Abstract
Fibrous pseudotumor of the bladder, a rare, benign, and proliferative lesion of the submucosal stroma, can be mistaken on gross examination for a malignant lesion and must be differentiated on histologic examination from several bladder malignancies. Radiographic examination alone cannot establish a definitive diagnosis. Complete transurethral resection of such lesions appears to be curative.
Key words: Bladder diseases; Fibroma; Hematuria; Urothelium, abnormalities
Inflammatory pseudotumor of the bladder was first reported by Roth1 in 1980, when he described a 32-year-old woman with recurrent cystitis and hematuria associated with an ulcerated bladder lesion. Most reported cases cite gross hematuria as the presenting symptom. Endoscopically and radiographically, these solid mass lesions cannot be distinguished from malignant tumors of the bladder. Unique histologic features include tumor-like, atypical spindle cell proliferations. The histogenesis and etiology of fibrous pseudotumors have not been defined, although chronic cystitis is characteristic in the history.2
Accurate diagnosis of these lesions, before and after excision, presents a significant challenge. We present a case report as well as a literature review concerning the presentation, radiographic and histologic findings, and management of fibrous pseudotumor of the bladder.
Case Report
A 31-year-old woman presented with a 3-day history of recurrent, gross hematuria. She described having blood in the midstream portion of her urine and having passed several small blood clots through the urethra. She also complained of severe urinary frequency (every 30 minutes), polyuria, polydipsia, and low back discomfort. The patient denied any history of fever, chills, sweats, nausea, or vomiting but had lost 10 lb during the preceding 2 weeks. She had intermittent, severe dysuria and sharp, low abdominal pain with the completion of each micturition. Past incidences of hematuria and recurrent urinary tract infections led to a history of multiple emergency department visits. Her medical history is significant for amenorrhea (since 1993), normocytic anemia, and hypothyroidism. She has no prior history of urinary tract calculi, instrumentation, trauma, or other urologic problems. She has smoked 1 pack of cigarettes a day for approximately 15 years and is also a recovering alcohol and cocaine addict.
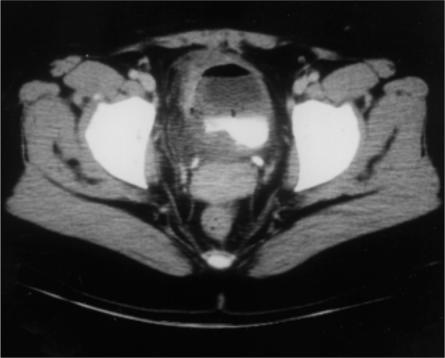
Physical examination revealed a mildly obese woman who appeared in good health. She was afebrile and hemodynamically stable. Bimanual pelvic examination identified a palpable, solid, large, mobile mass situated near the right wall of the bladder. Other pertinent findings included bilateral costovertebral angle tenderness, which was thought to be musculoskeletal in nature. Urinalysis documented hematuria without pyuria. Culture of a clean-catch urine specimen and cytologic examination of the voided urine were negative for abnormalities. Hematologic tests demonstrated a hemoglobin level of 8.9 g/dL and a hematocrit level of 25.4 mL/dL. CT of the abdomen and pelvis identified inflammatory, neoplastic changes within the bladder without evidence of pelvic adenopathy (Figure 1).
Figure 1.
CT scan of the pelvis with identification of an inflammatory neoplastic mass at the right lateral bladder wall.
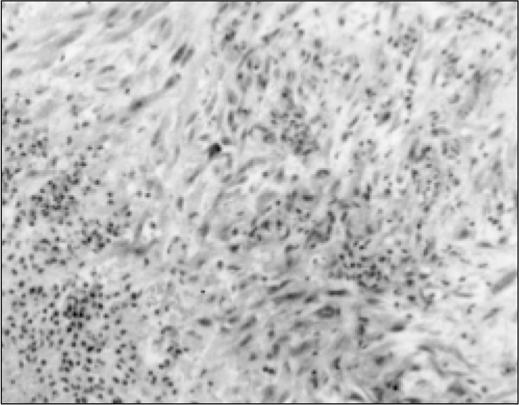
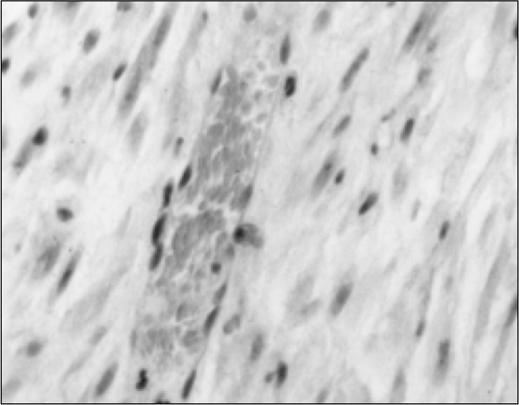
Cystoscopy revealed a large, pedunculated, whitish, solid tumor located at the right lateral bladder wall. There were marked inflammatory changes of the urothelium in the vicinity of the mass. Bilateral retrograde pyelograms showed normal upper tracts. Random cold-cup biopsies of the inflamed urothelium were obtained before complete transurethral resection of the mass was performed with a 28F resectoscope. The specimen consisted of pink-tan, rubbery tissue measuring 7 × 7 × 2.5 cm in aggregate and weighing 32 g. Transitional cell hyperplasia was evident on histologic examination of the bladder biopsy specimens. Microscopic examination of the bladder mucosal surface resected with the tumor identified ulceration (Figure 2A). The underlying tumor tissue consisted of bland spindle cells with elongated nuclei; spindle cells were arranged in fascicles. No obvious mitoses were observed (Figure 2B).
Figure 2A.
Photomicrograph of the bladder lesion showing ulceration of the mucosal surface and underlying spindle cell elements. Hematoxylin and eosin stain, reduced from ×40.
Figure 2B.
Spindle cell elements of the bladder lesion with benign nuclei. Hematoxylin and eosin stain, reduced from ×100.
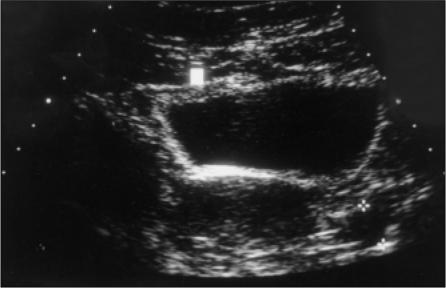
The final diagnosis was fibrous pseudotumor of the bladder, which was confirmed by the Armed Forces Institute of Pathology. The most recent urinalysis, pelvic ultrasonography (Figure 3), and cystoscopic follow-up evaluation 4 years after transurethral resection revealed no evidence of recurrent hematuria or tumor.
Figure 3.
Pelvic ultrasonogram demonstrating normal bladder at 4-year follow-up.
Discussion
Reactive, nonneoplastic proliferations arising within the bladder have been well documented and described in the literature. Terminology for such lesions has included atypical myofibroblastic tumor, atypical fibromyxoid tumor, pseudosarcomatous fibromyxoid tumor, plasma cell granuloma, nodular fascisms of the bladder, and inflammatory pseudotumor.3 While some authors may object to the term, inflammatory pseudotumor is most commonly used to describe this entity. Although lesions are thought to be benign, the importance of not misdiagnosing this process as a malignant one has been stressed repeatedly throughout the literature.
This lesion may occur at any age (range, 2 to 80 years), but typically occurs in young adults (average age, 28). Women appear to be twice as likely as men to present with this lesion. The size of the lesion is quite variable and has been reported as large as 9 cm, but most do not exceed 6 cm.4 Gross hematuria is the most common symptom at presentation. Gross examination typically reveals exophytic, singular, broad-based tumors that appear malignant endoscopeically. On microscopic examination, the characteristic appearance is that of spindle cells widely spaced in a vascular, myxoid, or edematous stroma. Some lesions demonstrate extensive sclerosis and infiltrating margins.4
Transurethral resection or partial cystectomy has been reported as the treatment of choice. To date, there has been only 1 reported case of recurrent disease following transurethral resection, but this was thought to be caused by incomplete removal of the transmural lesion.5 We proceeded with transurethral resection in our study patient. The benign nature of the lesion after complete resection is demonstrated by the lack of recurrence or evidence of metastasis 4 years following definitive surgical management. Therefore, it seems that the optimal treatment is complete local excision, which can be achieved with minimal morbidity.
These lesions can be regarded as an abnormal reparative proliferation of fibroblastic or myofibroblastic spindle cells and granulation tissue. As such, they grow slowly, do not metastasize, and have not been described as undergoing malignant transformation.6 Management should include surveillance endoscopy and biopsy to document resolution.7
In conclusion, we feel that the clinical manifestations and radiographic appearance of fibrous pseudotumor of the bladder are nonspecific. The combined clinical, gross, and microscopic pathologic features must be completely and carefully evaluated to differentiate this lesion from a malignant process. Pathologic examination remains the gold standard in achieving a definitive diagnosis. Special studies, such as immunohistochemical and electron microscopic examination, may prove helpful in determining the nature of the lesion.8 These lesions respond well to conservative management, have distinctive morphologic and intrastructural findings, and demonstrate no metastatic potential. Patients have an excellent prognosis following complete local excision. Because fibrous pseudotumors of the bladder are histologically similar to certain malignant tumors, close follow-up is necessary when considering the overall management of patients with these pseudotumors.
References
- 1.Roth JA. Reactive pseudosarcomatous response in urinary bladder. Urology. 1980;16:635–637. doi: 10.1016/0090-4295(80)90578-6. [DOI] [PubMed] [Google Scholar]
- 2.Wanibuchi H, Iwata H, Washida H, et al. A case report of inflammatory pseudotumor of the urinary bladder. Osaka City Med J. 1995;41:31–39. [PubMed] [Google Scholar]
- 3.Jones EC, Clement PB, Young RH. Inflammatory pseudotumor of the urinary bladder: a clinicopathological, immunohistochemical, ultrastructural, and flow cytometric study of 13 cases. Am J Surg Pathol. 1993;17:264–274. doi: 10.1097/00000478-199303000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Young RH. Pseudoneoplastic lesions of the urinary bladder and urethra: a selective review with emphasis on recent information. Semin Diagn Pathol. 1997;14:133–146. [PubMed] [Google Scholar]
- 5.Gugliada K, Nardi PM, Borenstein MS, Torno RB. Inflammatory pseudosarcoma (pseudotumor) of the bladder. Radiology. 1991;179:66–68. doi: 10.1148/radiology.179.1.2006306. [DOI] [PubMed] [Google Scholar]
- 6.N’Dow J, Brown PAJ, McClinton S, et al. Inflammatory pseudotumor of the urinary bladder. Br J Urol. 1993;72:379–380. doi: 10.1111/j.1464-410x.1993.tb00738.x. [DOI] [PubMed] [Google Scholar]
- 7.Stark GL, Feddersen R, Lowe BA, et al. Inflammatory pseudotumor (pseudosarcoma) of the bladder. J Urol. 1989;141:610–612. doi: 10.1016/s0022-5347(17)40911-6. [DOI] [PubMed] [Google Scholar]
- 8.Jones EC, Young RH. Myxoid and sclerosing sarcomatoid transitional cell carcinoma of the urinary bladder: a clinicopathologic and immunohistochemical study of 25 cases. Mod Pathol. 1997;10:908–916. [PubMed] [Google Scholar]