Abstract
Leiomyoma is a rare, benign tumor of the bladder. It frequently has an unusual presentation and its treatment options remain controversial. We describe a case of a leiomyoma of the bladder in a young female whose chief complaint was dyspareunia, and we review the management options.
Key words: Bladder Mass, Benign Mass, Leiomyoma, Diagnosis, Treatment
The patient is a 29-year-old white female, gravida 2, para 2, who reported to a local gynecologist that she had experienced dyspareunia and right lower-quadrant abdominal pain and tenderness over the preceding several months. She denied any episodes of fever, chills, gross hematuria, dysuria, or obstructive voiding symptoms. Her past medical history was significant only for pyelonephritis at the age of 3. A pelvic bimanual examination was difficult to perform because of the patient’s discomfort. A pelvic ultrasound demonstrated a benign right ovarian cyst and a 2.7 × 2.9 × 1.9 cm mixedechogenicity mass adjacent to and extending into the right posterior bladder wall and to the right of the cervix. The patient was referred to a local urologist who performed an intravenous pyelogram that suggested a filling defect on the right side of the bladder. Results of urinalysis and urine cytology were normal. Flexible cystoscopy could not be performed in the office because of the patient’s discomfort, and she was referred to us for further evaluation.
Physical Examination
A repeat urinalysis was normal. Flexible office cystoscopy was attempted and demonstrated an abnormal bulging of the right posterolateral wall of the bladder. CT scan revealed a normal upper tract, a slightly dilated mid-right ureter, lobulated enlargement of the uterus consistent with fibroids, and an ill-defined mass in the right bladder wall (Figure 1). The patient was taken to the operating room for an examination under anesthesia that clearly revealed a mass in the right paravaginal area superior to the vagina and separate from the uterus. Bimanual examination demonstrated that the mass was freely mobile. Cystoscopy showed a 3 to 4 cm submucosal mass just proximal and lateral to the right ureteral orifice, in the area of the palpable lesion (Figures 2A and 2B). Retrograde pyelogram demonstrated no filling defects, deviation, or dilation of the right ureter. A transurethral resection (TUR) of the lesion was performed. A frozen section showed leiomyoma of the bladder, and the lesion was subsequently resected endoscopically. At the completion of the resection, the previously palpable pelvic mass could no longer be appreciated by bimanual examination. On postoperative day 1, the patient’s urine was clear, the Foley catheter was removed, and the patient was discharged with a prescription for oral antibiotics.
Figure 1.
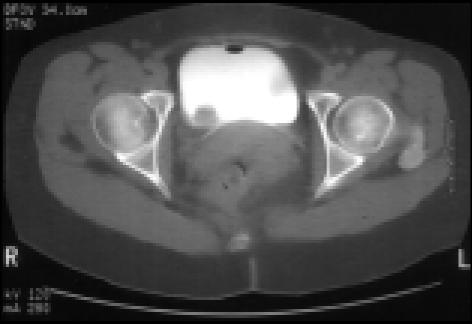
CT scan of the pelvis with intravenous contrast. Note the filling defect on the right posterior wall of the bladder.
Fig 2.
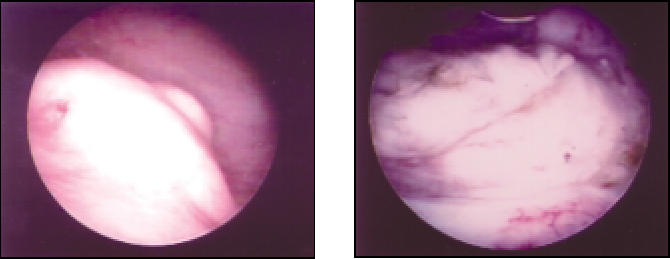
Cystoscopic view of the leiomyoma of the bladder. There was a 3 to 4 cm submucosal mass just proximal and lateral to the right ureteral orifice.
However, 1 month after the initial resection, the patient again reported severe dyspareunia, painful voiding, and right lower-quadrant abdominal pain. A bimanual examination revealed a very tender right adnexa. A urine culture was negative. An office cystoscopy revealed an increase in the size of the previously resected mass at the right posterolateral wall of the bladder. A repeat CT scan revealed a persistent mass along the right posterior wall of the bladder without any pelvic adenopathy or fluid collection. After lengthy discussion regarding further treatment options, including observation, repeat TUR, and open surgical excision, the patient opted to be taken back to the operating room for a partial cystectomy, which was peformed without complications.
After the bladder was opened, the mass, which was noted to be 2.5 to 3.0 cm, located just proximal and lateral to the right ureteral orifice (Figures 3A and 3B), was completely excised with a small cuff of normal bladder. The patient had an uneventful postoperative recovery and was discharged on postoperative day 4. The patient remains asymptomatic 1 year after the surgery. Pathology examination showed interlacing fascicles of spindle cells with abundant eosinophilic cytoplasm and elongated nuclei with blunt ends. No significant atypia, mitotic activity, or other indices of malignancy were noted (Figure 4). Final pathologic evaluation of the tumor determined that it was leiomyoma of the bladder with negative margins.
Fig 3.
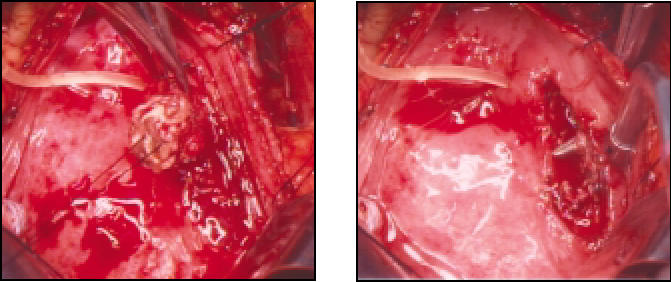
View of the bladder leiomyoma during open surgical excision. The mass was noted to be 2.5 to 3.0 cm, located just proximal and lateral to the right orifice.
Figure 4.

H&E staining of the tumor. Note the interlacing fascicles of spindle cells with abundant eosinophilic cytoplasm and elongated nuclei with blunt ends. 100X.
Discussion
Leiomyoma of the bladder, accounting for 35% of benign bladder tumors, is the most common mesenchymal tumor that occurs in the bladder.1 Since the first report by Virchow,2 an estimated 160 to 235 cases have been reported in the English language scientific literature.3,4 Reported tumor sizes vary from a few millimeters to 30 cm, although a majority of patients have a tumor size of less than 10 cm.
Review of 37 patients with leiomyoma of the bladder showed that a preponderance (76%) of women affected were from 30 to 60 years of age.5 The precise mechanism underlying this epidemiologic observation is uncertain. However, it has been suggested that estrogen may contribute to the growth of leiomyomata.6 Estrogen receptors have been identified in leiomyomatous tissues;7 in addition, estrogen and progesterone receptors are expressed in the bladder.8
The most common symptoms are obstructive voiding symptoms (49%), followed by irritative symptoms (38%), and hematuria (11%).5 It has been suggested that these tumors are symptomatic for two reasons: anatomic location and size.5 Specifically, tumors that are present near the bladder neck or ureteral openings are more likely to cause obstructive symptoms, while larger tumors tend to cause irritative symptoms. In the present case, the chief complaint of dyspareunia was unusual and suggests that patients with dyspareunia of unknown etiology may also require a careful urological evaluation.
The pathology of bladder leiomyoma is similar to that of uterine leiomyomata. The tumors usually appear as whitish-gray nodules with round lumps. There are also fascicles of spiral or vortex-appearing smooth muscle fibers separated by connective tissues. These tumors typically have less than 2 mitotic figures per high-power field.9 Grossly, these tumors are classified into three types: 1. endovesical, 2. intramural, and 3. extravesical. In the literature, the endovesical form is reported in 63%, the intramural in 7%, and the extravesical in 30% of cases. Of these types of bladder leiomyomas, the endovesical forms are most likely to be symptomatic because they protrude into the lumen of the bladder and are thus more likely to cause obstruction, irritation, or bleeding.
The initial evaluation of these tumors must include upper- and lower-tract evaluation. Once the upper tract is cleared, cystoscopy with biopsy of the mass will usually yield a definitive diagnosis. On cystoscopy, the leiomyoma typically is seen as a submucosal bladder mass with smooth and regular overlying mucosa. When a diagnosis of bladder leiomyoma is made, there are three options: 1. observation, 2. transurethral resection of the tumor, and 3. open surgical excision. Since malignant transformation of bladder leiomyoma has not been reported, some patients with bladder leiomyoma as an incidental finding may prefer to defer definitive treatment until symptoms appear. In a report on 37 patients, Goluboff and associates5 described treating asymptomatic patients conservatively and 34 patients with definitive surgery. Of the 34 patients who had definitive surgery, 11 had TUR while 23 had open surgery; 17 had simple enucleation, 6 had partial cystectomy, and 2 had cystoprostatectomy. Cystoprostatectomy was performed in patients with tumors greater than 20 cm and involving the ureters. Of these patients, two who underwent TUR needed a second operation for residual tumor. With such low rate of reoperation, it seems that TUR is a reasonable initial choice of treatment in patients with relatively small tumors.
In conclusion, bladder leiomyoma is a rare, benign tumor of the bladder. When it is first diagnosed, a careful work-up should be initiated to rule out any possibility of a malignant tumor. But once the diagnosis is made, most of these tumors can be treated with TUR or local excision.
Main Points.
Although rare, leiomyoma is the most common mesenchymal tumor that occurs in the bladder.
Approximately three-quarters of cases occur in women between the ages of 30 and 60.
Estrogen may contribute to the growth of leiomyomata.
Malignant transformation of bladder leiomyoma has not been reported.
Transurethral resection is a reasonable initial choice of treatment in patients with relatively small tumors.
Cystoprostatectomy has been performed in patients with large tumors involving the ureters.
Asymptomatic patients may prefer to defer treatment until symptoms appear.
References
- 1.Blasco Cesares FJ, Sacristan Sanfelipe J, Ibarez Servio L, et al. Characteristics of bladder leiomyoma in our setting. Arch Esp Urol. 1995;48:987–990. [PubMed] [Google Scholar]
- 2.Kretschmer JL. Leiomyoma of the bladder with a report of a case and a review of the literature. J Urol. 1931;26:575–589. [Google Scholar]
- 3.Teran AZ, Gambrell RD. Leiomyoma of the bladder: a case report and review of the literature. Int J Fertil. 1989;34:289–292. [PubMed] [Google Scholar]
- 4.Acapont Perez FM, Gil Salomon M, Chuan Nuez P, et al. Bladder leiomyoma. Arch Esp Urol. 1995;48:1035–1037. [PubMed] [Google Scholar]
- 5.Goluboff ET, O’Toole K, Sawczuk IS. Leiomyoma of the bladder: report of case and review of literature. Urology. 1994;43:238–241. doi: 10.1016/0090-4295(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 6.Neri A, Rabinerson D. Multiple leiomyoma of the urinary bladder in a hysterectomized woman. Acta Obstet Gynecol Scand. 1995;74:242. doi: 10.3109/00016349509008950. [DOI] [PubMed] [Google Scholar]
- 7.Elia G, Bergman A. Estrogen effects on the urethra: beneficial effects in women with genuine stress incontinence. Obstet Gynecol Surv. 1993;48:509–517. doi: 10.1097/00006254-199307000-00028. [DOI] [PubMed] [Google Scholar]
- 8.Tiernery WM, Ehrlich CE, Bailey JC. Intravenous leiomyomatosis of the uterus with extension to the heart. Am J Med. 1980;69:471–475. doi: 10.1016/0002-9343(80)90022-4. [DOI] [PubMed] [Google Scholar]
- 9.Knoll LD, Segura JW, Scheithauer BW. Leiomyoma of the bladder. J Urol. 1986;136:906–908. doi: 10.1016/s0022-5347(17)45124-x. [DOI] [PubMed] [Google Scholar]


