Abstract
Urinary incontinence is a significant health problem with considerable social and economic impact. It is important to distinguish between prevalence and incidence with regard to incontinence, and prevalence—the probability of having incontinence within a defined population at a defined point in time—is the more important when considering its impact and the utilization of healthcare resources. There are large variations in the severity and impact of incontinence, and its severity, frequency, and predictability all need to be considered when evaluating its effects on patients, The degree of bother is particularly significant when determining who will need treatment. Incontinence may be a result of bladder dysfunction, sphincter dysfunction, or a combination of both, but large-scale studies are not designed to determine the etiology. In young women, the prevalence of incontinence is usually low, but prevalence peaks around menopause, with a steady rise there-after into later life. Although the prevalence of stress and mixed (stress and urge) incontinence is higher than urge incontinence, the latter is more likely to require treatment. In women, moderate and severe bother have a prevalence ranging from about 3% to 17%. Severe incontinence has a low prevalence in young women, but rapidly increases at ages 70 through 80. In men, the prevalence of incontinence is much lower than in women, about 3% to 11% overall, with urge incontinence accounting for 40% to 80% of all male patients. Stress incontinence accounts for less than 10% of cases and is attributable to prostate surgery, trauma, or neurological injury. Incontinence in men also increases with age, but severe incontinence in 70- to 80-year-old men is about half of that in women. The most effective therapy for incontinence will rely on targeting the correct populations to be treated, which depends on how data is collected on prevalence and severity.
Key words: Incontinence, Urge incontinence, Epidemiology, Etiology, Prevalence, Incidence
Urinary incontinence is a significant health problem in the United States and worldwide. It has a considerable social and economic impact on individuals and society. When discussing the epidemiology and impact of incontinence, it is important to distinguish its between prevalence and incidence.
Prevalence is the probability of having a disease or condition, in this case incontinence, within a defined population at a defined point in time. For example, prevalence would be the number of 60-year-old women in the United States in the year 2001 experiencing the symptom of incontinence.
Incidence, on the other hand, is the probability of developing a disease or condition during a defined period of time. Thus, the percentage of continent women in 2001 that will develop incontinence over the next year would define the incidence of incontinence over a 1-year period.
In most discussions on incontinence, especially when determining social impact and allocation of healthcare resources, prevalence is the more important parameter. Incidence can be important when discussing diseases or treatment where incontinence is a possible outcome, for example, the incidence of incontinence one year after radical prostatectomy or the incidence of incontinence in patients one year after stroke.
Evaluating Incontinence
With a condition such as incontinence it is not only important to know how common it is, but also how many patients with incontinence will actually seek treatment. Severity and impact on quality of life vary greatly. Incontinence varies in degree of severity from several drops to complete bladder emptying. It may occur daily, or many times a day, or only occasionally, perhaps once a month. It may be fairly predictable (low-grade stress incontinence) or totally unpredictable (urge incontinence). These different factors—degree, frequency, and predictability—all play a role in evaluating the effect of incontinence on a particular patient.
The impact of incontinence, or degree of bother, is very important in determining the number of patients who will need treatment. Thus, it is very important to know precisely what is being evaluated and how “incontinence” is defined when reviewing studies on incontinence. The International Continence Society (ICS) defines incontinence as “involuntary loss of urine that is a social or hygienic problem and is objectively demonstrable.” This is different from incontinence that is defined by a person checking off “yes” to a question of “have you ever lost urine involuntarily” on a questionnaire. Although the second may be defined as an incontinence episode, it is not necessarily a social or hygienic problem.
Etiology
There are several different etiologies that underlie the symptom of incontinence. In simple terms, incontinence may be a result of bladder dysfunction, sphincter dysfunction, or a combination of both. Many large studies reporting on the prevalence of incontinence in a specific population do not distinguish between the different types or causes of incontinence. There have been a number of large surveys where questionnaires are the primary tool for evaluating the presence of incontinence. In these studies it is often difficult if not impossible to determine cause of incontinence. Even when patients are asked about specific symptoms, it is necessary to rely on subjective reporting to determine the etiology of incontinence. It is not always easy or accurate to sort out those patients with stress incontinence (sphincteric dysfunction), urge incontinence (bladder dysfunction), or mixed incontinence (both sphincter and bladder dysfunction) based on symptoms alone.
Incontinence in Women
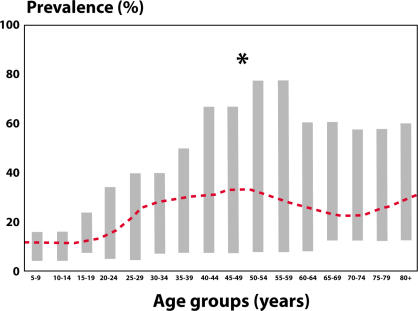
A 1995 review on the prevalence of incontinence in the general population summarized 11 studies conducted with a mixed population of females of various ages and a variety of causes of incontinence.1 Figure 1 shows that the prevalence is relatively low early in life, has a peak around the time of menopause, and then rises steadily between the ages of 60 and 80 years. The prevalence of 10% in 15–19-year-olds and 18% in 20–24-year-olds seems a bit high when one considers the number of young women who actually seek treatment for incontinence. This may be a result of including a large number of young women with “insignificant” or non-bothersome incontinence in the survey.
Figure 1.
Prevalence of incontinence in general population of females reported in 13 different studies. Young adult, 20% to 30%; Middle age, 30% to 40%; Elderly, 30% to 50%. Reprinted from Sandvik,1 with permission.
Many studies have looked at the relative prevalence of stress, urge, and mixed incontinence in specific populations (Table).2–12 The overall prevalence of stress incontinence and mixed incontinence (stress and urge incontinence) is quite high, whereas the overall percentage of urge incontinence is lower. When looking at such data, it is important to consider that although a majority of patients have the symptom of stress incontinence, urge incontinence (including lesser degrees of urge incontinence), tends to be considerably more bothersome than similar degrees of stress incontinence.
Table.
Prevalence Of Stress, Urge And Mixed Incontinence In Women Of Varying Age Groups*
| Author | Age | N | Stress (%) | Urge (%) | Mixed (%) |
|---|---|---|---|---|---|
| Iosif, 19842 | 61 | 912 | 40 | 27 | 33 |
| Hording, 19863 | 45 | 515 | 75 | 11 | 14 |
| Elving, 19894 | 30–59 | 2631 | 48 | 7 | 45 |
| Sommer, 19905 | 20–79 | 414 | 38 | 33 | 45 |
| Harrison, 19946 | 20+ | 314 | 48 | 9 | 44 |
| Yarnell, 19817 | 18+ | 1000 | 50 | 19 | 31 |
| Diokno, 19868 | 60+ | 1995 | 29 | 10 | 61 |
| Holst, 19989 | 18+ | 851 | 52 | 25 | 23 |
| Burgio, 199110 | 42–50 | 541 | 50 | 12 | 38 |
| Lara, 199411 | 18+ | 556 | 48 | 27 | 21 |
| Sandvik, 199512 | 20+ | 1820 | 51 | 10 | 39 |
| Mean (range) | 48 (29–75) | 17 (7–33) | 34 (14–61) |
Reprinted from Hunskaar et al,15 with permission.
Stress Versus Urge Incontinence
Epidemiological studies are usually done on general populations and not necessarily on those seeking treatment. Consequently, the results are not always useful with regard to allocating resources in developing new treatments for incontinence. That is, although the prevalence of low-grade stress incontinence may be high amongst postmenopausal women, often this condition is not bothersome. Urge incontinence may have a somewhat lower prevalence, but is often extremely bothersome. It is this second condition that will more likely require treatment and allocation of healthcare resources. Large studies are also limited by the ability of questionnaires and surveys to accurately predict the etiology of incontinence. Ouslander et al showed that symptoms are less predictive of the actual type of incontinence as patients get older.13 Therefore, the older the patient the less predictive symptoms are of the actual cause of incontinence.
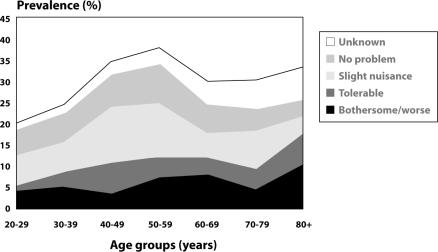
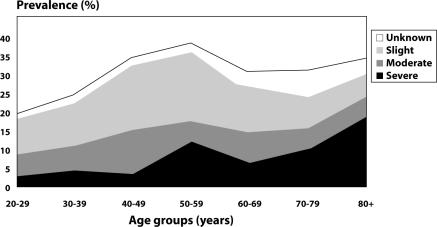
When severity and bother are included in the assessment of the prevalence of incontinence, the picture dramatically changes. Sandvik et al reported that when only moderate and severe bother are considered, the variability in prevalence ranges from approximately 3% to 17%, with most studies reporting 4% to 8% (Figure 2).12 Sandvik et al also looked specifically at the threshold of severity from slight to moderate to severe.14 They showed that severe incontinence comprises only a small portion of the population in the younger years, peaks at menopause, and then steadily and rapidly increases in the elderly population (through the 70’s and 80’s) (Figure 3). Finally, when moderate to severe incontinence is combined with the impact of considerable bother, this defines a segment of patients in the general population that are most likely going to require medical attention.15
Figure 2.
Prevalence of urinary incontinence when different thresholds of bother are considered. Data from Sandvik et al.12 Reprinted from Dionko et al,16 with permission
Figure 3.
Prevalence of urinary incontinence when different thresholds of severity are considered. Data from Sandvik et al.14 Reprinted from Dionko et al,16 with permission.
From a medical economic perspective, it is critical to realize that studies in the general population that are based on questionnaires will often include patients with degrees of incontinence that are not significant enough to cause bother or to have patients seek treatments. This means that epidemiological data that attempts to determine the prevalence of incontinence in the general population, as opposed to those who have sought or are seeking treatment, may be irrelevant with regard to allocating healthcare resources. Of significance in this regard is the data by Dionko et al, who showed that only 40% of incontinent patients would actually bring the issue of incontinence to the attention of their physicians.16 It is not clear, however, whether this is 40% of patients who are bothered or merely 40% of elderly individuals.
Incontinence in Men
The prevalence of incontinence in men of all ages is certainly lower than that for women. Large studies have indicated that there is a 3% to 11% overall prevalence rate of incontinence in the male population with urge incontinence being the prominent symptom reported in 40% to 80% of patients.14 Next, mixed incontinence is the most prevalent at 10% to 30%, whereas isolated stress incontinence accounts for less than 10% of incontinence in male patients. Stress incontinence in men is rare unless the patient has undergone some type of prostate surgery or has suffered neurological injury or trauma. Incontinence in men increases with age and appears to rise more steadily than it does in women. That is, there are no spikes in prevalence similar to those that occur for women around menopause. However, the estimates for severe incontinence in men in their 70’s and 80’s is still only about half of that in women.14 A major consideration in the incontinent male patient, especially with urge incontinence, is the potential contribution of bladder outlet obstruction to bladder overactivity. Many men suffering from bladder overactivity will also have bladder outlet obstruction. Such a situation can affect therapeutic options for patients.
Conclusions
There is certainly a large variability in reported prevalence rates for incontinence in men and women depending on study designs, definitions, and other factors that have been discussed. There is little data on incidence and not a great deal about the natural history of incontinence, at least in good epidemiologic studies. Data on remission rates of incontinence are also limited. Because of this lack of information, it is difficult to provide concise answers when patients present with incontinence and asks for a prognosis, that is, whether they will get better or worse without treatment. To provide better care for incontinent patients, it is critical that we target the correct populations to be treated. In defining those targets, it must be decided whether to collect data on all incontinent patients or only those seeking treatment. It is also important to determine the threshold for severity and bother that should be included in decision-making pertaining to allocation of resources for research and development and for treatment.
Main Points.
When discussing the epidemiology and impact of incontinence, it is important to distinguish between prevalence and incidence.
Prevalence is the probability of having incontinence within a defined population at a defined point in time; incidence is the probability of developing incontinence during a defined period of time.
In most discussions on incontinence, especially when determining social impact and allocation of healthcare resources, prevalence is the more important parameter.
Incontinence may be a result of bladder dysfunction, sphincter dysfunction, or a combination of both.
In women, the prevalence is relatively low early in life, has a peak around the time of menopause, and then rises steadily between the ages of 60 to 80 years.
The prevalence of incontinence in men of all ages is lower than that for women, with urge incontinence being the prominent symptom.
It is important to target the correct population of patients—those with the most severe, bothersome incontinence—to make the proper allocations of heath resources for research and treatment.
References
- 1.Sandvik H. Bergen, Norway: Department of Public Health and Primary Health Care, University of Bergen; 1995. Female urinary incontinence: studies of epidemiology and management in general practice [thesis] [Google Scholar]
- 2.Iosef CS, Bedassy Z. Prevalence of genitourinary symptoms in the late menopause. Acta Obstet Gynecol Scand. 1984;63:257–260. doi: 10.3109/00016348409155509. [DOI] [PubMed] [Google Scholar]
- 3.Hording U, Pedersen KH, Sidenius K, Hedegaard L. Urinary incontinence in 45-year-old women. An epidemiological survey. Scand J Urol Nephrol. 1986;20:183–186. doi: 10.3109/00365598609024491. [DOI] [PubMed] [Google Scholar]
- 4.Elving LB, Foldspang A, Lam GW, Mommsen S. Descriptive epidemiology of urinary incontinence in 3,100 women age 30–59. Scand J Urol Nephrol Suppl. 1989;125:37–43. [PubMed] [Google Scholar]
- 5.Sommer P, Bauer T, Nielsen KK, et al. Voiding patterns and prevalence of incontinence in women. A questionnaire survey. Br J Urol. 1990;66:12–5. doi: 10.1111/j.1464-410x.1990.tb14855.x. [DOI] [PubMed] [Google Scholar]
- 6.Harrison GL, Memel DS. Urinary incontinence in women: its prevalence and its management in a health promotion clinic. Br J Gen Pract. 1994;44:149–152. [PMC free article] [PubMed] [Google Scholar]
- 7.Yarnell JW, Voyle GJ, Richards CJ. Stephenson TP. The prevalence and severity of urinary incontinence in women. J Epidemiol Community Health. 1981 Mar;35:71–74. doi: 10.1136/jech.35.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diokno AC, Brock BM, Brown MB, Herzog R. Prevalence of urinary incontinence and other urological symptoms in the noninstitutionalized elderly. J Urol. 1986 Nov;136:1022–1025. [PubMed] [Google Scholar]
- 9.Holst K, Wilson PD. The prevalence of female urinary incontinence and reasons for not seeking treatment. N Z Med J. 1988;101:756–758. [PubMed] [Google Scholar]
- 10.Burgio KL, Matthews KA, Engel BT. Prevalence, incidence and correlates of urinary incontinence in healthy, middle-aged women. J Urol. 1991 Nov;146:1255–1259. doi: 10.1016/s0022-5347(17)38063-1. [DOI] [PubMed] [Google Scholar]
- 11.Lara C, Nacey J. Ethnic differences between Maori, Pacific Island and European New Zealand women in prevalence and attitudes to urinary incontinence. N Z Med J. 1994 Sep 28;107:374–376. [PubMed] [Google Scholar]
- 12.Sandvik H, Hunskaar S, Vanvik A, et al. Diagnostic classification of female urinary incontinence: an epidemiological survey corrected for validity. J Clin Epidemiol. 1995 Mar;48:339–343. doi: 10.1016/0895-4356(94)00147-i. [DOI] [PubMed] [Google Scholar]
- 13.Ouslander J, Staskin D, Raz S, et al. Clinical versus urodynamic diagnosis in an incontinent geriatric female population. J Urol. 1987;137:68. doi: 10.1016/s0022-5347(17)43873-0. [DOI] [PubMed] [Google Scholar]
- 14.Sandvik H, Hunskaar S, Seim A, et al. Validation of severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health. 1993;47:497. doi: 10.1136/jech.47.6.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunskaar S, Arnold EP, Burgio K, et al. Epidemiology and natural history of urinary incontinence. In: Abrams P, Khoury S, Wein A, et al., editors. Incontinence—First International Consultation on Incontinence. Plymouth, UK: Plymbridge Distributors Ltd.; 1999. pp. 199–226. [Google Scholar]
- 16.Dionko AC, Brock BM, Brown MB, et al. Prevalence of urinary incontinence and other urological symptoms in the noninstitutionalized elderly. J Urol. 1986;136:1022. [PubMed] [Google Scholar]