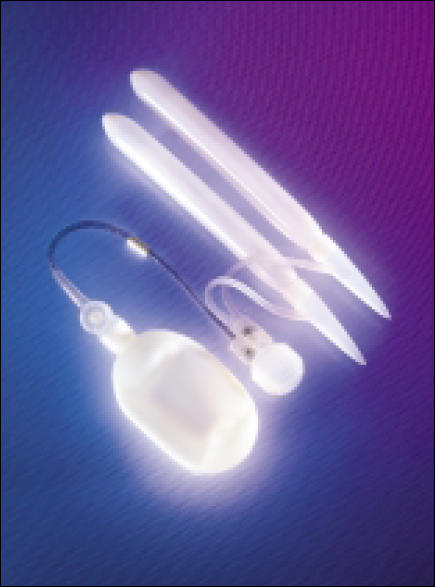
Vacuum erection devices have been commercially available since the early 1980s. These devices have three components: a vacuum cylinder, a pump to create a controlled negative pressure or vacuum, and one or more constriction rings (Figure 1). The constriction ring or rings are placed on the open end of the cylinder that has been coated with a water-soluble lubricant. The cylinder is then placed over the penis that has also been coated with the lubricant. The pump, which may be either manually or battery operated, depending on the model, is activated to create a controlled vacuum. Once engorgement of the penile tissues is obtained, 1 or more rings or tension bands are displaced onto the base of the penis. The cylinder is removed, and the man has intercourse with the rings remaining in place to maintain the erection-like state. The rings should be left on for no longer than 30 minutes.
Figure 1.

The Osbon ErecAid® Esteem™ system vacuum erection device. Image provided by Timm Medical Technologies and reprinted with permission.
Adverse Effects of Vacuum Erection Therapy
Nadig and colleagues4 studied the effects of a vacuum erection device in 35 men with organic ED. They found that blood flow into the penis decreased while the tension band was in place, and the penile skin temperature decreased by about 1 degree C. Congestion and cyanosis of the extra corporeal tissue occurred, and the superficial veins were distended. This resulted in a larger than normal penile circumference (4.3 cm mean with the device compared to 2.8 cm mean with a normal erection). Penile rigidity occurred only distal to the band, and thus the erection pivoted at the base of the penis.
Levine and Dimitriou5 reported that the ejaculate might be trapped in the urethra until the constriction band is released. Moreover, pain may occur during the creation of the suction in 20% to 40 % of users of these devices or on ejaculation in 3% to 16% of cases. Further, the authors reported that petechiae or bruising occurred in 25% to 39% and in 6% to 20% of users, respectively.
Broderick and associates6 used color duplex ultrasonography to study the hemodynamics of vacuum constriction erections. Their data showed that the erectile state distal to the vacuum constriction device band was one of low arterial flow.
Satisfaction with Vacuum Erection Device
In spite of these adverse effects, an erection-like state satisfactory for coitus was obtained by over 90% of users.5 Of those who elected to use the device, 69% reported continued use for at least 2 years.7 In a retrospective study, Sidi and colleagues8 looked at patient satisfaction with the vacuum erection device in a group of 100 men. The overall satisfaction rate was 68%. Pain, inconvenience, and premature loss of rigidity were cited as reasons for dissatisfaction.
In another study of 50 men with corporeal venous occlusive dysfunction, who were treated with a vacuum erection device, 38 (76%) were able to achieve a usable erection. Twenty-eight patients (56%) were satisfied, 13 (26%) were dissatisfied, and in 9 (18%) satisfaction with this method of treatment could not be determined.9 Jarow and associates10 showed, however, that when 377 patients were presented with a variety of treatment options for ED, only 12% chose the use of a vacuum erection device.
Contraindications to Vacuum Erection Device Therapy
There are few contraindications to this form of therapy. Patients on anticoagulants and patients with bleeding disorders may use these devices with care.11 Major complications have been reported infrequently. Penile skin necrosis,12,13 Peyronie’s disease,12,14 and Fournier’s gangrene15 are among these.
Penile Prosthesis Implantation
Penile prostheses available now in the United States are classified as noninflatable (Table 1) and inflatable (Table 2). Today, men who elect to have a penile prosthesis implantation generally have high expectations and want to have a device that can alternate between the flaccid and erect states. Furthermore, they would like to have penile flaccidity and erection as similar as possible to that produced by natural mechanisms. Of the available devices, the 3-piece inflatable prostheses with their large-volume abdominal-fluid reservoirs come closest to achieving these goals.
Table 1.
Noninflatable Penile Prostheses
| Prosthesis | Type | Manufacturer |
|---|---|---|
| AMS Malleable 650 | Malleable | American Medical |
| Systems* | ||
| Mentor Malleable | Malleable | Mentor Urology† |
| Mentor Accuform | Malleable | Mentor Urology† |
| Dura-II | Mechanical | Timm Medical |
| Technologies‡ |
American Medical Systems, Minnetonka, MN.
Mentor, Santa Barbara, CA.
Timm Medical Technologies, Eden Prairie, MN.
Table 2.
Inflatable Penile Prostheses
| Prosthesis | Type | Girth Expansion | Length Expansion |
|---|---|---|---|
| AMS Ambicor | 2-piece | No | No |
| AMS 700CX | 3-piece | Yes | No |
| AMS 700CXM | 3-piece | Yes | No |
| AMS Ultrex | 3-piece | Yes | Yes |
| Mentor Mark II | 2-piece | Yes | No |
| Mentor Alpha-1 | 3-piece | Yes | No |
| Mentor Alpha-1 | 3-piece | Yes | No |
| Narrow Back |
Three-piece inflatable devices are usually implanted under general or regional anesthesia. Either an infrapubic or a penoscrotal approach can be chosen. The penoscrotal approach provides easier and more complete corporeal exposure and avoids possible damage, especially during revision surgery, to the sensory dorsal nerves of the penis. Furthermore, the scrotal pump can be anchored with this approach. The only disadvantage to the penoscrotal approach is the need to create by palpation a retropubic space for the reservoir.
Improvements in Penile Prostheses
The Mentor (Santa Barbara, CA) 3-piece, Alpha-1 prosthesis provides girth-expanding cylinders (Figure 2), and American Medical Systems’ (AMS; Minnetonka, MN) 3-piece prosthesis provides both girth-expanding (CX and CXM) and girth-plus-length-expanding (Ultrex) cylinders (Figure 3). After implantation, Ultrex cylinders provide a mean of 2 cm (range, 1 to 5 cm) of length expansion.16 This feature, however, initially proved to function at the expense of increased mechanical failure of the Ultrex cylinders (80%, 5-year Kaplan-Meier survival).17 In 1993, the Ultrex cylinder design was changed, and the middle-layer fabric was tightened. In a study comparing the pre-1993 to the post-1993 Ultrex cylinders, the 5-year actuarial survival, free of mechanical failure, was shown to have increased to 96%.18 Similar studies using Kaplan-Meier survival estimates, which took into account differing lengths of time of follow-up, showed that recent rates of overall survival and survival free of mechanical failure for all components of the Mentor and AMS 3-piece prostheses are high (Table 3 shows post-1993 rates) and are much improved compared to early experiences with these inflatable penile prostheses.19–21
Figure 2.
Mentor Alpha-1® 3-piece inflatable penile prosthesis with Lock-out™ valve reservoir. Image courtesy of Mentor and reprinted with permission.
Figure 3.

AMS Ultrex 3-piece inflatable penile prosthesis. Image courtesy of American Medical Systems and reprinted with permission.
Table 3.
Five-Year Kaplan-Meier Survival Rates for 3-Piece Inflatable Prostheses from 1993 to the Present
| Study | Overall | Freedom from |
|---|---|---|
| Mechanical Failure | ||
| Goldstein et al19* | 75%‡ | |
| Milbank et al20† | 78% | 94% |
| Wilson et al21* | 93% |
Mentor Alpha-1 inflatable penile prosthesis.
AMS Ultrex inflatable penile prosthesis.
Three-year Kaplan-Meier survival rate.
Infected Penile Prostheses
Infection is the most significant complication of penile prosthesis implantation surgery, because almost all infections involving the periprosthetic space require further surgery. Infection rates for penile prosthesis implantations have been reported to vary from 0.6% to 16.7% for nonhydraulic implants, from 3.0% to 8.1% for hydraulic implants, and from 0.8% to 8% for 3-piece inflatable prostheses.22 In the past, all components of infected prostheses were removed, and penile prosthesis reimplantation was often delayed for 6 months to 1 year. During this time, scar tissue, which resulted from infection-related damage to corporeal smooth muscle, underwent maturation and contraction, producing a significantly smaller penis. During subsequent prosthesis reimplantation, this mature scar tissue was very difficult to dilate, and special implant and reconstructive techniques23,24 or the use of a small prosthesis25 were often necessary.
Salvage Procedure
To avoid these problems in prosthesis reimplantation following removal of an infected penile prosthesis, Mulcahy26 popularized the salvage procedure. In this procedure, all components of the infected device are removed, and then the implant space is copiously irrigated with saline, antibiotic solution, half-strength hydrogen peroxide, and half-strength povidone iodine solution. The open wound is then prepped and draped, the surgical team again scrubs and gowns, a new instrument table is brought in, and the new prosthesis is implanted. Using this protocol, Mulcahy showed in 55 cases that 82% of patients were free of infection, with follow-up ranging from 6 to 93 months.
Penile Prostheses for Erectile Deformity
Men who have an erectile deformity as the result of Peyronie’s disease and who also have ED are often most appropriately treated by penile prosthesis implantation and modeling of the penis over inflated cylinders.27 When the AMS 3-piece inflatable prosthesis is chosen for these patients, CX rather than Ultrex cylinders should be selected because CX cylinders produce better straightening of the penis.28
Satisfaction with Penile Prostheses
Numerous studies have been conducted on patient and partner satisfaction following penile prosthesis implantation. In a study of 272 recipients of an AMS 700 inflatable prosthesis, McLaren and Barrett29 reported 83% satisfaction among the recipients, and 70% satisfaction among their partners. Holloway and Farah30 reported 85% patient and 76% partner satisfaction among 145 AMS Ultrex recipients. Goldstein and colleagues31 found that 82% of 96 recipients of a Mentor Alpha-1 prosthesis experienced fulfilled expectations with this method of treatment for their ED. Beutler and associates32 found increased satisfaction in men using an inflatable penile prosthesis compared to men receiving a noninflatable penile prosthesis, and, in another study, they showed greater satisfaction among female partners of men using inflatable compared to noninflatable prostheses.33
In a prospective study of 35 penile prosthesis recipients, a 13-item psychosexual questionnaire, with items rated on a 1 to 5 scale, was administered preoperatively and at 3, 6, and 12 months postoperatively. Significant improvements in erectile ability and libido were noted, along with increased satisfaction with sexual life. There were decreases in feelings of sadness, anxiety, anger, frustration, and embarrassment related to sexual activity. These changes, relative to preoperative levels, peaked at 6 months and were maintained at 1 year.34 In another study comparing 115 men on penile injection therapy to 65 recipients of a penile prosthesis, after a mean follow-up of 5.4 years, 70% of the penile prosthesis recipients were still sexually active compared to only 41% of the penile injection patients.35
Penile Vascular Surgery
Penile vascular surgery consists of penile venous ligation procedures and penile arterial revascularization. Penile venous ligation to treat ED was originally proposed by Duncan36 in 1895 and performed by Wooten37 in 1902 and by Lydston38 in 1908. These investigators obtained short-lived improvement in erectile function; however, the procedures described by them did not achieve widespread popularity. Venous ligation again emerged in the mid 1980s,39 and for a period of time enjoyed reasonable popularity. In an effort to increase success rates and to make success more durable, the initial procedure of dorsal vein ligation was expanded to include circumflex and emissary vein ligation as well as cavernous and crural vein ligation.40 Crural ligation has also been proposed in an attempt to broaden success with these procedures.41 Bookstein and Lurie42 proposed venous embolization as an alternative to surgery.
In carefully selected patients, short-term success rates were shown to be reasonable (23%–80% within the first year), but decreased with a longer follow-up (14%–77% after 1 year).43 Late failures are probably caused by the development of collateral veins and because venous ligation does not address the primary source of this disorder, which is probably associated with corporeal smooth-muscle disease and neurotransmitter deficiencies.44 Also, diagnostic techniques for patients who might benefit from these procedures have not been validated with normal controls, and many men who have psychogenic ED may have had these operations performed.45,46 The popularity of penile venous ligation procedures as treatment for ED has fallen off significantly during the past several years, primarily as the result of poor long-term results.43
Penile Arterial Revascularization
Vascular disease is common as men age and is probably the leading cause of organic ED in men over the age of 50. The popularity of coronary arterial bypass grafts in the treatment of coronary artery disease suggested that similar procedures might be successful in restoring normal erectile function in men suffering from vasculogenic ED. Michal and colleagues47 reported the first penile arterial revascularization, in 1973, with direct anastomosis of the inferior epigastric artery to the corpus cavernosum. This procedure produced short-term success; however, fibrosis of the cavernous smooth muscle exposed to direct arterial inflow occurred and led to bypass thrombosis.
In what became known as the Michal II procedure, the inferior epigastric artery was anastomosed in an end-to-side fashion to the dorsal penile artery that, like the cavernous artery, arises from the common penile artery and shares numerous collaterals.48 Virag and associates49 described a procedure in which the inferior epigastric artery was anastomosed directly to the deep dorsal vein. Numerous other investigators have described various modifications of these basic procedures.
Controversy still exists regarding the long-term effectiveness of penile arterial revascularization procedures in their various forms, and they do not have widespread acceptance, especially in the United States. In his presidential address to the International Society of Impotence Research in 1990, Sharlip50 expressed his skepticism concerning some claims from proponents of this surgery. After doing a meta-analysis of literature reports, the American Urological Association’s Clinical Guidelines Panel, in 1996, declared that neither arterial nor venous surgery for ED was justified to be performed routinely, especially in older patients with vascular disease.51 Arterial revascularization procedures appear to have the greatest potential efficacy in young men with ED secondary to arterial injury from pelvic or perineal trauma.44,52
Main Points.
Currently available options to treat men with erectile dysfunction (ED) range widely from pharmacologic treatments such as oral agents, penile injections, and intraurethral medications to nonpharmacologic treatments including sex therapy, vacuum erection devices, penile prosthesis implantation, and penile vascular surgery.
Sex therapy may alone resolve psychogenic ED and can be an important adjunct to other treatments for ED of organic and mixed organic/psychogenic origin.
Vacuum erection devices may have significant adverse effects and questionable acceptability, but studies show that they result in erections satisfactory for intercourse in a high percentage of users.
Penile prostheses are available in inflatable and noninflatable forms that approximate the action of a naturally occurring erection. Three-piece inflatable penile prostheses have improved significantly in design over the last decade, and studies have reported high rates of satisfaction among users and their partners.
Penile vascular surgery has shown reasonable success within the first year after surgery, but late failures occur. The procedure appears to be most efficacious in young men with ED resulting from pelvic or perineal trauma.
Summary of Discussion Following Dr. Montague’s Presentation
Dr. Montague summarized the main points of his presentation as follows: First, obviously systemic therapy has revolutionized the treatment of ED. But there will always be a need for nonpharmacologic treatments. Systemic therapy is never going to work in every individual. Second, sex therapy is important. It is still the treatment of choice for some people with pure psychogenic ED (and that does exist), and sex therapy has a potential to cure that. In addition, sex therapy can be a useful adjunct to almost any other treatment for ED, since even organic dysfunction is almost always accompanied by a psychogenic component. Finally, penile prosthesis surgery is probably the only treatment that is potentially applicable to any man. In men with fibrosis of the corpora it is difficult to implant, but it can be done. For these men it is the only treatment available.
Dr. McCullough mentioned his observation that as a mentor for family practice residents in sexual health, many young family practitioners, who trained after the approval of sildenafil, think that injection therapy, MUSE®, and penile implants are archaic and are of historical interest only. Urologists have to make sure, McCullough continued, that the message is sent that there are good nonpharmacologic treatments for ED, and that there are urologists and mental health professionals who treat ED quite satisfactorily with these other treatments. There has to be an on-going education process for the PCPs who are now diagnosing and treating over two thirds of ED patients. Unless this education occurs, urologists may find themselves doing no implants.
Dr. Carson agreed, pointing out that not only do the other treatments exist, but the satisfaction rates with them are high. There are a number of studies now that have looked at prosthesis outcomes very carefully, Carson said, and the outcomes are very good. Mechanically, no longer are we replacing 30% of these prostheses in 2 or 3 years. Many of them are lasting a decade and a half or longer. The patient and the partner satisfaction rates are well in excess of 80%, and in many studies in excess of 90%.
Dr. Steers asked whether most of the implants today were replacements of failed devices. Montague replied that there has been an increase in de novo implants but the replacement of failing devices is very successful. If a patient has been satisfied with an implant and it has failed mechanically, he said, he almost never does a revision. “Instead, we remove the entire failed device and replace it with a brand new one.” Another issue with revision surgery is that infection rates have been higher than with primary implantation. Montague believes that infection rates can be lower if the urologist removes the entire original device and copiously irrigates all the prosthesis compartments, much like Mulcahy described with infected prostheses.
Dr. Sadovsky returned to the issue of physicians thinking that prosthesis implantation is an archaic technique. That belief is in part due to the fact that physicians do not know who is doing implantation and who does it well. “We just don’t know,” he said, “who is doing it in our region.” It might be interesting for the AUA, some other organization, or some publication to make a list of the centers that are proficient in implant surgery and make that information more widely available, so the physicians know to whom to send their patients.
Dr. Montague brought up the subject of ED as a progressive disorder. Even those patients who initially respond to oral therapy may, as their disease progresses, eventually stop responding. “In other presentations and publications,” Montague said, “I draw the parallel between the treatment of osteoarthritis and the treatment of ED.” There are millions of patients on NSAIDs to treat an age-related disorder, osteoarthritis. Many patients are satisfactorily managed with oral NSAID therapy for a period of time, and then their disease progresses. When that occurs, they move on to joint injections, arthroscopic surgery, and then, finally, hip or knee implant surgery, for their debilitating but not life-threatening osteoarthritis. “Implant surgery for osteoarthritis is a big business in the United States,” he concluded. “I think that this is what’s going to happen with ED.”
References
- 1.Lizza EF, Rosen RC. Definition and classification of erectile dysfunction: report of the Nomenclature Committee of the International Society of Impotence Research. Int J Impot Res. 1999;11:141–143. doi: 10.1038/sj.ijir.3900396. [DOI] [PubMed] [Google Scholar]
- 2.Rosen RC. Psychogenic erectile dysfunction: classification and management. Urol Clin North Am. 2001;28:269–278. doi: 10.1016/s0094-0143(05)70137-3. [DOI] [PubMed] [Google Scholar]
- 3.Masters WH, Johnson VE. Human Sexual Inadequacy. Boston: Little, Brown, & Co; 1970. [Google Scholar]
- 4.Nadig PW, Ware JC, Blumoff R. Noninvasive device to produce and maintain an erectionlike state. Urology. 1986;27:126–131. doi: 10.1016/0090-4295(86)90368-7. [DOI] [PubMed] [Google Scholar]
- 5.Levine LA, Dimitriou RJ. Vacuum constriction and external erection devices in erectile dysfunction. Urol Clin North Am. 2001;28:335–341. doi: 10.1016/s0094-0143(05)70142-7. [DOI] [PubMed] [Google Scholar]
- 6.Broderick GA, McGahan JP, Stone AR, White RD. The hemodynamics of vacuum constriction erections: assessment by color Doppler ultrasound. J Urol. 1992;147:57–61. doi: 10.1016/s0022-5347(17)37132-x. [DOI] [PubMed] [Google Scholar]
- 7.Cookson MS, Nadig PW. Long-term results with vacuum constriction device. J Urol. 1993;149:290–294. doi: 10.1016/s0022-5347(17)36059-7. [DOI] [PubMed] [Google Scholar]
- 8.Sidi AA, Becher EF, Zhang G, Lewis JH. Patient acceptance of and satisfaction with an external negative pressure device for impotence. J Urol. 1990;144:1154–1156. doi: 10.1016/s0022-5347(17)39679-9. [DOI] [PubMed] [Google Scholar]
- 9.Kolettis PN, Lakin MM, Montague DK, et al. Efficacy of the vacuum constriction device in patients with corporeal venous occlusive dysfuntion. Urology. 1995;46:856–858. doi: 10.1016/S0090-4295(99)80357-4. [DOI] [PubMed] [Google Scholar]
- 10.Jarow JP, Nana-Sinkam P, Sabbagh M, Eskew A. Outcome analysis of goal directed therapy for impotence. J Urol. 1996;155:1609–1612. [PubMed] [Google Scholar]
- 11.Limoge JP, Olins E, Henderson D, Donatucci CF. Minimally invasive therapies in the treatment of erectile dysfunction in anticoagulated cases: a study of satisfaction and safety. J Urol. 1996;155:1277–1279. doi: 10.1016/s0022-5347(01)66241-4. [DOI] [PubMed] [Google Scholar]
- 12.Ganem JP, Lucey DT, Janosko EO, Carson C. Unusual complications of the vacuum erection device. Urology. 1998;51:627–631. doi: 10.1016/s0090-4295(97)00706-1. [DOI] [PubMed] [Google Scholar]
- 13.Meinhardt W, Kropman RF, Lycklama a Nijeholt AA, Zwartendijk J. Skin necrosis caused by use of negative pressure device for erectile impotence. J Urol. 1990;144:983. doi: 10.1016/s0022-5347(17)39640-4. [DOI] [PubMed] [Google Scholar]
- 14.Kim JH, Carson CC., III Development of Peyronie’s disease with the use of a vacuum constriction device. J Urol. 1993;149(5 Pt 2):1314–1315. doi: 10.1016/s0022-5347(17)36378-4. [DOI] [PubMed] [Google Scholar]
- 15.Theiss M, Hofmockel G, Frohmuller HG. Fournier’s gangrene in a patient with erectile dysfunction following use of a mechanical erection aid device. J Urol. 1995;153:1921–1922. [PubMed] [Google Scholar]
- 16.Montague DK, Lakin MM. Early experience with the controlled girth and length expanding cylinder of the AMS Ultrex penile prosthesis. J Urol. 1992;148:1444–1446. doi: 10.1016/s0022-5347(17)36933-1. [DOI] [PubMed] [Google Scholar]
- 17.Daitch JA, Angermeier KW, Lakin MM, et al. Long-term mechanical reliability of AMS 700 series inflatable penile prostheses: comparison of CX/CXM and Ultrex cylinders. J Urol. 1997;158:1400–1402. [PubMed] [Google Scholar]
- 18.Milbank AJ, Montague DK, Angermeier KW, et al. Mechanical failure with the AMS Ultrex IPP: pre- and post-1993 structural modification. Int J Impot Res. 2001;13(suppl 5):S65. [Google Scholar]
- 19.Goldstein I, Newman L, Baum N, et al. Safety and efficacy outcome of mentor alpha-1 inflatable penile prosthesis implantation for impotence treatment. J Urol. 1997;157:833–839. [PubMed] [Google Scholar]
- 20.Milbank AJ, Montague DK, Angermeier KW, et al. Mechanical failure with the AMS Ultrex IPP: pre- and post-1993 structural modification. Presented at: Meeting of the Sexual Medicine Society of North America; December 7–9, 2001; Charleston, SC. [Google Scholar]
- 21.Wilson SK, Cleves MA, Delk JR., II Comparison of mechanical reliability of original and enhanced Mentor Alpha I penile prosthesis. J Urol. 1999;162(3 Pt 1):715–718. doi: 10.1097/00005392-199909010-00022. [DOI] [PubMed] [Google Scholar]
- 22.Moul JW, Carson CC. Infectious complications of penile prostheses. Infect Urol. 1989;2:97–108. [Google Scholar]
- 23.Herschorn S, Ordorica RC. Penile prosthesis insertion with corporeal reconstruction with synthetic vascular graft material. J Urol. 1995;154:80–84. [PubMed] [Google Scholar]
- 24.Rajpurkar A, Li H, Dhabuwala CB. Penile implant success in patients with corporal fibrosis using multiple incisions and minimal scar tissue excision. Urology. 1999;54:145–147. doi: 10.1016/s0090-4295(99)00060-6. [DOI] [PubMed] [Google Scholar]
- 25.Carbone DJ, Jr, Daitch JA, Angermeier KW, et al. Management of severe corporeal fibrosis with implantation of prosthesis via a transverse scrotal approach. J Urol. 1998;159:125–127. doi: 10.1016/s0022-5347(01)64033-3. [DOI] [PubMed] [Google Scholar]
- 26.Mulcahy JJ. Long-term experience with salvage of infected penile implants. J Urol. 2000;163:481–482. [PubMed] [Google Scholar]
- 27.Wilson SK, Delk JR., II A new treatment for Peyronie’s disease: modeling the penis over an inflatable penile prosthesis. J Urol. 1994;152:1121–1123. doi: 10.1016/s0022-5347(17)32519-3. [DOI] [PubMed] [Google Scholar]
- 28.Montague DK, Angermeier KW, Lakin MM, Ingleright BJ. AMS 3-piece inflatable penile prosthesis implantation in men with Peyronie’s disease: comparison of CX and Ultrex cylinders. J Urol. 1996;156:1633–1635. [PubMed] [Google Scholar]
- 29.McLaren RH, Barrett DM. Patient and partner satisfaction with the AMS 700 penile prosthesis. J Urol. 1992;147:62–65. doi: 10.1016/s0022-5347(17)37134-3. [DOI] [PubMed] [Google Scholar]
- 30.Holloway FB, Farah RN. Intermediate term assessment of the reliability, function and patient satisfaction with the AMS700 Ultrex penile prosthesis. J Urol. 1997;157:1687–1691. [PubMed] [Google Scholar]
- 31.Goldstein I, Bertero EB, Kaufman JM, et al. Early experience with the first pre-connected 3-piece inflatable penile prosthesis: the Mentor Alpha-1. J Urol. 1993;150:1814–1818. doi: 10.1016/s0022-5347(17)35903-7. [DOI] [PubMed] [Google Scholar]
- 32.Beutler LE, Scott FB, Rogers RR, Jr, et al. Inflatable and noninflatable penile prostheses: comparative follow-up evaluation. Urology. 1986;27:136–143. doi: 10.1016/0090-4295(86)90370-5. [DOI] [PubMed] [Google Scholar]
- 33.Beutler LE, Scott FB, Karacan I, et al. Women’s satisfaction with partners’ penile implant. Inflatable vs noninflatable prosthesis. Urology. 1984;24:552–558. doi: 10.1016/0090-4295(84)90100-6. [DOI] [PubMed] [Google Scholar]
- 34.Tefilli MV, Dubocq F, Rajpurkar A, et al. Assessment of psychosexual adjustment after insertion of inflatable penile prosthesis. Urology. 1998;52:1106–1112. doi: 10.1016/s0090-4295(98)00362-8. [DOI] [PubMed] [Google Scholar]
- 35.Sexton WJ, Benedict JF, Jarow JP. Comparison of long-term outcomes of penile prostheses and intracavernosal injection therapy. J Urol. 1998;159:811–815. [PubMed] [Google Scholar]
- 36.Duncan JA. Old age-a myth. Toledo Medical Surgical Reporter. 1895;3:163. [Google Scholar]
- 37.Wooten JS. Ligation of the dorsal vein of the penis as a cure for atonic impotence. Tex Med J. 1902;18:325–328. [PMC free article] [PubMed] [Google Scholar]
- 38.Lydston GF. The surgical treatment of impotence. Am J Med. 1908;15:1571-. [Google Scholar]
- 39.Wespes E, Schulman CC. Venous leakage: surgical treatment of a curable cause of impotence. J Urol. 1985;133:796–798. doi: 10.1016/s0022-5347(17)49231-7. [DOI] [PubMed] [Google Scholar]
- 40.Lue TF. Penile venous surgery. Urol Clin North Am. 1989;16:607–611. [PubMed] [Google Scholar]
- 41.Bar-Moshe O, Vandendris M. Treatment of impotence due to perineal venous leakage by ligation of crura penis. J Urol. 1988;139:1217–1219. doi: 10.1016/s0022-5347(17)42865-5. [DOI] [PubMed] [Google Scholar]
- 42.Bookstein JJ, Lurie AL. Transluminal penile venoablation for impotence: a progress report. Cardiovasc Interven Radiol. 1988;11:253–260. doi: 10.1007/BF02577012. [DOI] [PubMed] [Google Scholar]
- 43.Rao DS, Donatucci CF. Vasculogenic impotence: arterial and venous surgery. Urol Clin North Am. 2001;28:309–319. doi: 10.1016/s0094-0143(05)70140-3. [DOI] [PubMed] [Google Scholar]
- 44.Hwang TI, Yang CR. Penile vein ligation for venogenic impotence. Eur Urol. 1994;26:46–51. doi: 10.1159/000475341. [DOI] [PubMed] [Google Scholar]
- 45.Montague DK, Lakin MM. False diagnoses of venous leak impotence. J Urol. 1992;148:148–149. doi: 10.1016/s0022-5347(17)36541-2. [DOI] [PubMed] [Google Scholar]
- 46.Montague DK, Lakin MM, Medendorp SV, Tesar LJ. Infusion pharmacocavernosometry and nocturnal penile tumescence findings in men with erectile dysfunction. J Urol. 1991;145:768–771. doi: 10.1016/s0022-5347(17)38446-x. [DOI] [PubMed] [Google Scholar]
- 47.Michal V, Kramar R, Pospichal J, Hejhal L. Direct arterial anastomosis on corpora cavernosa penis in the therapy of erective impotence [in Czech] Rozhl Chir. 1973;52:587–590. [PubMed] [Google Scholar]
- 48.Michal V, Kramar R, Hejhal L. Revascularization procedures of the cavernous bodies. In: Zorgniotti AW, Rossi G, editors. Vasculogenic Impotence: Proceedings of the First International Conference on Corpus Cavernosum Revascularization. Springfield, Illinois: Charles C. Thomas; 1980. pp. 239–255. [Google Scholar]
- 49.Virag R, Zwang G, Dermange H, et al. Vasculogenic impotence: a review of 92 cases with 54 surgical operations. Vasc Surg. 1981;15:9. [Google Scholar]
- 50.Sharlip ID. The incredible results of penile vascular surgery. Int J Impot Res. 1991;3:1. [Google Scholar]
- 51.Montague DK, Barada JH, Belker AM, et al. Clinical guidelines panel on erectile dysfunction: summary report on the treatment of organic erectile dysfunction. J Urol. 1996;156:2007–2011. doi: 10.1016/s0022-5347(01)65419-3. [DOI] [PubMed] [Google Scholar]
- 52.Goldstein I. Arterial revascuarization procedures. Semin Urol. 1986;4:252–258. [PubMed] [Google Scholar]


