Abstract
The finding of varicocele in an adolescent male is common. Varicocele rarely causes symptoms and is often diagnosed on the routine physical examination. There is clear association between varicocele and male factor infertility; however, there is debate about whether, when, and whom to treat when present in adult or adolescent males. This review of the epidemiology, etiology, pathophysiology, and treatment of the adolescent with varicocele will provide the reader with tools to make appropriate decisions in dealing with this condition.
Key words: Varicocele, Varicocelectomy, Testicular growth arrest, Male infertility, Retroperitoneal ligation, Microsurgical inguinal repair
Avaricocele can be defined as an abnormal tortuosity and dilation of the veins of the pampiniform plexus (PP). Idiopathic varicocele is usually asymptomatic. It is noticed as an asymmetry in scrotal size, and presents as heaviness in the scrotum, or, rarely, with testicular pain. In most cases, the adolescent is unaware of the varicocele, and it is discovered during a regular physical examination or examination for military service.1–4
The incidence of high-grade varicocele is approximately 5% throughout the world.5 Varicocele is associated with a time-dependent growth arrest in adolescents and adult males.6 There is a clear association between varicocele, infertility, and testicular growth arrest.7–9 It is also known that varicocelectomy can reverse growth arrest in adolescents.10–13 This knowledge has raised the question of how best to manage adolescents with varicocele.
Adolescents do not present with infertility, and thus should prophylactic repair be performed to prevent infertility in the future? Who would benefit the most from varicocelectomy: adolescents with testicular growth arrest or any adolescent with varicocele? Is it better to wait for a semen analysis or offer earlier treatment based on testicular growth arrest? These questions can be only answered when we have a better understanding of the pathophysiology of varicocele.
This review presents the current literature on adolescent varicocele and provides guidelines to the clinician on how to manage adolescents with varicocele.
Epidemiology
In the general population of healthy males, the overall incidence of varicocele (all grades) is 10% to 15%.4,5,14,15 Approximately 30% to 50% of males with primary infertility have varicocele.16–19 Varicocele is most common on the left side. It appears at early puberty, but can occasionally be found in preadolescent boys.2,20 The incidence in older adolescents varies from 12.4% to 17.8%, with an average of 14.7% (Table 1), similar to the incidence in adult males.
Table 1.
Incidence of Varicocele in General Population of Healthy Adolescents
Anatomy
The arterial blood supply to the testicle comes from the testicular artery, vasal artery, and cremasteric artery. At the level of the testis, all three arteries anastomose to allow adequate blood supply, even with the division of the testicular artery.21,22
Venous drainage (Figure 1) is more complicated, with many individual variations. Above the testis is a network of communicated veins called the pampiniform plexus, which drains via the testicular vein trunci, pudendal veins, and cremasteric veins.23,24 In most cases, the testicular vein trunci form a single testicular vein entering the renal vein on the left and the inferior vena cava on the right. Venographic studies have demonstrated that the left testicular vein can rarely enter the inferior vena cava, and there are communications between the testicular vein and the inferior vena cava below the level of the renal veins.25–27 There is also cross-communication between the left and right testicular venous systems (Figure 2).26,28–30
Figure 1.
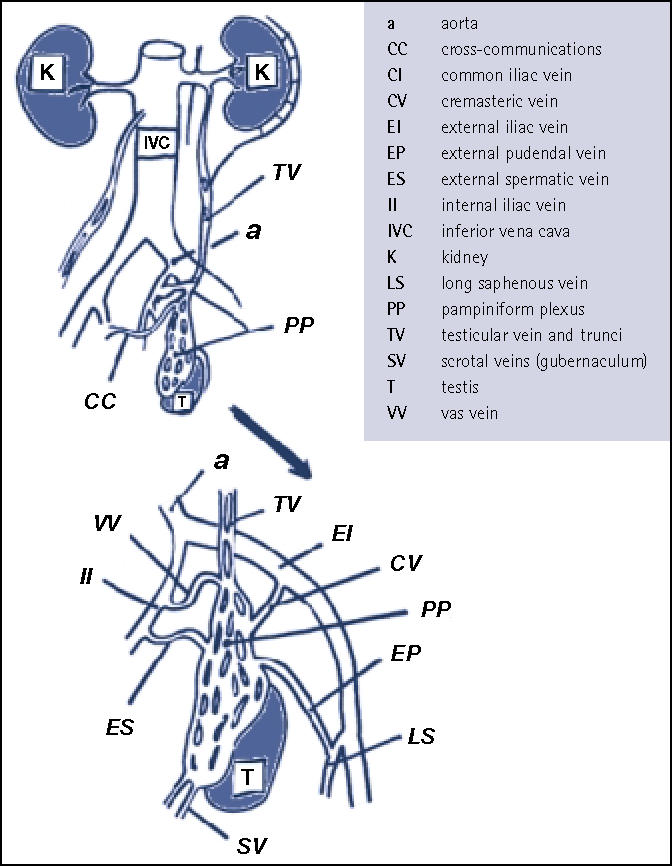
Anatomy of venous drainage from left testis. For abbreviations, see accompanying list.
Figure 2.
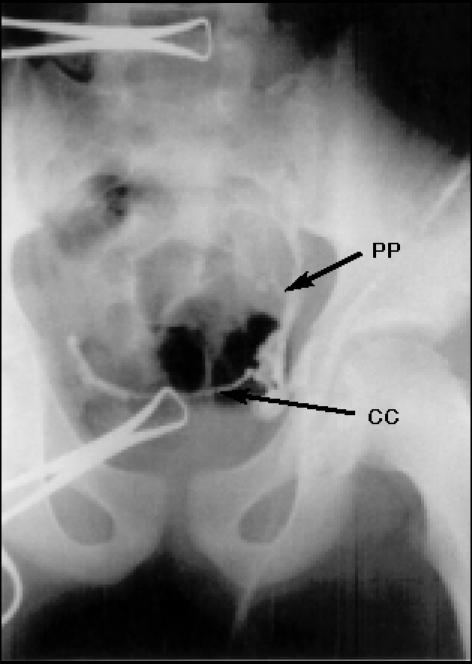
Intraoperative venogram showing left to right cross-communicating veins. CC, cross-communications; PP, pampiniform plexus veins.
Etiology
The predominance of left-side varicocele and the unique anatomy of the left testicular vein are the basis for several theories explaining the etiology of varicocele. The presence of venous valves was long believed to be a mechanism guarding against developing varicocele, and incompetence of the venous valve system was thought to be responsible for varicocele development. However, it was shown that there are males without varicocele who have an incompetent venous valve system and males with varicocele who have competent venous valves.29
Hydrostatic pressure difference could be a factor causing a left varicocele. Although the left testicular vein is longer than the right, the simple difference in hydrostatic pressure of a standing column of blood cannot be the only reason for development of varicocele, because all males would be affected.
The “nutcracker effect” is thought to occur when the testicular vein is compressed between the superior mesenteric artery and aorta. The increase in hydrostatic pressure results in varicocele formation. Although a high left renal vein to vena cava pressure gradient is noted in patients with varicocele, it is not a consistent feature.31,32
More recently, it has been hypothesized that increased arterial blood flow to the testis at puberty exceeds venous capacity, resulting in venous dilatation and varicocele.33,34 The results of animal studies to support this interesting theory are conflicting, and confirmation in humans will be necessary.35
The finding of elevated nitric oxide, a potent vasodilator, in the PP of males with varicocele raises another potential cause for the etiology of varicocele in the adolescent.36
Pathophysiology
The pathophysiology of varicocele can be studied in animal models by partial ligation of the left renal vein.37 Many features of the human condition, such as increased temperature of the affected testis, increased arterial blood flow, and histopathologic changes, can be replicated in animal models.38
The following theories attempt to explain the deleterious effect of the varicocele on testicular function:
Hyperthermia. The presence of varicocele is associated with elevated scrotal and testicular temperature and altered spermatogenesis.39 Experimental studies have shown that spermatogenesis occurs optimally at temperatures lower than body temperature. Many of the enzymes responsible for optimal DNA synthesis in the testis are temperature- dependent.40,41 The scrotal position of the testis and the countercurrent cooling system provided by the PP surrounding the testicular artery allow for heat exchange and are responsible for regulating optimal temperature for spermatogenesis.42 Stasis of blood in the varicocele with resultant increased temperature may be responsible for the deleterious effect of varicocele on spermatogenesis.43 Increased temperature is associated with decreased number of spermatogonia (SP) and increased apoptosis of germinal epithelium cells.44
Abnormal blood flow. A current hypothesis assumes that increased blood flow through the testis can affect spermatogenesis.45,46 An increase in hydrostatic pressure with a change in filtration pressure could considerably alter the composition of the interstitial fluid.47 This conceivably could alter the intimate paracrine communications between the Leydig cells (LCs), peritubular myoid cells, and Sertoli cells (SCs), ultimately affecting spermatogenesis.1 The myoid cells and capillary epithelium undergo pathological changes in association with varicocele that may effect transmembrane transport of substrates to the germinal epithelium.48
Hypoxia and “adrenal reflux.” Stasis of blood in the PP could affect partial oxygen pressure and change aerobic metabolism in the testis. However, hypoxia has not been demonstrated in testicular venous blood sampling in humans or experimental animals.49,50 Reflux of blood down the testicular vein has been demonstrated in patients with varicocele.51–53 Therefore, exposure of the testis to adrenal or renal metabolites is hypothesized to be a cause for testicular damage. However, adrenal or renal metabolites at the level of the testis have not been documented.37,54 Adrenalectomy in rats with experimental varicocele did not diminish the effects of the varicocele.55,56 Thus the adrenal/renal reflux theory does not appear to be responsible for the testicular damage associated with varicocele.55,57
Endocrine imbalance. Puberty, spermatogenesis, and testicular development are regulated by the hypothalamic-pituitary-testicular axis. There is a wide array of endocrine abnormalities associated with varicocele. LCs are under the control of luteinizing hormone (LH) and are responsible for testosterone (T) production. Some studies have shown that the serum T level may be affected by varicocele; however, it is intratesticular testosterone that is important in the regulation of spermatogenesis.58,59 In experimental animal models, varicocele can result in a decreased intratesticular testosterone level.60 The results of human studies are mixed. Ando and colleagues found reduced serum T level in males with varicocele and increased serum T level after repair of the varicocele.61–65 Swerdloff and Walsh, however, showed that there was no difference in testosterone level between males with and without a varicocele.66
Increased LH serum levels and an abnormal response to gonadotropin-releasing hormone (GnRH) could implicate a compromise of the hypothalamic-pituitary-gonadal axis involved in the control of T and spermatogenesis, a pattern similar to hypergonadotropic hypogonadism.67,68 Increased LH level results in LC hyperplasia, a known histologic finding in varicocele testicular biopsies.69–71
SC responsiveness to follicle-stimulating hormone (FSH) may be diminished in varicocele patients. Stimulation of SCs with FSH reversed spermatogenesis arrest in experimental animal models.72 Varicocelectomy restored normal levels of FSH.73 Altered levels of serum inhibin found in patients with varicocele may reflect altered function of SCs.74 Cameron and associates noticed that Sertoli-germ cell junctional complexes appeared to be structurally abnormal in patients with varicocele.75 They concluded that testicular disruption associated with varicocele is a phenomenon of the adluminal compartment, and that SCs are more sensitive to perturbation of the testicular environment than are germ cells. SCs may be the primary intratubular site of alteration leading secondarily to spermatogenic disruption.76 Histologic studies of the testis from patients with varicocele showed absent germ cells or altered spermatogonia to SC ratio, signs often associated with SC dysfunction.77 In addition to measuring circulating hormone levels, screening for point mutations in the circulating hormones, receptors, and secondary signaling systems may give more precise insight into male infertility and allow for patient stratification.78
Paracrine regulation of the testis. Insight into the detailed mechanism of spermatogenesis is even more complicated because it is also regulated by complex interactions and signals at the cellular level in the testis (Figure 3).1,79
Figure 3.
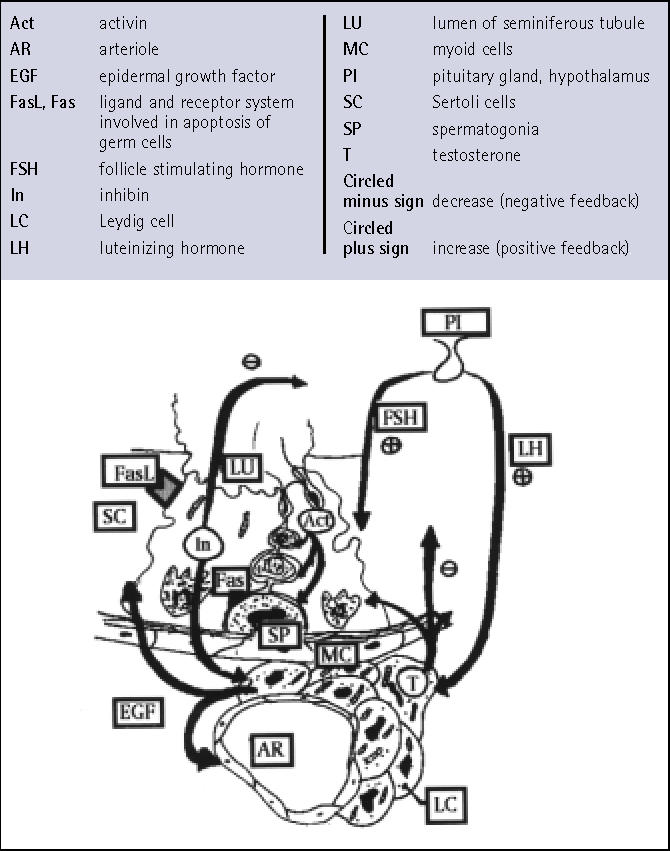
Endocrine regulation of spermatogenesis. Sertoli cells under the influence of follicle-stimulating hormone regulate spermatogenesis by activin, androgen binding protein, and direct interactions with spermatogonia and spermatids. Leydig cells (LCs) regulate spermatogenesis by achieving a high intratesticular testosterone concentration. Epidermal growth factor (EGF) is produced by LCs and controls mitotic divisions of germinal epithelium. EGF also stimulates divisions of peritubular myoid cells that in return produce another paracrine hormone, peritubular myoid substance (PmodS). For abbreviations, see accompanying list.
Both SCs and LCs regulate spermatogenesis by steroidogenesis and growth factor production.80,81 SCs tightly regulate germ cell proliferation and differentiation and are implicated in the control of germ cell apoptosis. Fas (APO-1, CD95), a transmembrane receptor protein expressed by germ cells, transmits an apoptotic signal within cells when bound by Fas ligand (FasL) produced by SCs. The Fas system has been implicated in regulation of apoptosis in germ cells.82 SCs stimulated by FSH produce inhibin (In) and activin (Ac).83 Inhibin has negative feedback control on the pituitary and FSH secretion. It also binds to LCs regulating T production. Activin binds to round spermatids and spermatogonia (SP), affecting spermatogenesis. SP are known to stimulate transferrin production by SCs by an unidentified protein substance.84
LCs control spermatogenesis not only by steroid production but also by epidermal growth factors (EGFs) that bind to SP and spermatids regulating cell divisions.85 Receptors for transforming growth factor (TGF), one of the EGFs produced by LCs, are found in peritubular myoid cells (PC). PCs secrete peritubular myoid cell substance (PmodS) that stimulates SCs. LCs control adluminal tubular compartment and transport of nutrients from the vascular space to germinal epithelium by vascular endothelial growth factor (VEGF). VEGF is of particular interest in varicocele, because it regulates endothelial permeability and is an angioproliferative factor.86
Locally produced neurotropins play their distinct role in spermatogenesis regulation.87 Opioid receptors are found on LCs. During stress, release of endorphins stimulates opioid receptors and decreases testosterone production. Blocking opioid receptors by naloxone restores testosterone production to normal.88 Naloxone did not change the serum concentration of LH, FSH, or T when given to patients with varicocele.89
Free radicals may also be considered paracrine substances, because they are produced and act locally. There is strong evidence that varicocele is associated with increased concentration of free radicals in semen. Free radical concentrations normalize after varicocelectomy.90,91
With each discovery of a new paracrine substance and a better understanding of the molecular mechanisms controlling spermatogenesis, we will better define the pathophysiologic mechanisms responsible for growth arrest and deleterious effects on spermatogenesis. The ability to measure these substances may allow us to predict which adolescent and/or adult with varicocele requires surgical intervention.
Pathology
Testicular hypotrophy. The testicular function most affected by varicocele is spermatogenesis.92 The most common findings on semen analysis are increased number of pathologic sperm forms, decreased motility, and decreased sperm density.8,93,94 Sperm analysis in adolescents with varicocele shows decreased sperm density, increased number of pathological forms, and decreased motility; however, there are no established norms for adolescent semen analysis.93 Varicocele is also associated with testicular growth arrest in adolescents.10,12 Testicular growth arrest may be considered the hallmark of testicular damage in adolescent varicocele. Significant volume loss in adolescents with varicocele has been noted in 77% of boys, 10% of whom had a left testis one fourth the size of the right testis.95 Testicular hypotrophy is time-dependent.96,97
Testicular volume during preadolescence is constant, and at the onset of puberty the testis suddenly increases in size even prior to other pubertal changes. In adolescents with varicocele, the rapid growth of the testis between the ages of 11 and 16 is affected by varicocele and results in a volume discrepancy between the right and left testis. The hypothesis that there is a negative correlation between testicular volume and sperm density, motility, and number of pathologic forms is well supported in the literature.8,98,99
Histopathology. Testicular biopsy in males with varicocele shows a wide array of abnormalities. The most common findings are LC hyperplasia, decreased number of SP per tubule, spermatogenesis arrest, and sloughing of germinal epithelium.99–103 A thickened basement membrane of seminiferous tubules and proliferative lesions of endoepithelium are often demonstrated and may affect transport of oxygen and glucose through these structures.104,105 The damage to the basement membrane seems to be time-dependent, as shown by ultrastructural and immunohistochemical observations that highlighted focal damage at the level of the peritubular basal lamina in pubertal boys with varicocele, but this damage was not as severe as that described in adult varicocele.106 Myofibroblasts obtained from pubertal males with varicocele showed no evidence of transformation into fibroblasts other than increased presence of extracellular matrix. In adult males, myofibroblasts transform into fibroblasts, with varicocele causing peritubular fibrosis. This can explain why the varicocelectomy in adolescents is able to reverse growth arrest and restore normal architecture of the testis, while the same procedure in adults with varicocele does not always affect testicular atrophy, although it may improve the semen characteristics.107,108
Peritubular fibrosis and increased thickness of basal membrane correlate negatively with sperm density and number of pathologic forms.109 The longitudinal smooth muscle fibers in vein walls are hypertrophied in high-grade varicocele; however, it is not yet clear whether this is a cause or a consequence of varicocele. One can stipulate that vein wall hypertrophy may be the result of a high volume of blood flowing through the vessels or increased hydrostatic pressure.110
Diagnosis
The adolescent with varicocele is often asymptomatic, and the varicocele is detected on routine physical exam. The patient should be examined standing in a warm room to relax the scrotum and allow easier examination of the spermatic cord. The scrotum is first visually inspected for any obvious distention around the spermatic cord; a visible varicocele is considered a large or grade 3 varicocele. The scrotum, testes, and cord structures are then gently palpated. A palpable varicocele has been described as feeling like a bag of worms or a squishy tube. More subtle varicoceles may feel like a thickened, asymmetric cord. The nonvisible but palpable varicocele is considered to be moderate in size (grade 2). If a varicocele is not palpable, but the patient performs a Valsalva maneuver that distends the PP of veins, a small (grade 1) varicocele is present.
After examining the patient in the standing position, the patient should be examined supine. Idiopathic varicocele is more prominent in the upright position and disappears in the supine position. A thickened cord due to a varicocele should resolve in the supine position, whereas a thickened cord due to a lipoma will not change when the patient is supine. Secondary varicocele, especially on the right side, can be caused by serious conditions such as retroperitoneal tumors, kidney tumors, or lymphadenopathy.111 A secondary varicocele does not change its size so dramatically in the supine position.
Testicular size needs to be measured to determine whether the varicocele is adversely affecting the growth of the testis. The volume of a normal testis measures 1 cc to 2 cc in the prepubertal male. Because of extensive individual variation in normal growth and development, testicular size is correlated with Tanner stage, growth velocity, and bone age rather than chronological age.
A number of methods have been used to measure the size of the testis. These include visual comparison, rulers, calipers, comparative ovoids (Prader orchidometer), punched-out elliptical rings (Takahara orchidometer), and ultrasound. A high correlation (r = .992) between ultrasound and actual volume was noted and was shown to be highly reproducible.112 The Prader orchidometer was shown to correlate with ultrasound measurement in 256 patients (r = .91), although the degree of correlation was dependent on the investigator’s clinical experience. In a clinical study of 22 male adolescents with a varicocele, 24% of patients with growth arrest would have been missed if measured by Prader orchidometer alone, and 3 patients felt to have a significant size discrepancy (>2 mL) by Prader orchidometer measurements were found to be normal by ultrasound volume estimate. These findings indicate that clinical estimates of testicular size by the Prader orchidometer are not as accurate or reproducible as those determined by ultrasound. Accurate measurement is important because operative decisions rest in the balance.113 This finding was recently confirmed by Diamond and colleagues who recommend annual ultrasound assessment of testicular volume in adolescents with varicocele.114
There is considerable disagreement as to what constitutes a significant size discrepancy justifying surgical intervention. Testicular ultrasound is the most accurate and reproducible method to assess testicular volume and significant testicular size variations. A volume difference of less than 2 mL can be due to the measurement technique alone. Therefore, size variation of more than 2 mL by ultrasound is currently the best indicator of testicular damage and should serve as the minimal requirement for surgical repair of the adolescent varicocele.1 Surgical intervention reverses testicular growth arrest, and assessment of testicular volume postoperatively predicts resolution of the varicocele.12,11
Management
There are some cardinal questions to be answered regarding management of adolescent varicocele:
Once a varicocele has been found, what information needs to be given to the patient and his parents? A number of psychological reactions (anxiety, depressed mood) were experienced in approximately 30% of boys who were informed about varicocele.116 Because the word infertility is often associated with sexual impairment, we believe that during discussion with the patient and his parents, the only fact that should be stressed is that varicocele may result in a decrease in testicular volume that can be reversed by surgical treatment. However, it is hard to discount the association between varicocele and infertility in this era of common accessibility to the medical literature on the Internet (we found 1743 Web pages in searching for the term varicocele; many included the word infertility in the text). Because there are studies that demonstrate an abnormal semen analysis in adolescents, it seems advisable to discuss all findings first with the parents who can be helpful in presenting the problem to the child.117,118
Once diagnosed, whom should we treat? Varicocele is the most common correctable cause of male infertility.119 Two thirds of patients will have improvement in semen analysis after varicocele repair, and 40% of partners will become pregnant.16 Historically, adolescent varicocele was left untreated because its relationship to infertility was not well established. Subsequently, Kass and Belman showed that testicular growth arrest could be reversed by varicocelectomy in adolescents.120 Repair of varicocele not only reversed growth arrest but also improved semen analysis in adolescents and young males.118,121,122
There is good evidence that, if left untreated, with time the varicocele will continue to affect testicular growth with loss of volume and progressive deterioration in semen analysis.6,123 Goldstein and Gorelick suggest that varicocele causes a progressive decline in fertility and that prior fertility in men with varicocele does not predict resistance to varicocele-induced infertility in the future, so-called secondary infertility.6 However, Lund and Larsen followed 39 men with varicocele for 8 years and were not able to show progressive decline in semen analysis results compared with healthy subjects.124
The association between varicocele and infertility is well established.7 The most difficult question is which clinical test should we use to establish the indications for surgical treatment in an adolescent with varicocele?
Currently, the clinical tests used to establish criteria for varicocele repair are:
Grade of varicocele
Measurement of testicular volume to assess testicular growth arrest
GnRH stimulation test
Measurement of PP vein diameter
Serum LH, FSH, and inhibin levels
Semen analysis
1. Varicocele grade. Varicocele grade does not correlate well with abnormal semen analysis or infertility in adults.125 There are varying opinions regarding correlation between grade of varicocele and degree of testicular hypotrophy in adolescents. Lyon and associates found no correlation of varicocele grade and testicular size in 30 adolescents.95 In contrast, Skoog, Steeno, and Paduch all independently noticed that boys with severe varicocele have a smaller ipsilateral testicle.10,113,116 It was also noticed that the smaller the testis, the worse the semen analysis results.8,93 However, grade of varicocele by itself should not be the sole indication for treatment.
2. Testicular volume. There is an abundance of literature confirming that varicocele is associated with testicular growth arrest in adolescents, and varicocele repair results in testicular “catch-up” growth.10,118,121,122 Testicular growth arrest with a volume difference of more than 2 mL assessed by ultrasonography is the most common indication for treatment.1,10 The development of secondary infertility is another strong argument for early varicocele repair because, if left untreated, varicocele can not only affect testicular volume but also spermatogenesis.6 A decrease in testicular volume is the best indicator for surgical correction of varicocele. However, not every boy with varicocele and testicular growth arrest will be infertile, and there is still a need to search for a test that would better distinguish between adolescents with a varicocele who will develop infertility and those who will remain fertile. In adult males, the situation is a little simpler because the indications for surgery are usually established after 12 months of infertility confirmed by abnormal semen analysis and the presence of varicocele. Obtaining a semen sample in adolescents is possible but difficult.
3. GnRH stimulation test. Damage to germinal epithelium results in compensatory stimulation of the pituitary gland and subsequent increase in FSH and LH production by gonadotrophs.126 Intravenous administration of GnRH stimulates the pituitary gland to release FSH and LH. FSH levels are elevated in any condition (like varicocele) affecting the integrity of germinal epithelium.127 In theory, the GnRH stimulation test could distinguish between adolescents with varicocele who have abnormal testicular functions and those who have normal spermatogenesis.11 However, in clinical practice, the GnRH stimulation test is expensive, requires multiple serum samples, and lacks an association between abnormal results, growth arrest, and infertility.128–130 An abnormal GnRH stimulation test was found in 30% of adolescents with varicocele and was not correlated with atrophy or infertility.131 Currently, it seems that the GnRH stimulation test has a limited role in the clinical evaluation of adolescents with varicocele in the United States, but is still used in clinical trials in Europe.132
4. PP vein diameter. Ultrasonographic measurement of PP vein diameter (PPVD) has been used to look for subclinical varicocele in the adult infertile population when the physical exam is inconclusive and to follow persistent varicocele, but PPVD measurements are not useful in adolescents.133,134
5a. Inhibin level. Serum inhibin levels reflect the integrity of the seminiferous tubule and function of the SCs. Inhibin measurement in serum does not add any diagnostic information not found by FSH measurement. Inhibin B levels after dynamic GnRH stimulation failed to aid in stratification of adolescents with varicocele.136 At present, there are not enough data to support the use of serum In levels in making clinical decisions.74,83,137–139
5b. FSH stimulation. FSH has been utilized as an adjuvant therapy after varicocelectomy in adult infertile patients; however, it also can be used in adolescents with varicocele. Radicioni and Schwarzenberg postulate that more than 50% of improvement in semen analysis in males treated with a 3-month course of FSH indicates a better outcome after varicocelectomy.140 However, at present there isn’t enough evidence to advocate FSH stimulation prior to varicocelectomy in adolescents.
6. Semen analysis. Increased number of pathologic forms, decreased progressive motility, and decreased sperm density are the most common abnormalities found on semen analysis in men with varicocele-related infertility. Varicocele is associated with impaired disposal of residual sperm cytoplasm in the testis and epididymis.141 The retained sperm cytoplasm causes release of free radicals and infertility. Varicocelectomy was shown to lower the number of sperm with retained cytoplasm.142 It is concluded that varicocele may cause deleterious alterations in early spermatid head differentiation during spermiogenesis and that varicocele patients with a high incidence of sperm acrosome and nucleus malformations are appropriate candidates for varicocele correction.143 By applying strict morphologic criteria to semen analysis, it was shown that varicocele repair improves the morphologic abnormalities of the sperm head found on preoperative semen analysis.144 Because there is good correlation among sperm morphology, fertility index, and results from artificial reproductive techniques (ART), it is prudent to offer varicocelectomy to men with abnormal sperm morphology even with normal testicular size.145,146
Management summary. Currently, prophylactic surgery for every adolescent with varicocele is not advised because it would result in the treatment of 15% of adolescents. However, it appears that treatment should be offered to:
Adolescents with testicular growth arrest (2 SD from normal testicular growth curves, more than 2 mL of difference between left and right testicles)
Adolescents with abnormal semen analysis with high-grade varicocele
Adolescents with symptoms: pain, heaviness, swelling
Adolescents with bilateral varicoceles
Treatment Options
Treatment options in the management of adolescents with varicocele originated from the practice in adult male infertility.
Surgical ligation and division of the testicular veins or intravenous embolization of the testicular veins accomplish varicocele repair.
Three open surgical approaches are currently used: subinguinal (Marmar), inguinal (Ivanissevich), and retroperitoneal (Palomo). Laparoscopic varicocele ligation is often used in adults. Embolization techniques, regardless of embolizing material, can be classified as antegrade (infusion through scrotal part of the PP veins) and retrograde (catheter placed through femoral vein puncture) techniques.
Failure rate, frequency of complications, cost, and outcome are important factors that need to be evaluated in choosing the preferable treatment option in adolescent patients (Table 2). It is important to remember that most studies on varicocele repair concern adult infertile males with varicocele and not adolescents.
Table 2.
Surgical Approach, Complications, and Relative Costs of Varicocele Repair
| Technique | Hydrocele Rate | Failure Rate | Cost | References |
|---|---|---|---|---|
| Retroperitoneal | 7%–10% | 9%–11% (artery sparing) | Low | 10,147 |
| <3% (artery taking) | 12 | |||
| Inguinal | 3%–7% | 9%-12% | Low | 150,163,188 |
| Inguinal microscopic | <1% | 2.1% | Moderate | 155 |
| 0.6% | 156 | |||
| Laparoscopic | 1.25% | 9% | High | 189 |
| 1.25% in adolescents | 190 | |||
| Embolization | 19% | High | 172 |
Failure rate. Recurrence of the varicocele after the repair can occur in 9% to 16% of adolescents. It was shown by Lund and our group that persistence of varicocele should be assessed by performing an ultrasound 6 months after surgery.148 Persistence of the varicocele results in lack of “catch-up” testicular growth.12 Most authors attribute the high persistence rate to missed venous collaterals that run parallel to the main testicular vein. The collaterals can be quite difficult to identify and ligate separately from the testicular artery. The reported persistence rate using the artery-sparing retroperitoneal approach ranges from 3% to 11%.12,147,149,150 Ligation of both testicular vein trunci and the artery has the advantage of a decreased persistence rate and does not result in testicular atrophy, because the testis has collateral arterial blood supply from the cremasteric and deferential arteries.12,21 Atassi and colleagues achieved a persistence rate below 2% in adolescents treated by high retroperitoneal ligation with testicular artery ligation.12 Artery and vein ligation using laparoscopy was also shown to result in similar catchup growth of the testis in adolescents and a low persistence rate.151 There is, however, some objection to simultaneous ligation of the testicular artery in men with previous inguinal surgery, as there may be a compromised blood supply from the cremasteric and deferential arteries. Interruption of the testicular artery in these patients creates a high probability of developing testicular atrophy. Subsequent vasectomy in patients with testicular artery division should be avoided because ligation of the vasal artery could result in testicular atrophy.
Nagar recently reported a low persistence rate after varicocelectomy, if patients were stratified using color Doppler ultrasound.152 A high ligation was performed only when reverse blood flow was demonstrable in the varicocele during a Valsalva maneuver, and a low approach was utilized when this finding was absent. One can hypothesize that pelvic collateral and cross-communicating veins were responsible for the varicocele in patients who showed lack of reverse blood flow through the PP on ultrasound. Obviously, outcome in this group would be unsuccessful if managed by a high retroperitoneal approach. The high incidence of pelvic splanchnic veins communicating with the internal spermatic vein found during embolization confirms Nagar’s hypothesis.153 We previously showed the importance of cross-communicating veins and pelvic veins in the persistence of varicocele; these results and Nagar’s observations are opening a whole new area for future study.154
The high varicocele persistence rate and postoperative hydrocele rate led to the development of microsurgical varicocelectomy. Both subinguinal and inguinal microsurgical repair are used quite often in adults with varicocele and indeed offer lower persistence rates and a low incidence of postoperative hydrocele.155–157 The low persistence rate using the microsurgical inguinal repair is attributed to ligation of all distended veins and collaterals at the level of the internal inguinal ring.155,156 Because more pediatric urologists and surgeons are gaining experience in microsurgical inguinal varicocele repair, we may see this procedure becoming a surgery of choice for adolescents.158,159 Reports by Minevitch and Goldstein demonstrated a significantly lower rate of persistence and postoperative hydrocele in adolescent patients.158,160,161 The microscopic approach allows one to ligate only the veins, leaving the lymphatic vessels intact and decreasing the postoperative hydrocele rate to less than 1%.156,157 These encouraging reports were recently confirmed by a prospective study by Cayan and associates, who treated 468 patients by either high retroperitoneal ligation or inguinal microsurgical repair. Microsurgical varicocelectomy resulted in fewer cases of postoperative hydrocele and recurrences.162
Laparoscopic varicocele repair with and without artery-sparing modifications are suitable surgical techniques.163–165 The testicular vein and artery can be divided with hemostatic clips or coagulated with bipolar electrode.166 Laparoscopic varicocele ligation can be employed in adolescents.167–169 Laparoscopic surgery in the pediatric population bares the risk of significant complications like bowel perforation, major vascular injury, pneumothorax, and incisional hernia. Laparoscopic varicocele ligation is more expensive, takes longer, and offers no benefits of pain management or earlier return to daily activities as compared with the microvascular inguinal approach.170 In a prospective, randomized study to compare laparoscopy versus open repair for varicocele in adult males with infertility (160 patients in the laparoscopy arm and 120 in the inguinal arm), laparoscopy was shown to be more expensive and to lack any advantages over the inguinal approach.171 We are also concerned about the much higher cost of laparoscopy and its potential risks. In our opinion, laparoscopic varicocelectomy should not be used in adolescents. A retroperitoneal approach or microsurgical inguinal repair is preferred.
Retrograde embolization, unfortunately is associated with an unacceptable high rate of persistence and is the most expensive of treatment techniques.1 A possible explanation of such a high persistence rate of varicocele after embolization is the highly variable anatomy of the testicular venous drainage and technical difficulties.172 Because the embolization is performed in otherwise healthy young males with approximately 70 more years of life, one should also be concerned about radiation exposure during embolization, with a subsequent 0.1% life-long risk for cancer.173 Antegrade embolization is more often used to treat persistent varicocele than as an initial treatment.174–178
Other options to decrease the rate of varicocele persistence are intraoperative venography and methylene blue injections.27,150,179,180 Intraoperative venography in theory should facilitate ligation of all testicular vein trunci and decrease the rate of persistence. Hart and associates recommend routine use of intraoperative venography because 16% of their 62 patients had missed venous vessels after initial venous ligation.181 Similar conclusions, based on a decreased persistence rate, were also made by Levitt, Zaontz, and Gill.182–184 However, Palmer and Kass reported no difference in their rate of varicocele persistence after repair with and without intraoperative venography.147,150,179 Based on these studies, intraoperative venography offers a marginal benefit in prevention of persistent varicocele.
Based on our review of the literature and the results of a survey of pediatric urologists in the United States, high retroperitoneal ligation of the testicular artery and veins offers the best results in adolescents. Although currently the high retroperitoneal approach is a treatment of choice in adolescent varicocele, pediatric urologists should consider using the microscopic inguinal or subinguinal approach with arterial preservation.
The Future
What are future directions for urologists and scientists interested in varicocele? Advanced molecular biology techniques used for evaluation of the infertile male have increased our understanding of the physiology of spermatogenesis. We now realize that azoospermia and severe oligoasthenospermia are rare in pure varicocele. It is estimated that 14.7% of males with azoospermia carry microdeletions of the long arm of chromosome Y.185 Males with varicocele and azoospermia or severe oligoasthenospermia may actually suffer from point mutation or deletion of genes important in spermatogenesis. It seems unlikely that those patients as either adults or adolescents will benefit from varicocelectomy. By screening for aberrations of genes involved in regulation of spermatogenesis, we will be able to exclude those with genetic abnormalities and establish better criteria for management of patients with varicocele.
Conclusions
The adolescent with varicocele presents the clinician with an interesting and challenging problem. There is a great need for further basic research to help better select patients who need surgical correction of varicocele. We have outlined recommendations that can be used in everyday practice. Each clinician needs to make his/her own decisions regarding appropriate candidates, timing, and methods for treatment of adolescents with varicocele.
Main Points.
Varicocele is associated with time-dependent testicular growth arrest and is the most common correctible cause of male infertility.
In adolescent males it is usually asymptomatic, on the left side, and diagnosed during routine physical examination.
Testicular growth arrest with a volume difference of >2 mL assessed by ultrasonography is currently the best indicator of testicular damage and should serve as the minimal requirement for surgical repair of the adolescent varicocele.
Varicocelectomy can reverse growth arrest in adolescents (and may prevent future infertility).
Laparoscopic varicocelectomy should not be used in adolescents. Although the high retroperitoneal ligation of the testicular artery and veins is the treatment of choice in adolescents, pediatric urologists should consider using microscopic inguinal or subinguinal repair with arterial preservation.
Clinical tests currently establish criteria for repair, and there is need for a test to distinguish between adolescents with varicocele who will develop infertility and those who will remain fertile.
References
- 1.Skoog SJ, Roberts KP, Goldstein M, Pryor JL. The adolescent varicocele: what’s new with an old problem in young patients? Pediatrics. 1997;100:112–121. doi: 10.1542/peds.100.1.112. [DOI] [PubMed] [Google Scholar]
- 2.Buch JP, Cromie WJ. Evaluation and treatment of the preadolescent varicocele. Urol Clin North Am. 1985;12:3–12. [PubMed] [Google Scholar]
- 3.Vasavada S, Ross J, Nasrallah P, Kay R. Prepubertal varicoceles. Urology. 1997;50:774–777. doi: 10.1016/S0090-4295(97)00332-4. [DOI] [PubMed] [Google Scholar]
- 4.Lund L, Rasmussen HH, Ernst E. Asymptomatic varicocele testis. Scand J Urol Nephrol. 1993;27:395–398. doi: 10.3109/00365599309180452. [DOI] [PubMed] [Google Scholar]
- 5.Niedzielski J, Paduch D, Raczynski P. Assessment of adolescent varicocele. Pediatr Surg Int. 1997;12:410–413. doi: 10.1007/BF01076952. [DOI] [PubMed] [Google Scholar]
- 6.Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril. 1993;59:613–616. [PubMed] [Google Scholar]
- 7.Goldstein M. New insights into the etiology and treatment of male infertility. J Urol. 1997;158:1808–1809. doi: 10.1016/s0022-5347(01)64135-1. Editorial;Comment. [DOI] [PubMed] [Google Scholar]
- 8.The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. World Health Organization. 1992;57:1289–1293. Fertil Steril. [PubMed] [Google Scholar]
- 9.Belloli G, S DA, Pesce C, Fantuz E. Varicocele in childhood and adolescence and other testicular anomalies: an epidemiological study. Pediatr Med Chir. 1993;15:159–162. [PubMed] [Google Scholar]
- 10.Paduch DA, Niedzielski J. Repair versus observation in adolescent varicocele: a prospective study. J Urol. 1997;158:1128–1132. doi: 10.1097/00005392-199709000-00111. [DOI] [PubMed] [Google Scholar]
- 11.Kass EJ, Reitelman C. Adolescent varicocele. Urol Clin North Am. 1995;22:151–159. [PubMed] [Google Scholar]
- 12.Atassi O, Kass EJ, Steinert BW. Testicular growth after successful varicocele correction in adolescents: comparison of artery sparing techniques with the Palomo procedure [see comments] J Urol. 1995;153:482–483. doi: 10.1097/00005392-199502000-00065. [DOI] [PubMed] [Google Scholar]
- 13.Lenzi A, Gandini L, Bagolan P, et al. Sperm parameters after early left varicocele treatment. Fertil Steril. 1998;69:347–349. doi: 10.1016/s0015-0282(97)00474-3. [DOI] [PubMed] [Google Scholar]
- 14.Meacham RB, Townsend RR, Rademacher D, Drose JA. The incidence of varicoceles in the general population when evaluated by physical examination, gray scale sonography and color Doppler sonography. J Urol. 1994;151:1535–1538. doi: 10.1016/s0022-5347(17)35295-3. [DOI] [PubMed] [Google Scholar]
- 15.Di Cataldo A, Trombatore G, Di Carlo I, et al. Idiopathic varicocele: incidence in 517 subjects. Minerva Chir. 1990;45:485–487. [PubMed] [Google Scholar]
- 16.Pryor JL, Howards SS. Varicocele. Urol Clin North Am. 1987;14:499–513. [PubMed] [Google Scholar]
- 17.Opitz JM, Shapiro SS, Uehling DT. Genetic causes and workup of male and female infertility. 3. Details of the clinical evaluation. Postgrad Med. 1979;66:129–136. doi: 10.1080/00325481.1979.11715204. [DOI] [PubMed] [Google Scholar]
- 18.Nashan D, Behre HM, Grunert JH, Nieschlag E. Diagnostic value of scrotal sonography in infertile men: report on 658 cases. Andrologia. 1990;22:387–395. doi: 10.1111/j.1439-0272.1990.tb02013.x. [DOI] [PubMed] [Google Scholar]
- 19.Jarow JP, Coburn M, Sigman M. Incidence of varicoceles in men with primary and secondary infertility. Urology. 1996;47:73–76. doi: 10.1016/s0090-4295(99)80385-9. [DOI] [PubMed] [Google Scholar]
- 20.Sawczuk IS, Hensle TW, Burbige KA, Nagler HM. Varicoceles: effect on testicular volume in prepubertal and pubertal males. Urology. 1993;41:466–468. doi: 10.1016/0090-4295(93)90510-h. [DOI] [PubMed] [Google Scholar]
- 21.Parrott TS, Hewatt L. Ligation of the testicular artery and vein in adolescent varicocele. J Urol. 1994;152:791–793. doi: 10.1016/s0022-5347(17)32711-8. discussion 793. [DOI] [PubMed] [Google Scholar]
- 22.Mellinger BC. Varicocelectomy. Tech Urol. 1995;1:188–196. [PubMed] [Google Scholar]
- 23.Lechter A, Lopez G, Martinez C, Camacho J. Anatomy of the gonadal veins: a reappraisal. Surgery. 1991;109:735–739. [PubMed] [Google Scholar]
- 24.Beck EM, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol. 1992;148:1190–1194. doi: 10.1016/s0022-5347(17)36857-x. [DOI] [PubMed] [Google Scholar]
- 25.Chatel A, Bigot JM, Dectot H, Helenon C. Radiological anatomy of the spermatic veins. Report of 152 retrograde spermatic phlebographies (author’s transl) J Chir (Paris) 1978;115:443–450. [PubMed] [Google Scholar]
- 26.Wishahi MM. Anatomy of the venous drainage of the human testis: testicular vein cast, microdissection and radiographic demonstration. A new anatomical concept. Eur Urol. 1991;20:154–160. doi: 10.1159/000471687. [DOI] [PubMed] [Google Scholar]
- 27.Campobasso P. Blue venography in adolescent varicocelectomy: a modified surgical approach. J Pediatr Surg. 1997;32:1298–1301. doi: 10.1016/s0022-3468(97)90306-7. [DOI] [PubMed] [Google Scholar]
- 28.Wishahi MM. Detailed anatomy of the internal spermatic vein and the ovarian vein. Human cadaver study and operative spermatic venography: clinical aspects. J Urol. 1991;145:780–784. doi: 10.1016/s0022-5347(17)38450-1. [DOI] [PubMed] [Google Scholar]
- 29.Wishahi MM. Anatomy of the spermatic venous plexus (pampiniform plexus) in men with and without varicocele: intraoperative venographic study. J Urol. 1992;147:1285–1289. doi: 10.1016/s0022-5347(17)37544-4. [DOI] [PubMed] [Google Scholar]
- 30.Shafik A, Moftah A, Olfat S, et al. Testicular veins: anatomy and role in varicocelogenesis and other pathologic conditions. Urology. 1990;35:175–182. doi: 10.1016/0090-4295(90)80071-t. [DOI] [PubMed] [Google Scholar]
- 31.Stassen CM, Weil EH, Janevski BK. Left renal vein compression syndrome (“nutcracker phenomenon“) ROFO Fortschr Geb Rontgenstr Nuklearmed. 1989;150:708–710. doi: 10.1055/s-2008-1047107. [DOI] [PubMed] [Google Scholar]
- 32.Gall H, Rudofsky G, Bahren W, Roth J, Altwein JE. Intravascular pressure measurements and phlebography of the renal vein: a contribution to the etiology of varicocele. Urologe [A] 1987;26:325–330. [PubMed] [Google Scholar]
- 33.Green KF, Turner TT, Howards SS. Varicocele: reversal of the testicular blood flow and temperature effects by varicocele repair. J Urol. 1984;131:1208–1211. doi: 10.1016/s0022-5347(17)50874-5. [DOI] [PubMed] [Google Scholar]
- 34.Nagler HM, Lizza EF, House SD, et al. Testicular hemodynamic changes after the surgical creation of a varicocele in the rat. Intravital microscopic observations. J Androl. 1987;8:292–298. doi: 10.1002/j.1939-4640.1987.tb00964.x. [DOI] [PubMed] [Google Scholar]
- 35.Li H, Dubocq F, Jiang Y, Tiguert R, et al. Effect of surgically induced varicocele on testicular blood flow and Sertoli cell function. Urology. 1999;53:1258–1262. doi: 10.1016/s0090-4295(99)00013-8. [DOI] [PubMed] [Google Scholar]
- 36.Ozbek E, Turkoz Y, Gokdeniz R, Davarci M, Ozugurlu F. Increased nitric oxide production in the spermatic vein of patients with varicocele. Eur Urol. 2000;37:172–175. doi: 10.1159/000020135. [DOI] [PubMed] [Google Scholar]
- 37.Kay R, Alexander NJ, Baugham WL. Induced varicoceles in rhesus monkeys. Fertil Steril. 1979;31:195–199. [PubMed] [Google Scholar]
- 38.Wang R, Chang JS, Zhou XM, Chen DY. Varicocele in the rat: a new experimental model. Effect on histology, ultrastructure and temperature of the testis and the epididymis. Urol Res. 1991;19:319–322. doi: 10.1007/BF00299069. [DOI] [PubMed] [Google Scholar]
- 39.Gazvani MR, Wood SJ, Thomson AJ, et al. Assessment of testicular core temperatures using microwave thermography. Hum Reprod. 2000;15:1723–1726. doi: 10.1093/humrep/15.8.1723. [DOI] [PubMed] [Google Scholar]
- 40.Fujisawa M, Yoshida S, Matsumoto O, et al. Deoxyribonucleic acid polymerase activity in the testes of infertile men with varicocele. Fertil Steril. 1988;50:795–800. doi: 10.1016/s0015-0282(16)60318-7. [DOI] [PubMed] [Google Scholar]
- 41.Fujisawa M, Yoshida S, Matsumoto O, et al. Decrease of topoisomerase I activity in the testes of infertile men with varicocele. Arch Androl. 1988;21:45–50. doi: 10.3109/01485018808986732. [DOI] [PubMed] [Google Scholar]
- 42.Zorgniotti AW. Testis temperature, infertility, and the varicocele paradox. Urology. 1980;16:7–10. doi: 10.1016/0090-4295(80)90321-0. [DOI] [PubMed] [Google Scholar]
- 43.Hienz HA, Voggenthaler J, Weissbach L. Histological findings in testes with varicocele during childhood and their therapeutic consequences. Eur J Pediatr. 1980;133:139–146. doi: 10.1007/BF00441582. [DOI] [PubMed] [Google Scholar]
- 44.Shikone T, Billig H, Hsueh A. Experimentally induced cryptorchidism increases apoptosis in rat testis. Biol Reprod. 1994;51:865–872. doi: 10.1095/biolreprod51.5.865. [DOI] [PubMed] [Google Scholar]
- 45.Harrison RM, Lewis RW, Roberts JA. Testicular blood flow and fluid dynamics in monkeys with surgically induced varicoceles. J Androl. 1983;4:256–260. doi: 10.1002/j.1939-4640.1983.tb02363.x. [DOI] [PubMed] [Google Scholar]
- 46.Saypol DC, Howards SS, Turner TT, Miller ED., Jr Influence of surgically induced varicocele on testicular blood flow, temperature, and histology in adult rats and dogs. J Clin Invest. 1981;68:39–45. doi: 10.1172/JCI110252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sweeney TE, Rozum JS, Gore RW. Alteration of testicular microvascular pressures during venous pressure elevation. Am J Physiol. 1995;269:H37–H45. doi: 10.1152/ajpheart.1995.269.1.H37. [DOI] [PubMed] [Google Scholar]
- 48.Santamaria L, Martin R, Nistal M, Paniagua R. The peritubular myoid cells in the testes from men with varicocele: an ultrastructural, immunohistochemical and quantitative study. Histopathology. 1992;21:423–433. doi: 10.1111/j.1365-2559.1992.tb00426.x. [DOI] [PubMed] [Google Scholar]
- 49.Ibrahim AA, Hamada TA, Moussa MM. Effect of varicocele on sperm respiration and metabolism. Andrologia. 1981;13:253–259. doi: 10.1111/j.1439-0272.1981.tb00044.x. [DOI] [PubMed] [Google Scholar]
- 50.Sharma RK, Agarwal A. Role of reactive oxygen species in male infertility. Urology. 1996;48:835–850. doi: 10.1016/s0090-4295(96)00313-5. [DOI] [PubMed] [Google Scholar]
- 51.Mali WP, Arndt JW, Coolsaet BL, et al. Haemodynamic aspects of left-sided varicocele and its association with so-called right-sided varicocele. Int J Androl. 1984;7:297–308. doi: 10.1111/j.1365-2605.1984.tb00787.x. [DOI] [PubMed] [Google Scholar]
- 52.Mali WP, Oei HY, Arndt JW, et al. Hemodynamics of the varicocele. Part II. Correlation among the results of renocaval pressure measurements, varicocele scintigraphy and phlebography. J Urol. 1986;135:489–493. doi: 10.1016/s0022-5347(17)45701-6. [DOI] [PubMed] [Google Scholar]
- 53.Mali WP, Oei HY, Arndt JW, et al. Hemodynamics of the varicocele. Part I. Correlation among the clinical, phlebographic and scintigraphic findings. J Urol. 1986;135:483–488. doi: 10.1016/s0022-5347(17)45700-4. [DOI] [PubMed] [Google Scholar]
- 54.Turner TT, Lopez TJ. Effects of experimental varicocele require neither adrenal contribution nor venous reflux. J Urol. 1989;142:1372–1375. doi: 10.1016/s0022-5347(17)39102-4. [DOI] [PubMed] [Google Scholar]
- 55.Sofikitis N, Miyagawa I. Left adrenalectomy in varicocelized rats does not inhibit the development of varicocele-related physiologic alterations. Int J Fertil Menopausal Stud. 1993;38:250–255. [PubMed] [Google Scholar]
- 56.York JP, Klump R, Smith JJ, Drago JR. The role of the adrenal in the rat varicocele model. In Vivo. 1990;4:145–147. [PubMed] [Google Scholar]
- 57.Steeno O, Koumans J, De Moor P. Adrenal cortical hormones in the spermatic vein of 95 patients with left varicocele. Andrologia. 1976;8:101–104. doi: 10.1111/j.1439-0272.1976.tb02118.x. [DOI] [PubMed] [Google Scholar]
- 58.Su LM, Goldstein M, Schlegel PN. The effect of varicocelectomy on serum testosterone levels in infertile men with varicoceles. J Urol. 1995;154:1752–1755. [PubMed] [Google Scholar]
- 59.Hampl R, Lachman M, Novak Z, et al. Serum levels of steroid hormones in men with varicocele and oligospermia as compared to normozoospermic men. Exp Clin Endocrinol. 1992;100:117–119. doi: 10.1055/s-0029-1211189. [DOI] [PubMed] [Google Scholar]
- 60.Rajfer J, Turner TT, Rivera F, et al. Inhibition of testicular testosterone biosynthesis following experimental varicocele in rats. Biol Reprod. 1987;36:933–937. doi: 10.1095/biolreprod36.4.933. [DOI] [PubMed] [Google Scholar]
- 61.Ando S, Giacchetto C, Beraldi E, et al. Testosterone and dihydrotestosterone seminal plasma levels in varicocele patients. Acta Eur Fertil. 1982;13:113–117. [PubMed] [Google Scholar]
- 62.Ando A, Giacchetto C, Beraldi E, et al. The influence of age on Leydig cell function in patients with varicocele. Int J Androl. 1984;7:104–118. doi: 10.1111/j.1365-2605.1984.tb00766.x. [DOI] [PubMed] [Google Scholar]
- 63.Ando S, Giacchetto C, Colpi G, et al. Physiopathologic aspects of Leydig cell function in varicocele patients. J Androl. 1984;5:163–170. doi: 10.1002/j.1939-4640.1984.tb02388.x. [DOI] [PubMed] [Google Scholar]
- 64.Ando S, Giacchetto C, Beraldi E, et al. Progesterone, 17-OH-progesterone, androstenedione and testosterone plasma levels in spermatic venous blood of normal men and varicocele patients. Horm Metab Res. 1985;17:99–103. doi: 10.1055/s-2007-1013461. [DOI] [PubMed] [Google Scholar]
- 65.Ando S, Giacchetto C, Colpi GM, et al. Testosterone precursors in spermatic venous blood of normal men and varicocele patients. A study of delta 4 pathway of testosterone biosynthesis. Acta Endocrinol (Copenh) 1985;108:277–283. doi: 10.1530/acta.0.1080277. [DOI] [PubMed] [Google Scholar]
- 66.Swerdloff RS, Walsh PC. Pituitary and gonadal hormones in patients with varicocele. Fertil Steril. 1975;26:1006–1012. doi: 10.1016/s0015-0282(16)41416-0. [DOI] [PubMed] [Google Scholar]
- 67.Kass EJ, Freitas JE, Bour JB. Adolescent varicocele: objective indications for treatment. J Urol. 1989;142:579–582. doi: 10.1016/s0022-5347(17)38822-5. discussion 603–605. [DOI] [PubMed] [Google Scholar]
- 68.Bickel A, Dickstein G. Factors predicting the outcome of varicocele repair for subfertility: the value of the luteinizing hormone-releasing hormone test. J Urol. 1989;142:1230–1234. doi: 10.1016/s0022-5347(17)39040-7. [DOI] [PubMed] [Google Scholar]
- 69.McFadden MR, Mehan DJ. Testicular biopsies in 101 cases of varicocele. J Urol. 1978;119:372–374. doi: 10.1016/s0022-5347(17)57494-7. [DOI] [PubMed] [Google Scholar]
- 70.Hadziselimovic F, Leibundgut B, Da Rugna D, Buser MW. The value of testicular biopsy in patients with varicocele. J Urol. 1986;135:707–710. doi: 10.1016/s0022-5347(17)45826-5. [DOI] [PubMed] [Google Scholar]
- 71.Sirvent JJ, Bernat R, Navarro MA, et al. Leydig cell in idiopathic varicocele. Eur Urol. 1990;17:257–261. doi: 10.1159/000464051. [DOI] [PubMed] [Google Scholar]
- 72.Sofikitis N, Takahashi C, Kadowaki H, et al. Surgical repair versus medical treatment of varicocele in the rat: pharmacological manipulation of the varicocelized testicle. Eur Urol. 1992;22:44–52. doi: 10.1159/000474720. [DOI] [PubMed] [Google Scholar]
- 73.Cayan S, Kadioglu A, Orhan I, et al. The effect of microsurgical varicocelectomy on serum follicle stimulating hormone, testosterone and free testosterone levels in infertile men with varicocele. BJU Int. 1999;84:1046–9. doi: 10.1046/j.1464-410x.1999.00353.x. [DOI] [PubMed] [Google Scholar]
- 74.Plymate SR, Paulsen CA, McLachlan RI. Relationship of serum inhibin levels to serum follicle stimulating hormone and sperm production in normal men and men with varicoceles [published erratum appears in J Clin Endocrinol Metab 1992 Oct;75(4):1059] J Clin Endocrinol Metab. 1992;74:859–864. doi: 10.1210/jcem.74.4.1548351. [DOI] [PubMed] [Google Scholar]
- 75.Cameron DF, Snydle FE. The blood-testis barrier in men with varicocele: a lanthanum tracer study. Fertil Steril. 1980;34:255–258. doi: 10.1016/s0015-0282(16)44958-7. [DOI] [PubMed] [Google Scholar]
- 76.Cameron DF, Snydle FE, Ross MH, Drylie DM. Ultrastructural alterations in the adluminal testicular compartment in men with varicocele. Fertil Steril. 1980;33:526–33. doi: 10.1016/s0015-0282(16)44719-9. [DOI] [PubMed] [Google Scholar]
- 77.Cameron DF, Snydle FE. Ultrastructural surface characteristics of seminiferous tubules from men with varicocele. Andrologia. 1982;14:425–433. doi: 10.1111/j.1439-0272.1982.tb02287.x. [DOI] [PubMed] [Google Scholar]
- 78.Ramanujam LN, Liao WX, Roy AC, Ng SC. Association of molecular variants of luteinizing hormone with male infertility. Hum Reprod. 2000;15:925. doi: 10.1093/humrep/15.4.925. [DOI] [PubMed] [Google Scholar]
- 79.Carreau S. Paracrine control of human Leydig cell and Sertoli cell functions. Folia Histochem Cytobiol. 1996;34:111–119. [PubMed] [Google Scholar]
- 80.Schlatt S, Meinhardt A, Nieschlag E. Paracrine regulation of cellular interactions in the testis: factors in search of a function. Eur J Endocrinol. 1997;137:107–117. doi: 10.1530/eje.0.1370107. [DOI] [PubMed] [Google Scholar]
- 81.Schlatt S, Arslan M, Weinbauer GF, et al. Endocrine control of testicular somatic and premeiotic germ cell development in the immature testis of the primate Macaca mulatta. Eur J Endocrinol. 1995;133:235–247. doi: 10.1530/eje.0.1330235. [DOI] [PubMed] [Google Scholar]
- 82.Lee J, Richbug JH, Younkin SC, Boekelheide K. The Fas system is a key regulator of germ cell apoptosis in the testis. Endocrinology. 1997;138:2081–2088. doi: 10.1210/endo.138.5.5110. [DOI] [PubMed] [Google Scholar]
- 83.Mather JP, Moore A, Li RH. Activins, inhibins, and follistatins: further thoughts on a growing family of regulators. Proc Soc Exper Biol Med. 1997;215:209–222. doi: 10.3181/00379727-215-44130. [DOI] [PubMed] [Google Scholar]
- 84.Boujrad N, Hochereau-de Reviers MT, Carreau S. Evidence for germ cell control of Sertoli cell function in three models of germ cell depletion in adult rat. Biol Reprod. 1995;53:1345–1352. doi: 10.1095/biolreprod53.6.1345. [DOI] [PubMed] [Google Scholar]
- 85.Yan YC, Sun YP, Zhang ML. Testis epidermal growth factor and SP. Arch Androl. 1998;40:133–146. doi: 10.3109/01485019808987936. [DOI] [PubMed] [Google Scholar]
- 86.Ergun S, Kilic N, Fiedler W, Mukhopadhyay AK. Vascular endothelial growth factor and its receptors in normal human testicular tissue. Mol Cell Endocrinol. 1997;131:9–20. doi: 10.1016/s0303-7207(97)00082-8. [DOI] [PubMed] [Google Scholar]
- 87.Seidl K, Buchberger A, Erck C. Expression of nerve growth factor and neurotrophin receptors in testicular cells suggest novel roles for neurotrophins outside the nervous system. Reprod Fertil Dev. 1996;8:1075–1087. doi: 10.1071/rd9961075. [DOI] [PubMed] [Google Scholar]
- 88.Kostic T, Andric S, Kovacevic R, Maric D. The effect of opioid antagonists in local regulation of testicular response to acute stress in adult rats. Steroids. 1997;62:703–708. doi: 10.1016/s0039-128x(97)00071-8. [DOI] [PubMed] [Google Scholar]
- 89.Bablok L, Fracki S, Wielgos M, et al. The naloxone test in patients with varicocele. Ginekol Pol. 1998;69:380–384. [PubMed] [Google Scholar]
- 90.Barbieri ER, Hidalgo ME, Venegas A, et al. Varicocele-associated decrease in antioxidant defenses. J Androl. 1999;20:713–717. [PubMed] [Google Scholar]
- 91.Hendin BN, Kolettis PN, Sharma RK, et al. Varicocele is associated with elevated spermatozoal reactive oxygen species production and diminished seminal plasma antioxidant capacity. J Urol. 1999;161:1831–1834. [PubMed] [Google Scholar]
- 92.Micic S, Illic V, Isvaneski M. Correlation of hormone and histologic parameters in infertile men with varicocele. Urol Int. 1983;38:187–190. doi: 10.1159/000280888. [DOI] [PubMed] [Google Scholar]
- 93.Paduch DA, Niedzielski J. Semen analysis in young men with varicocele: preliminary study. J Urol. 1996;156:788–790. doi: 10.1097/00005392-199608001-00063. [DOI] [PubMed] [Google Scholar]
- 94.Nagao RR, Plymate SR, Berger RE, et al. Comparison of gonadal function between fertile and infertile men with varicoceles. Fertil Steril. 1986;46:930–933. [PubMed] [Google Scholar]
- 95.Lyon RP, Marshall S, Scott MP. Varicocele in childhood and adolescence: implication in adulthood infertility? Urology. 1982;19:641–644. doi: 10.1016/0090-4295(82)90019-x. [DOI] [PubMed] [Google Scholar]
- 96.Lipshultz LI, Corriere JN., Jr Progressive testicular atrophy in the varicocele patient. J Urol. 1977;117:175–176. doi: 10.1016/s0022-5347(17)58387-1. [DOI] [PubMed] [Google Scholar]
- 97.Witt MA, Lipshultz LI. Varicocele: a progressive or static lesion? Urology. 1993;42:541–543. doi: 10.1016/0090-4295(93)90268-f. [DOI] [PubMed] [Google Scholar]
- 98.Handelsman DJ, Conway AJ, Boylan LM, Turtle JR. Testicular function in potential sperm donors: normal ranges and the effects of smoking and varicocele. Int J Androl. 1984;7:369–382. doi: 10.1111/j.1365-2605.1984.tb00794.x. [DOI] [PubMed] [Google Scholar]
- 99.Hadziselimovic F, Herzog B, Jenny P. The chance for fertility in adolescent boys after corrective surgery for varicocele. J Urol. 1995;154:731–733. doi: 10.1097/00005392-199508000-00106. [DOI] [PubMed] [Google Scholar]
- 100.Aragona F, Ragazzi R, Pozzan GB, et al. Correlation of testicular volume, histology and LHRH test in adolescents with idiopathic varicocele. Eur Urol. 1994;26:61–66. doi: 10.1159/000475344. [DOI] [PubMed] [Google Scholar]
- 101.Ponchietti R, Grechi G, Dini G. Varicocele in adolescents: ultrastructural aspects. Acta Eur Fertil. 1986;17:47–50. [PubMed] [Google Scholar]
- 102.Kass EJ, Chandra RS, Belman AB. Testicular histology in the adolescent with a varicocele. Pediatrics. 1987;79:996–998. [PubMed] [Google Scholar]
- 103.Castro-Magana M, Angulo M, Canas A, Uy J. Leydig cell function in adolescent boys with varicoceles. Arch Androl. 1990;24:73–79. doi: 10.3109/01485019008986861. [DOI] [PubMed] [Google Scholar]
- 104.Hadziselimovic F. Testicular and vascular changes in patients with varicocele. Acta Urol Belg. 1995;63:51–54. [PubMed] [Google Scholar]
- 105.Chakraborty J, Hikim AP, Jhunjhunwala JS. Stagnation of blood in the microcirculatory vessels in the testes of men with varicocele. J Androl. 1985;6:117–126. doi: 10.1002/j.1939-4640.1985.tb00826.x. [DOI] [PubMed] [Google Scholar]
- 106.Santoro G, Romeo C, Impellizzeri P, et al. Ultrastructural and immunohistochemical study of basal lamina of the testis in adolescent varicocele. Fertil Steril. 2000;73:699–705. doi: 10.1016/s0015-0282(99)00611-1. [DOI] [PubMed] [Google Scholar]
- 107.Romeo C, Santoro G, Impellizzeri P, et al. Myofibroblasts in adolescent varicocele: an ultrastructural and immunohistochemical study. Uroll Res. 2000;28:24–28. doi: 10.1007/s002400050005. [DOI] [PubMed] [Google Scholar]
- 108.Papanikolaou F, Chow V, Jarvi K, et al. Effect of adult microsurgical varicocelectomy on testicular volume. Urology. 2000 Jul;56:136–139. doi: 10.1016/s0090-4295(00)00535-5. [DOI] [PubMed] [Google Scholar]
- 109.Uygur MC, Arik AI, Erol D, et al. Quantitative evaluation of biopsy gun testis needle biopsy. Correlation between biopsy score of varicocelebearing testis and sperm count. J Reprod Med. 1999;44:445–449. [PubMed] [Google Scholar]
- 110.Tanji N, Fujiwara T, Kaji H, et al. Histologic evaluation of spermatic veins in patients with varicocele. Int J Urol. 1999;6:355–360. doi: 10.1046/j.1442-2042.1999.00076.x. [DOI] [PubMed] [Google Scholar]
- 111.Roy CR, Wilson T, Raife M, Horne D. Varicocele as the presenting sign of an abdominal mass. J Urol. 1989;141:597–599. doi: 10.1016/s0022-5347(17)40906-2. [DOI] [PubMed] [Google Scholar]
- 112.Behre HM, Nashan D, Nieschlag E. Objective measurement of testicular volume by ultrasonography. Int J Androl. 1989;12:395–403. doi: 10.1111/j.1365-2605.1989.tb01328.x. [DOI] [PubMed] [Google Scholar]
- 113.Costabile RA, Skoog S, Radowich M. Testicular volume assessment in the adolescent with a varicocele. J Urol. 1992;147:1348–1350. doi: 10.1016/s0022-5347(17)37561-4. [DOI] [PubMed] [Google Scholar]
- 114.Diamond DA, Paltiel HJ, DiCanzio J, et al. Comparative assessment of pediatric testicular volume: orchidometer versus ultrasound. J Urol. 2000;164:1111–1114. doi: 10.1097/00005392-200009020-00048. [DOI] [PubMed] [Google Scholar]
- 115.Gentile DP, Cockett AT. The effect of varicocelectomy on testicular volume in 89 infertile adult males with varicoceles. Fertil Steril. 1992;58:209–211. doi: 10.1016/s0015-0282(16)55165-6. [DOI] [PubMed] [Google Scholar]
- 116.Steeno O, Knops J, Declerck L, et al. Prevention of fertility disorders by detection and treatment of varicocele at school and college age. Andrologia. 1976;8:47–53. doi: 10.1111/j.1439-0272.1976.tb01645.x. [DOI] [PubMed] [Google Scholar]
- 117.Yamamoto M, Hibi H, Katsuno S, Miyake K. Effects of varicocelectomy on testis volume and semen parameters in adolescents: a randomized prospective study. Nagoya J Med Sci. 1995;58:127–132. [PubMed] [Google Scholar]
- 118.Laven JS, Haans LC, Mali WP, et al. Effects of varicocele treatment in adolescents: a randomized study. Fertil Steril. 1992;58:756–762. doi: 10.1016/s0015-0282(16)55324-2. [DOI] [PubMed] [Google Scholar]
- 119.Greenberg SH, Lipshultz LI, Wein AJ. Experience with 425 subfertile male patients. J Urol. 1978;119:507–510. doi: 10.1016/s0022-5347(17)57531-x. [DOI] [PubMed] [Google Scholar]
- 120.Kass EJ, Belman AB. Reversal of testicular growth failure by varicocele ligation. J Urol. 1987;137:475–476. doi: 10.1016/s0022-5347(17)44072-9. [DOI] [PubMed] [Google Scholar]
- 121.Okuyama A, Nakamura M, Namiki M, et al. Surgical repair of varicocele at puberty: preventive treatment for fertility improvement [see comments] J Urol. 1988;139:562–564. doi: 10.1016/s0022-5347(17)42525-0. [DOI] [PubMed] [Google Scholar]
- 122.Haans LC, Laven JS, Mali WP, et al. Testis volumes, semen quality, and hormonal patterns in adolescents with and without a varicocele. Fertil Steril. 1991;56:731–736. doi: 10.1016/s0015-0282(16)54607-x. [DOI] [PubMed] [Google Scholar]
- 123.Sayfan J, Siplovich L, Koltun L, Benyamin N. Varicocele treatment in pubertal boys prevents testicular growth arrest. J Urol. 1997;157:1456–1457. [PubMed] [Google Scholar]
- 124.Lund L, Larsen SB. A follow-up study of semen quality and fertility in men with varicocele testis and in control subjects. Br J Urol. 1998;82:682–686. doi: 10.1046/j.1464-410x.1998.00850.x. [DOI] [PubMed] [Google Scholar]
- 125.Vereecken RL, Boeckx G. Does fertility improvement after varicocele treatment justify preventive treatment at puberty? Urology. 1986;28:122–126. doi: 10.1016/0090-4295(86)90102-0. [DOI] [PubMed] [Google Scholar]
- 126.Hudson RW, McKay DE. The gonadotropin response of men with varicoceles to gonadotropin-releasing hormone. Fertil Steril. 1980;33:427–432. [PubMed] [Google Scholar]
- 127.Hudson RW, Crawford VA, McKay DE. The gonadotropin response of men with varicoceles to a four-hour infusion of gonadotropin-releasing hormone. Fertil Steril. 1981;36:633–637. [PubMed] [Google Scholar]
- 128.Haidl G, Maass C, Schill WB. When to treat varicocele? Acta Chir Hung. 1994;34:309–314. [PubMed] [Google Scholar]
- 129.Hudson RW. The endocrinology of varicoceles. Fertil Steril. 1988;49:199–208. doi: 10.1016/s0015-0282(16)59700-3. [DOI] [PubMed] [Google Scholar]
- 130.Osuna JA, Lozano JR, Cruz I, Tortolero I. Pituitary and testicular function in adolescents with varicocele. Arch Androl. 1999;43:183–188. doi: 10.1080/014850199262472. [DOI] [PubMed] [Google Scholar]
- 131.Kass EJ, Freitas JE, Salisz JA, Steinert BW. Pituitary gonadal dysfunction in adolescents with varicocele [see comments] Urology. 1993;42:179–181. doi: 10.1016/0090-4295(93)90643-o. [DOI] [PubMed] [Google Scholar]
- 132.Foppiani L, Piredda S, Cavani S, et al. Gonadotropin response to GnRH and seminal parameters in low grade varicocele. Arch Ital Urol Androl. 1999;71:7–12. [PubMed] [Google Scholar]
- 133.Winkelbauer F, Karnel F, Ammann ME, Hofbauer J. Ultrasound diagnosis of persistent varicocele after sclerotherapy. Ultraschall Med. 1994;15:29–32. doi: 10.1055/s-2007-1004001. [DOI] [PubMed] [Google Scholar]
- 134.Aydos K, Baltaci S, Salih M, et al. Use of color Doppler sonography in the evaluation of varicoceles. Eur Urol. 1993;24:221–225. doi: 10.1159/000474298. [DOI] [PubMed] [Google Scholar]
- 135.Bohring C, Krause W. Serum levels of inhibin B in men with different causes of spermatogenic failure. Andrologia. 1999;31:137–141. [PubMed] [Google Scholar]
- 136.Carrillo A, Gershbein A, Glassberg KI, Danon M. Serum inhibin B levels and the response to gonadotropin stimulation test in pubertal boys with varicocele. J Urol. 1999;162:875–877. doi: 10.1097/00005392-199909010-00081. [DOI] [PubMed] [Google Scholar]
- 137.Pryor JP, Pugh RC, Cameron KM, et al. Plasma gonadotrophic hormones, testicular biopsy and seminal analysis in the men of infertile marriages. Br J Urol. 1976;48:709–717. doi: 10.1111/j.1464-410x.1976.tb06724.x. [DOI] [PubMed] [Google Scholar]
- 138.Baccetti B, Burrini AG, Capitani S, et al. Studies on varicocele. II. The inhibin secretion. J Submicrosc Cytol Pathol. 1993;25:137–44. [PubMed] [Google Scholar]
- 139.Baccetti B, Burrini AG, Capitani S, et al. Studies on varicocele. 1. Submicroscopical and endocrinological features. J Submicrosc Cytol Pathol. 1991;23:659–665. [PubMed] [Google Scholar]
- 140.Radicioni A, Schwarzenberg TL. The use of FSH in adolescents and young adults with idiopathic, unilateral, left varicocele not undergoing surgical intervention. Preliminary study. Minerva Endocrinol. 1999;24:63–68. [PubMed] [Google Scholar]
- 141.Zini A, Defreitas G, Freeman M, et al. Varicocele is associated with abnormal retention of cytoplasmic droplets by human spermatozoa. Fertil Steril. 2000;74:461–464. doi: 10.1016/s0015-0282(00)00703-2. [DOI] [PubMed] [Google Scholar]
- 142.Zini A, Buckspan M, Jamal M, Jarvi K. Effect of varicocelectomy on the abnormal retention of residual cytoplasm by human spermatozoa. Hum Reprod. 1999;14:1791–1793. doi: 10.1093/humrep/14.7.1791. [DOI] [PubMed] [Google Scholar]
- 143.Reichart M, Eltes F, Soffer Y, et al. Sperm ultramorphology as a pathophysiological indicator of SP in males suffering from varicocele [In Process Citation] Andrologia. 2000 May;32:139–45. doi: 10.1046/j.1439-0272.2000.00355.x. [DOI] [PubMed] [Google Scholar]
- 144.Bouchot O, Prunet D, Gaschignard N, Buzelin JM. Surgery of varicocele: results concerning sperm motility and morphology. Prog Urol. 1999;9:703–706. [PubMed] [Google Scholar]
- 145.Bartoov B, Eltes F, Reichart M, et al. Quantitative ultramorphological analysis of human sperm: fifteen years of experience in the diagnosis and management of male factor infertility. Arch Androl. 1999;43:13–25. doi: 10.1080/014850199262698. [DOI] [PubMed] [Google Scholar]
- 146.Bartoov B, Eltes F, Reichart M, et al. Quantitative ultramorphological (QUM) analysis of human sperm: diagnosis and management of male infertility. Arch Androl. 1999;42:161–177. doi: 10.1080/014850199262823. [DOI] [PubMed] [Google Scholar]
- 147.Kass EJ, Marcol B. Results of varicocele surgery in adolescents: a comparison of techniques. J Urol. 1992;148:694–696. doi: 10.1016/s0022-5347(17)36696-x. [DOI] [PubMed] [Google Scholar]
- 148.Lund L, Roebuck DJ, Lee KH, et al. Clinical assessment after varicocelectomy. Scand J Urol Nephrol. 2000;34:119–122. doi: 10.1080/003655900750016733. [DOI] [PubMed] [Google Scholar]
- 149.Allouch G. Varicocele in adolescents. 67 cases. J Urol (Paris) 1996;102:62–65. [PubMed] [Google Scholar]
- 150.Palmer LS, Maizels M, Kaplan WE, et al. The influence of surgical approach and intraoperative venography on successful varicocelectomy in adolescents. J Urol. 1997;158:1201–1204. doi: 10.1097/00005392-199709000-00135. [DOI] [PubMed] [Google Scholar]
- 151.Lund L, Tang YC, Roebuck D, et al. Testicular catch-up growth after varicocele correction in adolescents. Pediatr Surg Int. 1999;15:234–237. doi: 10.1007/s003830050564. [DOI] [PubMed] [Google Scholar]
- 152.Nagar H, Mabjeesh NJ. Decision-making in pediatric varicocele surgery: use of color Doppler ultrasound. Pediatr Surg Int. 2000;16:75–76. doi: 10.1007/s003830050020. [DOI] [PubMed] [Google Scholar]
- 153.Salerno S, Cannizzaro F, Lo Casto A, et al. Anastomosis between the left internal spermatic and splanchnic veins. Retrospective analysis of 305 patients. Radiol Med. 2000;99:347–351. [PubMed] [Google Scholar]
- 154.Niedzielski J, Paduch DA. Recurrence of varicocele after high retroperitoneal repair: implications of intraoperative venography. J Urol. 2001;165:837–940. [PubMed] [Google Scholar]
- 155.Marmar JL, Kim Y. Subinguinal microsurgical varicocelectomy: a technical critique and statistical analysis of semen and pregnancy data. J Urol. 1994;152:1127–1132. doi: 10.1016/s0022-5347(17)32521-1. [DOI] [PubMed] [Google Scholar]
- 156.Goldstein M, Gilbert BR, Dicker AP, et al. Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique. J Urol. 1992;148:1808–1811. doi: 10.1016/s0022-5347(17)37035-0. [DOI] [PubMed] [Google Scholar]
- 157.Chalouhy E, Kassardjian Z, Merhej S, et al. Microsurgical high inguinal varicocelectomy with delivery of the testis. J Med Liban. 1994;42:105–108. [PubMed] [Google Scholar]
- 158.Minevich E, Wacksman J, Lewis AG, Sheldon CA. Inguinal microsurgical varicocelectomy in the adolescent: technique and preliminary results. J Urol. 1998;159:1022–1024. [PubMed] [Google Scholar]
- 159.Becmeur F, Sauvage P. Should varicoceles be treated in the adolescent? How? J Chir (Paris) 1999;136:93–96. [PubMed] [Google Scholar]
- 160.Lemack GE, Uzzo RG, Schlegel PN, Goldstein M. Microsurgical repair of the adolescent varicocele. J Urol. 1998;160:179–181. [PubMed] [Google Scholar]
- 161.Lima M, Domini M, Libri M. The varicocele in pediatric age: 207 cases treated with microsurgical technique. Eur J Pediatr Surg. 1997;7:30–33. doi: 10.1055/s-2008-1071044. [DOI] [PubMed] [Google Scholar]
- 162.Cayan S, Kadioglu TC, Tefekli A, et al. Comparison of results and complications of high ligation surgery and microsurgical high inguinal varicocelectomy in the treatment of varicocele. Urology. 2000;55:750–754. doi: 10.1016/s0090-4295(99)00603-2. [DOI] [PubMed] [Google Scholar]
- 163.Ulker V, Garibyan H, Kurth KH. Comparison of inguinal and laparoscopic approaches in the treatment of varicocele. Int Urol Nephrol. 1997;29:71–77. doi: 10.1007/BF02551420. [DOI] [PubMed] [Google Scholar]
- 164.al-Shareef ZH, Koneru SR, al-Tayeb A, et al. Laparoscopic ligation of varicoceles: an anatomically superior operation [see comments] Ann R Coll Surg Engl. 1993;75:345–348. [PMC free article] [PubMed] [Google Scholar]
- 165.Wuernschimmel E, Lipsky H, Noest G. Laparoscopic varicocele ligation: a recommendable standard procedure with good long-term results. Eur Urol. 1995;27:18–22. doi: 10.1159/000475116. [DOI] [PubMed] [Google Scholar]
- 166.Amendolara M, Antoniello L, Battocchio F. Laparoscopic treatment of varicocele. Chir Ital. 1999;51:247–252. [PubMed] [Google Scholar]
- 167.Seibold J, Janetschek G, Bartsch G. Laparoscopic surgery in pediatric urology. Eur Urol. 1996;30:394–399. doi: 10.1159/000474202. [DOI] [PubMed] [Google Scholar]
- 168.Fahlenkamp D, Winfield HN, Schonberger B, et al. Role of laparoscopic surgery in pediatric urology. Eur Urol. 1997;32:75–84. [PubMed] [Google Scholar]
- 169.Humphrey GM, Najmaldin AS. Laparoscopy in the management of pediatric varicoceles. J Pediatr Surg. 1997;32:1470–1472. doi: 10.1016/s0022-3468(97)90565-0. [DOI] [PubMed] [Google Scholar]
- 170.Hirsch IH, Abdel-Meguid TA, Gomella LG. Postsurgical outcomes assessment following varicocele ligation: laparoscopic versus subinguinal approach. Urology. 1998;51:810–815. doi: 10.1016/s0090-4295(97)00709-7. [DOI] [PubMed] [Google Scholar]
- 171.Mandressi A, Buizza C, Antonelli D, Chisena S. Is laparoscopy a worthy method to treat varicocele? Comparison between 160 cases of two-port laparoscopic and 120 cases of open inguinal spermatic vein ligation. J Endourol. 1996;10:435–441. doi: 10.1089/end.1996.10.435. [DOI] [PubMed] [Google Scholar]
- 172.Feneley MR, Pal MK, Nockler IB, Hendry WF. Retrograde embolization and causes of failure in the primary treatment of varicocele. Br J Urol. 1997;80:642–646. doi: 10.1046/j.1464-410x.1997.00407.x. [DOI] [PubMed] [Google Scholar]
- 173.Chalmers N, Hufton AP, Jackson RW, Conway B. Radiation risk estimation in varicocele embolization. Br J Radiol. 2000;73:293–297. doi: 10.1259/bjr.73.867.10817046. [DOI] [PubMed] [Google Scholar]
- 174.Johnsen N, Johnsen I, Tauber R. Semen analysis after treatment of varicocele by antegrade scrotal sclerotherapy. Adv Exp Med Biol. 1997;424:187–188. doi: 10.1007/978-1-4615-5913-9_36. [DOI] [PubMed] [Google Scholar]
- 175.Kuenkel MR, Korth K. Rationale for antegrade sclerotherapy in varicoceles. Eur Urol. 1995;27:13–17. doi: 10.1159/000475115. [DOI] [PubMed] [Google Scholar]
- 176.Johnsen N, Tauber R. Financial analysis of antegrade scrotal sclerotherapy for men with varicoceles. Br J Urol. 1996;77:129–132. doi: 10.1046/j.1464-410x.1996.78622.x. [DOI] [PubMed] [Google Scholar]
- 177.Mottrie AM, Matani Y, Baert J, et al. Antegrade scrotal sclerotherapy for the treatment of varicocele in childhood and adolescence. Br J Urol. 1995;76:21–24. doi: 10.1111/j.1464-410x.1995.tb07825.x. [DOI] [PubMed] [Google Scholar]
- 178.Fette A, Mayr J. Treatment of varicoceles in childhood and adolescence with Tauber’s antegrade scrotal sclerotherapy [In Process Citation] J Pediatr Surg. 2000;35:1222–1225. doi: 10.1053/jpsu.2000.8758. [DOI] [PubMed] [Google Scholar]
- 179.Palmer LS, Cohen S, Reda EF, et al. Intraoperative spermatic venography reconsidered. J Urol. 1995;154:225–227. [PubMed] [Google Scholar]
- 180.Belloli G, D’Agostino S, Musi L, Campobasso P. Adolescent varicocele: operative anatomy and tricks for successful correction. Eur J Pediatr Surg. 1995;5:219–221. doi: 10.1055/s-2008-1066209. [DOI] [PubMed] [Google Scholar]
- 181.Hart RR, Rushton HG, Belman AB. Intraoperative spermatic venography during varicocele surgery in adolescents. J Urol. 1992;148:1514–1516. doi: 10.1016/s0022-5347(17)36953-7. [DOI] [PubMed] [Google Scholar]
- 182.Levitt S, Gill B, Katlowitz N, et al. Routine intraoperative post-ligation venography in the treatment of the pediatric varicocele. J Urol. 1987;137:716–718. doi: 10.1016/s0022-5347(17)44187-5. [DOI] [PubMed] [Google Scholar]
- 183.Zaontz MR, Firlit CF. Use of venography as an aid in varicocelectomy. J Urol. 1987;138:1041–1042. doi: 10.1016/s0022-5347(17)43494-x. [DOI] [PubMed] [Google Scholar]
- 184.Gill B, Kogan SJ, Maldonado J, et al. Significance of intraoperative venographic patterns on the postoperative recurrence and surgical incision placement of pediatric varicoceles. J Urol. 1990;144:502–505. doi: 10.1016/s0022-5347(17)39503-4. discussion 512–513. [DOI] [PubMed] [Google Scholar]
- 185.Seifer I, Amat S, Delgado-Viscogliosi P, et al. Screening for microdeletions on the long arm of chromosome Y in 53 infertile men. Int J Androl. 1999;22:148–154. doi: 10.1046/j.1365-2605.1999.00161.x. [DOI] [PubMed] [Google Scholar]
- 186.Oster J. Varicocele in children and adolescents. Scand J Urol Nephrol. 1971;5:27–32. doi: 10.3109/00365597109133569. [DOI] [PubMed] [Google Scholar]
- 187.Yerokhin A. Classification and frequency of varicocele in children. Klin Khir. 1979;6:45–46. [PubMed] [Google Scholar]
- 188.Dubin L, Amelar RD. Varicocelectomy: twenty-five years of experience. Int J Fertil. 1988;33:226–8. 231–235. [PubMed] [Google Scholar]
- 189.Dahlstrand C, Thune A, Hedelin H, et al. Laparoscopic ligature of the spermatic veins. A comparison between outpatient and hospitalised treatment. Scand J Urol Nephrol. 1994;28:159–162. doi: 10.3109/00365599409180493. [DOI] [PubMed] [Google Scholar]
- 190.Belloli G, Musi L, D’Agostino S. Laparoscopic surgery for adolescent varicocele: preliminary report on 80 patients. J Pediatr Surg. 1996;31:1488–1490. doi: 10.1016/s0022-3468(96)90161-x. [DOI] [PubMed] [Google Scholar]


