Abstract
Numerous gender-specific etiologies are responsible for bladder outlet obstruction (BOO). BOO may be induced by specific functional and anatomic causes. The resulting obstruction frequently produces lower urinary tract symptoms (LUTS). Categorizing and understanding these entities is crucial when proceeding with a LUTS evaluation as specific diagnostic modalities may then be used to fully delineate the degree of BOO and any secondary issues. Although urodynamic evaluation and pressure flow evaluation is the gold standard diagnostic tool, other modalities may also be used, including post void residual analysis, urinary flow rates, cystoscopy, and selected radiologic ones. Patient self-appraisal of symptoms using various inventories such as the American Urologic Association Symptom Index or the International Prostate Symptom Score is relevant to the initial assessment and subsequent longitudinal follow up. Analysis of secondary symptoms of obstruction in women is often performed using a subjective symptom appraisal and is determined urodynamically, assessing the pressure-flow relation during voiding. The complete assessment of LUTS arising from BOO often includes several of these modalities to fully define the obstructive impact on the individual's urinary function and quality of life.
Key words: Bladder outlet obstruction, Lower urinary obstruction, Lower urinary tract symptoms, Benign prostatic obstruction, Gender differences, Urodynamic studies, Cystoscopy, Quality of life issues, Noninvasive measures
When considering the causes of bladder outlet obstruction (BOO), it is important to appreciate that BOO results from a variety of etiologies, which may be functional or anatomic. BOO often produces lower urinary tract symptoms (LUTS), although the degree of bother by LUTS is highly variable and not predictable on the basis of the specific inciting etiology. Induced LUTS symptoms may be predominantly obstructive, irritative, or often a combination of both. Typically, obstructive symptoms include hesitancy, sensation of incomplete bladder emptying, diminished urinary stream, and post voiding urinary dribbling. Irritative complaints include urinary urgency, frequency of urination, occasional dysuria, and nocturia. Rarely are symptoms related to BOO isolated; often the individual experiencing LUTS presents with a variety of mixed symptoms of obstruction and irritation. BOO may also occur in the complete absence of symptoms and be first identified in the scenario of urinary retention or decompensation of the upper urinary tracts.
Functional obstruction may be caused by detrusor-sphincter dyssynergia (DSD), either at the level of the smooth muscle or rhabdosphincter; primary bladder neck obstruction, which may be functional and anatomic in character; or due to dysfunctional voiding, associated with learned voiding disorders or pelvic floor dysfunction associated with pain syndromes. Anatomic obstruction in men results most commonly from benign prostatic enlargement (BPH) or urethral stricture. In women, anatomic obstruction most commonly arises from incontinence procedures.
Whatever the etiology, BOO produces compression or resistance upon the bladder outflow channel at any location from the bladder neck to urethral meatus. This induced resistance initiates a bladder response that is highly variable and quite unpredictable. The characteristic symptomatic response—with some combination of obstructive and irritative complaints—is nonspecific for causation and intensity. Therefore, disabling irritative symptoms can exist with minimal objective findings, whereas complete decompensation of the lower urinary tract may be identified in an otherwise asymptomatic individual.
Given the substantive symptomatic impact of BOO regardless of gender, symptomatic appraisal is a crucial aspect of evaluation. When used in association with screening history, physical examination, and postvoid residual urine volume (PVR) determination, symptomatic response may be used as a monitor for LUTS progression and response to therapy. This proposed evaluation paradigm presupposes that confounding factors are not present or identified on initial screening (eg, significant PVR, neurologic disease, prior lower urinary tract surgical intervention, etc). Under the circumstance of identified comorbidity, lack of response to initial empiric therapy, progression of symptoms despite therapy, or in the case of doubt regarding etiology, more advanced urodynamic evaluation is indicated.
The evaluation goal is not only to establish a likely diagnosis, but to define bladder storage and emptying characteristics. Bladder storage abnormality is often an underappreciated sequela of BOO, and is associated with substantive symptomatic and physiologic effect. Urodynamic evaluation is the gold standard for quantitating the degree of obstruction, related detrusor contractile dysfunction, and simultaneous pressure/flow analysis. The evaluation of detrusor contraction magnitude with contemporaneous analysis of flow, often with fluoroscopic observation, provides the most definitive assessment of the voiding event.
Urodynamic assessment of voiding, however, is not without confounding variables (eg, urethral catheter size, ability of the individual to void in the circumstances of the study, academic disagreement surrounding absolute and cutoff criteria for obstruction). Nonetheless, urodynamic studies (UDS) supply critical data for management and treatment planning, and represent an integral component of assessing complicated BOO.
Bladder Outlet Obstruction In Women
Causation
The etiologies for BOO in women are diverse and represent a combination of functional and anatomic issues. The most common causative factor is considered to be obstruction from stress urinary incontinence (SUI) surgery (Table 1). The overall adjusted incidence of BOO arising from incontinence interventions is estimated to be approximately 2%.1 However, this approximation is assumed for urinary retention after surgery. Given that BOO may present with less dramatic but bothersome symptoms (eg, positional voiding dysfunction, hesitancy, interrupted urinary flow, and de novo or exacerbated urinary urgency and frequency), the overall incidence of postoperative obstruction is probably much higher and more properly reflected by the ranges reported by the American Urologic Association (AUA) Guidelines on SUI.2
Table 1.
Etiologies of Bladder Outlet Obstruction in Women
Non-neurogenic
|
Neurogenic
|
Furthermore, obstructive symptoms may be obfuscated by either persistent SUI or urinary tract infection. More recent meta-analysis has similarly reported that varying rates of voiding dysfunction, mainly obstruction, after incontinence surgery are somewhat dependent on the type of procedure performed. These procedures are retropubic (Burch), 4% to 22%; retro-pubic (Marshall-Marchetti-Krantz), 5% to 20%; pubovaginal sling, 4% to 10%; transvaginal needle suspension, 5% to 7%; and tension-free vaginal tape, 2% to 4%. Autologous slings, as the gold standard intervention, have associated rates of obstruction as defined by the author of 1% to 33%, although the definition of “obstruction” is extremely varied across series.2
A consequence of postoperative obstructive phenomenon is secondary intervention to relieve sling tension or to explant the sling due to associated obstructive phenomena. The rates of lysis for autologous slings range from 1% to 30% with additional patients who require long-term catheterization (2 to 42%) and urethral dilation (3 to 8%).1 New onset storage symptoms range from 0 to 43%. Similar cumulative rates of obstruction, retention, and storage abnormality have been reported with allograft slings. Although ostensibly less morbid, even newer midurethral technologies for sling application appear to have persistent rates of retention and new urinary symptoms that reflect the altered dynamic of urethral support associated with these techniques. No standardized method for reporting voiding difficulties after surgical intervention for SUI yet exists; however, a proposed system might include some combination of symptomatic and objective assessment.
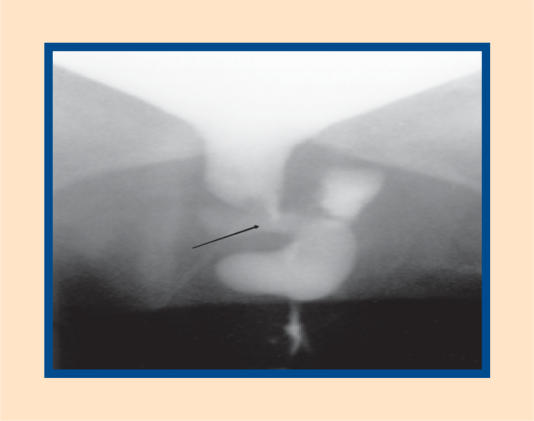
Noniatrogenic anatomic causes of obstruction include pelvic organ prolapse (cystocele, rectocele, enterocele, uterine procidentia), genital malignancy (such as uterine or cervical carcinoma), extra-urinary vaginal masses (vaginal cysts, Gartner's duct remnants), and urethral pathology (diverticulum, urethral carcinoma) (Figure 1). Gynecologic lesions also may produce BOO inclusive of large ovarian cysts or tumors,3,4 and cervical or uterine tumors. BOO may also occur during pregnancy due to uterine displacement.5–7 Usually, retention in pregnancy resolves within the first trimester due to uterine enlargement and anteversion.5–7
Figure 1.
Complex urethral diverticulum causing urethral obstruction. Arrow denotes relative area of urethral stenosis.
Pelvic prolapse is increasingly being identified as contributing to voiding dysfunction in many women. Gardy and colleagues8 reported a rough correlation between grade of cystocele and residual urine volume in a group of women with prolapse, with higher grades (3 and 4) having a 30% higher association with elevated PVR. High grade prolapse may also lead to renal deterioration due to obstruction of the bladder outlet, ureteral orifices, or both.9 Even prolapse lesions arising in other compartments such as large rectoceles can produce anatomic obstruction at the bladder outlet.10
Functional obstruction can arise from sphincteric dyssynergia, smooth or skeletal, arising from neurogenic causes; smooth muscle dyssynergia without neurogenic cause (primary bladder neck obstruction); and sphincteric pseudo-dyssynergia secondary to dysfunctional voiding (Hinman's syndrome).
Dysfunctional voiding can produce profound effects on the urinary tract with both symptomatic and anatomic sequelae.11–14 Although previously considered a pediatric diagnosis, it is increasingly being recognized in adults who present with mixed irritative and obstructive complaints.15–17 Dyssynergy manifested by these patients has been explained as a compensatory response of the urethral sphincteric mechanism to sudden detrusor overactivity. With chronicity, this response becomes ingrained into the voiding habit resulting in incomplete emptying and staccato or poor urinary flow.15–17 External sphincter spasticity has been reported to arise from inflammatory conditions of the pelvic floor such as urethritis, cystitis, or periurethral glandular infection.18,19
Neurogenic dyssynergia is commonly seen with multiple sclerosis (MS) and other suprasacral neurologic lesions in women. Although several forms of dyssynergia may exist,20 what commonly arises is an obstructive pattern most often seen with MS. Sirls and colleagues21 reported that 28 of 113 women with MS demonstrated DSD, with 70% also manifesting detrusor overactivity. These urodynamic findings have been correlated with plaque progression and atrophy in patients with progressive MS.22
The distinct entity of primary bladder neck obstruction in women is assumed to be rare. Groutz and colleagues noted that it accounted for 8% of 38 women in their series.23 Kuo diagnosed this entity in 30 of 76 women with BOO on the basis of pressure/flow criteria.24 Others have reported incidences ranging from 0 to 4% in large well-characterized groups of women with voiding dysfunction.25,26 Although unknown, putative etiologies for this clinical entity include smooth muscle hyper-trophy due to collagen deposition,27 increased smooth tonus imparting loss of elasticity to the proximal bladder neck,28 or increased or aberrant adrenergic receptor density in the smooth muscle of the proximal urethra.29–31
Primary urethral stricture disease is rare in women, usually being identified in those with prior urethral instrumentation or surgery, such as diverticular resection. In one series, however, primary urethral stricture disease accounted for 13% of women with BOO.23
Evaluation
Evaluation of the female patient with BOO requires a relatively high level of suspicion by the examining physician. Often significant symptoms lead to an initial consultation; as in men, the time course of symptom evolution may be variable. Inciting events, such as recent SUI surgery or development of an acute or subchronic anatomic lesion (eg, an infected diverticulum or vaginal prolapse), may assist in recognizing the etiology.
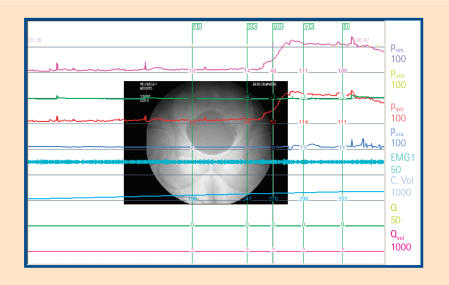
A variety of modalities may assist in the BOO diagnosis. Nonurodynamic testing modalities are usually used in combination with some urodynamic evaluation to give a complete delineation of the inciting etiology and the overall impact of lower urinary tract function (Figure 2).
Figure 2.
Urodynamic tracing, including pressure-flow analysis, of woman with BOO after pubovaginal sling surgery. Note voiding pressures greater than 100 cm H2O. BOO, bladder outlet obstruction.
Medical history and physical examination provide the basic foundation for subsequent evaluation. Certain factors such as medication use, changes in mobility, and alterations in bowel function must be considered. The time course of symptom development and the possible relationship with inciting events (eg, SUI surgery or an acute neurogenic event, such as exacerbation or development of overt MS) also must be factored into the decision and diagnostic paradigm.
Similarly, certain physical examination factors must also be evaluated. These include the presence and degree of concomitant vaginal prolapse, inclusive of anterior, posterior, and apical compartments of the vagina; the presence and degree of urethral hypermobility; the degree of anterior vaginal wall fibrosis if BOO is present after surgery; and any associated neurologic abnormalities, such as loss or change of perineal sensation, anal sphincteric tone, bulbocavernosus reflex, or other lower extremity neurologic findings.
Nonurodynamic assessment modalities include PVR assessment, cystoscopy, radiographic techniques such as the voiding cystourethrogram (VCUG), and occasionally advanced assessments, such as MRI of the bladder outlet and urethra.
Urinary residual assessment is considered a vital factor in the over-all estimation of the degree of BOO. Previously, this assessment was performed by urethral catheterization. The recent development of accurate and reproducible ultrasonographic techniques that use portable devices and are comparable to stationary ultrasound results has allowed for the general use of these methods in the outpatient setting. Huang and colleagues found that although the percentage differences varied between techniques (eg, mean percentage error 13.1% with stationary and 36% with portable, mean volume differences 21.9 mL vs 34.4 mL respectively), the accessibility and ease of the portable method made it a very convenient approach for PVR assessment.32
Furthermore, ultrasound use in determining PVR has been an excel-lent predictor of catheterization in at-risk populations, such as post-partum women. Yip and colleagues noted significant correlation values between PVR estimated by ultrasound and by catheterized volumes in a group of postpartum women.33 Therefore, evidence supporting the reproducibility of ultrasound as an assessment of PVR suggests that this technique is not only an accurate but a facile and less invasive method than urethral instrumentation.
Cystoscopy provides visual assessment of the urethra and bladder, especially any alteration in the relationship between these structures, such as acute proximal urethral angulation or changes in urethral distensibility associated with fixation and peri-urethral fibrosis. Foreign bodies within the urinary tract also are best identified by this technique. Urethral abnormalities such as diverticuli or peri-urethral masses impinging on the urethral lumen may also be identified.
I find cystoscopy particularly important in the postoperative state, not only as a discriminating tool for locating obstruction foci, but as an outcome indicator of interventions for surgically induced BOO. Urethrolysis should correct any urethral deformation suspected of inducing the obstructive phenomenon and this resolution is confirmed intraoperatively with repeat cystoscopy before surgery is viewed as anatomically successful.
Advanced techniques such as VCUG may be used in conjunction with multichannel urodynamics when videourodynamic studies are not available. The VCUG may identify specific anatomic areas of obstruction, any radiographic evidence of prolapse, abnormal relationships between bladder lumen and urethral axis (consistent with hyperangulation), and urethral pathology, such as diverticulum resulting in obstruction or deformation of the urethra.
MRI evaluation of the female urethra has now become the gold standard for identification and assessment of both extrinsic and intrinsic urethral pathology. Endoluminal34 and external coil techniques have been used to assess urethral diverticular location and complexity with a high degree of specificity.35,36 MRI also has been found to provide delineation of extrinsic lesions such as mullerian duct remnants37 and leiomyoma.38 The unparalleled anatomic depiction that MRI provides established this technique as the radiologic test of choice when diagnostic possibilities include peri- or paraurethral lesions as possible etiologies for BOO in women.
Given the unique male and female differences in voiding, many of the prior micturition analyses standardized for men do not apply to women. The nomograms for obstruction in men applicable in the circumstance of prostatic obstruction pre- and post-treatment, for instance, do not apply to women. Due to the varying etiologies for BOO and the lack of standardized “normal” voiding parameters in women, no urodynamic definition of obstruction in women has been generally accepted.
Initial attempts to assess urodynamic obstruction in women used only noninvasive flow parameters with 15cc/s maximal flow chosen as the separation point.39 Others added the configuration of the flow pattern and the absence of significant PVR as an additional variable to this arbitrary flow magnitude.25 More complicated definitions have used multiple factors including detrusor pressure (> 50 cm H2O), maximum flow rate (< 12 mL/s), urethral resistance, and elevated in combination as indicating BOO.26 Further attempts at refining the urodynamic diagnosis have used simultaneous pressure/flow analysis to determine the optimum segregation values for peak flow (Qmax) and peak detrusor pressure at peak flow (Pdet @ Qmax).40
In a prospective evaluation of symptomatic women, the differentiating values for these variables were Qmax of 15 mL/s or less and a Pdet @ Qmax of greater than 20 cm H2O. Subsequent evaluation of a larger group noted that a Qmax ≤ 11 mL/s and a Pdet @ Qmax ≥ 21 cm H2O provided greater sensitivity and specificity.41 Further refinement and more patients have used Qmax ≥ 12 and Pdet @ Qmax ≥ 25 as the most discriminating values, with each variable, if not normal, indicative of BOO.42
In addition, the simultaneous use of fluoroscopy can add to the diagnosis of obstruction, allowing localization of the obstruction site.43 Nitti and colleagues also reported maximum flow (Qmax), detrusor pressure at maximum flow (Pdet @ Qmax), and magnitude of PVR as significant independent differentiating factors between obstruction and nonobstruction.
Other groups have reported similar segregating values. Blaivas and Groutz44 developed a nomogram for obstruction in women using some-what more strict segregating values.44 These were (Qmax ≤ 12 mL/s combined with a Pdet @ Qmax of > 20 cm H2O) and/or the presence of urinary retention, or inability to void despite sustained voiding pressures of > 20 cm H2O, or the presence of radiographically localized obstruction in the presence of sustained voiding pressures of > 20 cm H2O.
Given methodologic difficulties in obtaining the values defined above, the authors constructed their nomogram using noninstrumented flow and maximum voiding pressure as the variables. The resultant nomogram was then stratified by severity of obstruction, with moderate and severe obstruction being differentiated from no or mild obstruction at the relatively high peak voiding pressure of approximately 58 cm H2O.44 Although there has been reported agreement between these varied methods for determining obstruction,45 no absolute criteria as yet exist to fully differentiate obstruction in women, especially in cases when obstruction is superimposed on either low-pressure, premorbid voiding habits or in borderline cases.
Even in the case of suspected post-operative obstruction, absolute diagnosis is often evasive, and must be based on a composite assessment of subjective and objective criteria.
Bladder Outlet Obstruction in Men
Causation
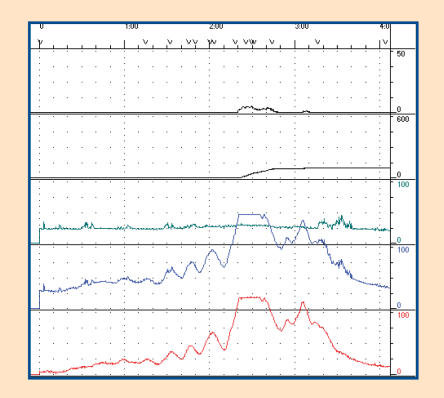
BOO in men has traditionally been linked to the prostate. Recent terminological changes have led to the use of benign prostatic obstruction/enlargement (BPO/BPE) as nomenclature to replace previously used eponyms such as benign prostatic hyperplasia (BPH). Also synonymous with BOO in men is LUTS.46 It is clear that LUTS, in both sexes, is at least partially due to a component of age-related detrusor dysfunction with the subsequent superimposition of other pathologies, most common of which in men is BPO (Figure 3). The appreciation that prostatic glandular and stromal hyper-plasia is not synonymous with BOO or LUTS has allowed a more advanced understanding of the dynamic factors involved in BOO in men.
Figure 3.
Detrusor storage abnormality associated with high pressure obstruction in male with BOO due to prostatic enlargement. BOO, bladder outlet obstruction.
By far, BPO is the most common cause of BOO in men and stems from a variety of etiologies. Glandular and stromal hyperplasia of the prostate has long been supposed to be a primary contributor to BPO. However, complex aging-related factors probably also play a role in maturation and subsequent senescence of hyperplastic tissue within the prostate. Recently the documentation of senescent prostatic epithelial cells in men with enlarged prostates suggests that these cells may play a role in BPO development.47
Although androgens do not fundamentally produce BPH, the presence of androgens is required for subsequent development of BPH and this is a permissive effect. With age, despite the diminishing levels of circulating testosterone, levels of dihydrotestosterone (DHT) and androgen receptor remain high, therefore implicating the potential role of these 2 components of the androgen cascade in the perpetuation of prostatic enlargement.48 The enzyme 5α-reductase is critical for conversion of testosterone into DHT, which remains the principal androgen within the prostate throughout life.49
Withdrawal of the high local concentration of androgens results in cellular apoptosis and is considered one of the crucial components of involution of hyperplastic cells.50 At least two 5α-reductase enzymes are known to exist (Type 1 and Type 2). The Type 2 enzyme is considered to be the critical component for hyper-plastic growth in middle and later age.51 The type 2 subtype of 5α-reductase has a predominant effect in the prostatic stroma.
Increasing evidence also suggests that stromal and epithelial interactions in the prostate produce both the normal prostatic environment as well as the aberrant one necessary for the development of hyperplastic prostatic tissue. Some data suggest that BPH arises due to a defect in the stromal control component within the unique stromal-epithelial interaction.52
Another important factor in the development of hyperplastic tissue within the prostate may be inter-action between local growth factors and steroid hormones. These growth factors include a diverse stimulatory group such as insulin-like growth factor (IGF), transforming growth factor-beta (TGF-β) and other epithelial type growth factors.53
Finally, familial and genetic contributions also must be factored into the development of the hyper-plastic prostate. Analysis of inheritance patterns of men undergoing treatment for BOO due to prostatic disease suggests an autosomal dominant inheritance pattern with a higher concordance rate in monozygotic twins as compared to identical embryos.54 Also, prostatic hyperplasia associated with familial inheritance patterns usually is characterized by larger glandular size compared to men with sporadic BPH.
Other prevailing causes of BOO in men include urethral stricture disease. This is a much more common entity in men than in women and often is not perceived as an anatomic finding until a patient presents with urinary retention or other symptoms initially thought to be due to non-specific LUTS. Previously considered to be primarily due to inflammatory disorders such as urethritis, urethral stricture disease is now considered to be most commonly due to trauma.
The interrelationship between detrusor and sphincteric function is also as important for BOO in men as in women. Dysfunctional voiding is being increasingly recognized as a component of chronic pain in LUTS syndromes, such as chronic prostatitis. Also, neurogenic-based DSD is commonly seen in various spinal cord and suprasacral neurologic processes. True dyssynergia is limited to spinal lesions that are suprasacral but infra-pontine in location. Pseudo-dyssynergia has been attributed to bradykinesia of the sphincter in Parkinson's disease and may also be present in other movement disorders, such as multiple systems atrophy.
Primary bladder neck obstruction in men is a much more common entity than in women, with incidence more substantially weighted towards younger men. (See Figure 4.) The contribution of smooth muscle tone as a basic etiology for primary bladder neck obstruction in men has been well documented.
Figure 4.
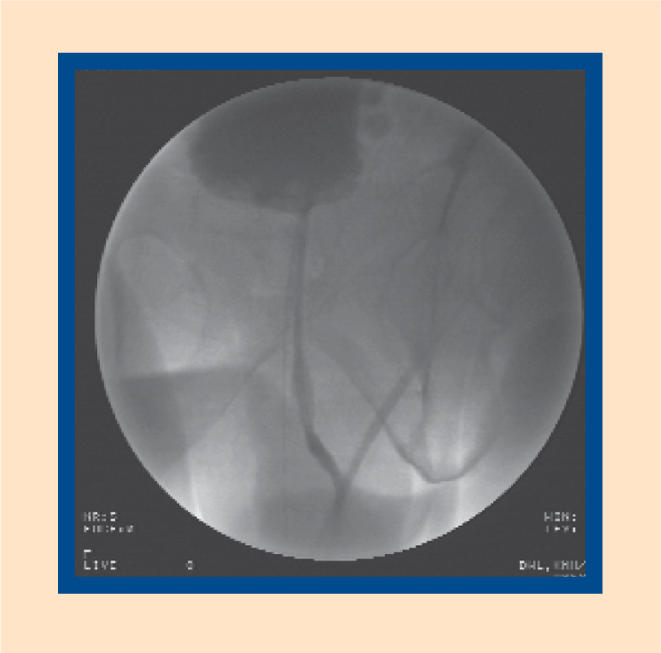
Fluoroscopic image of non-relaxing bladder neck in young male with presumptive primary bladder neck obstruction.
Evaluation
The evaluation of BOO in men is dependent on similar fundamental principles as that of women. Examination of historical and physical evidence of both onset and magnitude and severity of symptoms is critical in the primary evaluation of these patients.
Basic evaluation of LUTS and BOO in men includes ultrasonographic PVR; symptomatic assessment using validated tools, such as the AUA Urinary Symptom Index (AUA-7) or the International Prostate System Score (IPSS); and urinary flow rate determination. Neither uroflowmetry nor PVR is specific to BOO causation.55–59 Urinary flow rate is standardized and well accepted as a criterion for assessment of flow patterns. Flow rate parameters are well established (less than 10 mm/s consistent with obstruction).58–59
However, approximately one third of men with decreased flow rates are not obstructed and their diminished flow rates are representative of poor detrusor contractility. A normal flow rate also does not preclude the possibility of obstruction. Similarly, only about 50% of men with LUTS and increased PVR will be obstructed and one fourth of men with severe obstruction will not demonstrate any significant PVR elevation.60–61 There-fore, concomitant analysis of flow rates and residual volumes is important to avoid misinterpretation of isolated data. The combination of both tools, when viewed in light of bothering symptoms, is considered to be the best initial paradigm for establishing the BOO diagnosis.62–64
Noninvasive measures of the relationship between bladder pressure and flow rate have been described using 2 techniques. Both techniques use pressure transmission through a standing column of fluid, associated with an isovolumetric detrusor pressure, with occlusion of the urethral meatus during free urinary flow.65 One technique uses a condom catheter and occlusion technique with pressure transduction occurring distal to the urethral meatus.66 The other method uses a cuff that is inflated to compress the urethra. The pressure associated with interruption of urinary flow is equated to the isovolumetric detrusor pressure.67
Both techniques have some pitfalls and require further validation. The possible addition of this technique to other less invasive measures may provide an ideal minimally invasive paradigm for the assessment of BOO in the future.
In the case of failed presumptive therapy, complex presentation scenarios, ambiguous screening evaluation criteria, or when diagnosis is in doubt, more directed evaluation may be indicated. This would include urodynamics, alternative radiologic procedures, or cystoscopy. Cystoscopy is generally considered to be the most specific method with which to evaluate degree and magnitude of stricture presence within the urethra. Perineal ultrasonography has been used for this indication as well, although with less degree of familiarity in the hands of most urologists.
The one advantage of perineal ultrasonography may be its ability to determine the extent of mural fibrosis associated with the actual luminal stricture disease. Ultrasonography may also serve a role in patients suspected of having upper tract changes related to BOO, and may provide evidence for the effect of BOO on upper tract strictures. Urodynamic techniques include complete uroflowmetry, multi-channel urodynamics for complex cases, and video urodynamics in specialized situations.
Formal urodynamic evaluation is usually reserved for complicated cases or in situations where there has been no response to therapy that is seemingly appropriate on the basis of prior initial uroflow and PVR assessment. In men, urodynamics is often performed in conjunction with a simultaneous pressure flow evaluation. Although the sine qua non of obstruction in pressure/flow evaluation is high detrusor pressure associated with low urinary flow rate, other combinations may indicate the possibility of detrusor failure, such as low detrusor pressure with low urinary flow. Also, relatively increased urinary flow rates may be associated with high pressures, indicating an obstruction variant.
The pressure flow evaluation of complex BOO in men has been reasonably well standardized beginning with the International Continence Society nomogram for BPO first described in 1997.68 Other nomograms, such as the Abrams-Griffiths nomogram and the Schafer nomogram are relatively concordant.69 Using these nomograms, various subsidiary calculations have been proposed for obstruction. The Bladder Outlet Obstruction Index (BOOI) [where BOOI = Pdet @Qmax − 2(Qmax)] and Bladder Contractility Index (BCI) [where BCI = Pdet Qmax + 5(Qmax)] have both been proposed as bladder function assessments associated with BOO.64,68 Both calculations simplify computations and allow the categorization of men with BOO and LUTS into subsidiary groups depending upon bladder contractility and outlet obstruction.68
Conclusions
The etiology of BOO is diverse and definitely gender specific. Often anatomic causes induce functional abnormality that remains somewhat unique for each individual, regardless of sex. A full appreciation of the possible etiologies of obstruction is necessary in order to identify overt and more subtle scenarios. In women, iatrogenic causes of obstruction are the most common. Other entities account for far fewer of the cases. The obstruction evaluation in women is somewhat more diverse in terms of modalities used, with no single grouping of techniques that are generally apropos. Individualized evaluation remains a tenet of analysis, and urodynamic criteria used to diagnose BOO in women continue to evolve.
In men, by far the most common entity producing BOO is BPO/BPE. Again, symptomatic appraisal is a crucial component of evaluation in order to assess the magnitude of symptom impact. The combination of PVR, urinary flow measures, and symptom appraisal has been generally accepted as the initial screening and evaluation paradigm for BOO and LUTS in men and are now considered standard. More complex techniques such as voiding pressure flow studies remain the gold standard and are more thoroughly standardized in men than in women.
Future trends will continue to focus on enhancing diagnostic accuracy and specificity of BOO evaluation. Noninvasive measures may become more commonly used as their validation against older techniques occurs.
Main Points.
Bladder outlet obstruction (BOO) results from functional or anatomic etiologies. BOO produces compression or resistance upon the bladder outflow channel at any location from the bladder neck to the urethral meatus. This produces lower urinary tract symptoms (LUTS), which may be predominantly obstructive, irritative, or often a combination of both.
The most common cause of BOO in women is obstruction from stress urinary incontinence (SUI) surgery. Recent meta-analysis has reported that varying rates of voiding dysfunction, mainly obstruction, after incontinence surgery are somewhat dependent on the type of procedure performed.
Nonurodynamic testing modalities are usually used in combination with urodynamic evaluation to diagnose BOO in women. Nonurodynamic assessment modalities include postvoid residual urine volume (PVR) assessment, cystoscopy, voiding cystourethrogram, and magnetic resonance imaging.
Due to the varying etiologies for BOO and the lack of standardized “normal" voiding parameters in women, no urodynamic definition of obstruction in women has been generally accepted.
In men, benign prostatic obstruction (BPO) is the most common cause of BOO and stems from a variety of etiologies. Other causes of BOO include urethral stricture disease, dysfunctional voiding, neurogenic-based detrusor-sphincter dyssynergia (DSD), and primary bladder neck obstruction.
A normal flow rate in men does not preclude the possibility of obstruction. Concomitant analysis of flow rates and residual volumes is important to avoid misinterpretation of isolated data.
Urodynamics, alternative radiologic procedures, or cystoscopy is recommended in the case of failed presumptive therapy, a complex presentation scenario, or when a diagnosis is in doubt.
Formal urodynamic evaluation is usually reserved for complicated cases and is often performed in conjunction with a pressure flow evaluation.
References
- 1.Gomelsky A, Scarpero HM, Dmochowski RR. Sling surgery for stress urinary incontinence in the female: what surgery, which material? AUA Update Series. 2003;XXII:266–276. (lesson 34) [Google Scholar]
- 2.Leach GE, Dmochowski RR, Appell RA, et al. J Urol. Vol. 158. The American Urological Association; 1997. Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical management of female stress urinary incontinence; pp. 875–880. (3 Pt 1) [DOI] [PubMed] [Google Scholar]
- 3.Kingsnorth AN. Urinary retention due to ovarian cyst. Br J Urol. 1984;56:439–440. doi: 10.1111/j.1464-410x.1984.tb05845.x. [DOI] [PubMed] [Google Scholar]
- 4.Doran J, Roberts M. Acute urinary retention in the female. Br J Urol. 1976;47:793–796. doi: 10.1111/j.1464-410x.1975.tb04059.x. [DOI] [PubMed] [Google Scholar]
- 5.Silva PD, Berberich W. Retroverted impacted gravid uterus with acute urinary retention: report of two cases and a review of the literature. Obstet Gynecol. 1986;68:121–123. [PubMed] [Google Scholar]
- 6.Hansen JH, Amussen M. Acute urinary retention in the first trimester of pregnancy. Acta Obstet Gynecol Scand. 1985;64:279–280. doi: 10.3109/00016348509155130. [DOI] [PubMed] [Google Scholar]
- 7.Burdon S, Maurer JE, Lich R., Jr Acute retention in pregnancy. J Urol. 1951;65:578–580. doi: 10.1016/S0022-5347(17)68523-9. [DOI] [PubMed] [Google Scholar]
- 8.Gardy M, Kozminski M, DeLancey J, et al. Stress incontinence and cystoceles. J Urol. 1991;145:1211–1213. doi: 10.1016/s0022-5347(17)38579-8. [DOI] [PubMed] [Google Scholar]
- 9.Nichols DH. Vaginal prolapse affecting bladder function. Urol Clin North Am. 1985;12:329–338. [PubMed] [Google Scholar]
- 10.Long CY, Hsu SC, Wu TP, et al. Urodynamic comparison of continent and incontinent women with severe uterovaginal prolapse. J Reprod Med. 2004;49:33–37. [PubMed] [Google Scholar]
- 11.Hinman F, Baumann FW. Vesical and ureteral damage from voiding dysfunction in boys without neurologic or obstructive disease. J Urol. 1973;109:727–732. doi: 10.1016/s0022-5347(17)60526-3. [DOI] [PubMed] [Google Scholar]
- 12.Allen TD. The non-neurogenic neurogenic bladder. J Urol. 1977;117:232–238. doi: 10.1016/s0022-5347(17)58412-8. [DOI] [PubMed] [Google Scholar]
- 13.Allen TD, Bright TC III. Urodynamic patterns in children with dysfunctional voiding problems. J Urol. 1978;119:247–249. doi: 10.1016/s0022-5347(17)57447-9. [DOI] [PubMed] [Google Scholar]
- 14.Hinman F., Jr Nonneurogenic neurogenic bladder (the Hinman syndrome) — 15 years later. J Urol. 1986;136:769–777. doi: 10.1016/s0022-5347(17)45077-4. [DOI] [PubMed] [Google Scholar]
- 15.Jorgensen TM, Djurhuus JC, Schroder HD. Idiopathic detrusor sphincter dyssynergia in neurologically normal patients with voiding abnormalities. Eur Urol. 1982;8:107–110. doi: 10.1159/000473490. [DOI] [PubMed] [Google Scholar]
- 16.McGuire EJ, Savastano JA. Urodynamic studies in enuresis and the nonneurogenic neurogenic bladder. J Urol. 1984;132:299–302. doi: 10.1016/s0022-5347(17)49603-0. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan WE, Firlit CR, Schoenberg HW. The female urethral syndrome: external sphincter spasticity as etiology. J Urol. 1980;124:48–49. doi: 10.1016/s0022-5347(17)55287-8. [DOI] [PubMed] [Google Scholar]
- 18.Raz S, Smith RB. External sphincter spasticity syndrome in female patients. J Urol. 1976;115:443–446. doi: 10.1016/s0022-5347(17)59235-6. [DOI] [PubMed] [Google Scholar]
- 19.Webster JR. Combined video/pressure/flow cystourethrography in female patients with voiding disturbances. Urology. 1975;5:209–215. doi: 10.1016/0090-4295(75)90012-6. [DOI] [PubMed] [Google Scholar]
- 20.McGuire E. Electromyographic evaluation of sphincter function and dysfunction. Urol Clin North Am. 1979;6:121–124. [PubMed] [Google Scholar]
- 21.Sirls LT, Zimmern PE, Leach GE. Role of limited evaluation and aggressive medical management in multiple sclerosis: a review of 113 patients. J Urol. 1994;151:946–950. doi: 10.1016/s0022-5347(17)35131-5. [DOI] [PubMed] [Google Scholar]
- 22.Ukkonen M, Elovaara I, Dastidar P, Tammela TL. Urodynamic findings in primary progressive multiple sclerosis are associated with increased volumes of plaques and atrophy in the central nervous system. Acta Neurol Scand. 2004;109:100–105. doi: 10.1034/j.1600-0404.2003.00184.x. [DOI] [PubMed] [Google Scholar]
- 23.Groutz A, Blaivas JG, Chaikin DC. Bladder outlet obstruction in women: definition and characteristics. Neurourol Urodyn. 2000;19:213–220. doi: 10.1002/(sici)1520-6777(2000)19:3<213::aid-nau2>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 24.Kuo HC. Urodynamic parameters for the diagnosis of bladder outlet obstruction in women. Urol Int. 2004;72:46–51. doi: 10.1159/000075272. [DOI] [PubMed] [Google Scholar]
- 25.Bass JS, Leach GE. Bladder outlet obstruction in women. Prob Urol. 1991;5:141–154. [Google Scholar]
- 26.Massey JA, Abrams PA. Obstructed voiding in the female. Br J Urol. 1988;61:36–39. doi: 10.1111/j.1464-410x.1988.tb09158.x. [DOI] [PubMed] [Google Scholar]
- 27.Farrar DJ, Osborn JL, Stephenson TP, et al. A urodynamic view of bladder outflow obstruction in the female: factors influencing the results of treatment. Br J Urol. 1976;47:815–822. doi: 10.1111/j.1464-410x.1975.tb04062.x. [DOI] [PubMed] [Google Scholar]
- 28.Axelrod SL, Blaivas JG. Bladder neck obstruction in women. J Urol. 1987;137:497–499. doi: 10.1016/s0022-5347(17)44086-9. [DOI] [PubMed] [Google Scholar]
- 29.Mayo ME. Primary bladder neck obstruction in men. J Urol. 1982;128:957–959. doi: 10.1016/s0022-5347(17)53299-1. [DOI] [PubMed] [Google Scholar]
- 30.Norgaard JP, Schwartz-Sorensen S, Djurhuus JC. Functional bladder neck obstruction in women. Urol Int. 1984;39:207–210. doi: 10.1159/000280977. [DOI] [PubMed] [Google Scholar]
- 31.Diokno AC, Hollander JB, Bennett CJ. Bladder neck obstruction in women: a real entity. J Urol. 1984;132:294–298. doi: 10.1016/s0022-5347(17)49601-7. [DOI] [PubMed] [Google Scholar]
- 32.Huang YH, Bih LI, Chen SL, et al. The accuracy of ultrasonic estimation of bladder volume: a comparison of portable and stationary equipment. Arch Phys Med Rehabil. 2004;85:138–141. doi: 10.1016/s0003-9993(03)00271-5. [DOI] [PubMed] [Google Scholar]
- 33.Yip SK, Sahota D, Chang AM. Determining the reliability of ultrasound measurements and the validity of the formulae for ultrasound estimation of postvoid residual bladder volume in postpartum women. Neurourol Urodyn. 2003;22:255–260. doi: 10.1002/nau.10112. [DOI] [PubMed] [Google Scholar]
- 34.Blander DS, Rovner ES, Schnall MD, et al. Endoluminal magnetic resonance imaging in the evaluation of urethral diverticula in women. Urology. 2001;57:660–665. doi: 10.1016/s0090-4295(00)01082-7. [DOI] [PubMed] [Google Scholar]
- 35.Rovner ES, Wein AJ. Diagnosis and reconstruction of the dorsal or circumferential urethral diverticulum. J Urol. 2003;170:82–86. doi: 10.1097/01.ju.0000067291.70172.b5. discussion 86. [DOI] [PubMed] [Google Scholar]
- 36.Vakili B, Wai C, Nihira M. Anterior urethral diverticulum in the female: diagnosis and surgical approach. Obstet Gynecol. 2003;102:1179–1183. doi: 10.1016/s0029-7844(03)00681-1. [DOI] [PubMed] [Google Scholar]
- 37.Okur H, Gough DC. Management of mullerian duct remnants. Urology. 2003;61:634–637. doi: 10.1016/s0090-4295(02)02418-4. discussion 637. [DOI] [PubMed] [Google Scholar]
- 38.Pavlica P, Bartolone A, Gaudiano C, Barozzi L. Female paraurethral leiomyoma: ultrasonographic and magnetic resonance imaging findings. Acta Radiol. 2004;45:796–798. doi: 10.1080/02841850410001376. [DOI] [PubMed] [Google Scholar]
- 39.Farrar DJ, Osborne JL, Stephenson TL, et al. A urodynamic view of bladder outflow obstruction in the female: factors influencing the results of treatment. Br J Urol. 1976;47:815–822. doi: 10.1111/j.1464-410x.1975.tb04062.x. [DOI] [PubMed] [Google Scholar]
- 40.Chassagne S, Bernier PA, Haab F, et al. Proposed cutoff values to define bladder outlet obstruction in women. Urology. 1998;51:408–411. doi: 10.1016/s0090-4295(97)00634-1. [DOI] [PubMed] [Google Scholar]
- 41.Lemack GE, Zimmern PE. Pressure flow analysis may aid in identifying women with outflow obstruction. J Urol. 2000;163:1823–1828. [PubMed] [Google Scholar]
- 42.Defreitas GA, Zimmern PE, Lemack GE, Shariat SF. Refining diagnosis of anatomic female bladder outlet obstruction: comparison of pressure-flow study parameters in clinically obstructed women with those of normal controls. Urology. 2004;64:675–679. doi: 10.1016/j.urology.2004.04.089. [DOI] [PubMed] [Google Scholar]
- 43.Nitti VW, Tu LM, Gitlin J. Diagnosing bladder outlet obstruction in women. J Urol. 1999;161:1535–1540. [PubMed] [Google Scholar]
- 44.Blaivas JG, Groutz A. Bladder outlet obstruction nomogram for women with lower urinary tract symptomatology. Neurourol Urodyn. 2000;9:553–564. doi: 10.1002/1520-6777(2000)19:5<553::aid-nau2>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 45.Fleischmann N, Hartanto V, Rosenblum N, et al. Comparison of diagnostic criteria for female bladder outlet obstruction. J Urol. 2004;171(suppl):450. doi: 10.1016/j.juro.2006.07.031. [DOI] [PubMed] [Google Scholar]
- 46.Abrams P. New words for old: lower urinary tract symptoms for “prostatism.”. BMJ. 1994;308:929–930. doi: 10.1136/bmj.308.6934.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choi J, Shendrik I, Peacocke M, et al. Expression of senescence-associated beta-galactosidase in enlarged prostates from men with benign prostatic hyperplasia. Urology. 2000;56:160–166. doi: 10.1016/s0090-4295(00)00538-0. [DOI] [PubMed] [Google Scholar]
- 48.McConnell JD, Barry MJ, Bruskewitz RC, et al. Clinical Practice Guideline. Number 8. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, U.S. Department of Health and Human Services; 1994. Benign prostatic hyperplasia: diagnosis and treatment. [PubMed] [Google Scholar]
- 49.McConnell JD. Prostatic growth: new insights into hormonal regulation. Br J Urol. 1995;76(suppl 1):5–10. [PubMed] [Google Scholar]
- 50.Kyprianou N, Isaccs JT. Expression of transforming growth factor-beta in the rat ventral prostate during castration-induced programmed cell death. Mol Endrocrinol. 1989;3:1515–1522. doi: 10.1210/mend-3-10-1515. [DOI] [PubMed] [Google Scholar]
- 51.Russell DW, Wilson JD. Steroid 5 alpha-reductase: two genes/two enzymes. Annu Rev Biochem. 1994;63:25–62. doi: 10.1146/annurev.bi.63.070194.000325. [DOI] [PubMed] [Google Scholar]
- 52.Isaac J, Coffey DS. Etiology and disease process of benign prostatic hyperplasia. Prostate. 1987;(suppl 2):33–50. doi: 10.1002/pros.2990150506. [AQ5] [DOI] [PubMed] [Google Scholar]
- 53.Peehl DM, Cohen P, Rosenfeld RG. The insulin-like growth factor system in the prostate. World J Urol. 1995;13:306–311. doi: 10.1007/BF00185974. [DOI] [PubMed] [Google Scholar]
- 54.Partin AW, Page WF, Lee BR, et al. Concordance rates for benign prostatic disease among twins suggest hereditary influence. Urology. 1994;44:646–650. doi: 10.1016/s0090-4295(94)80197-5. [DOI] [PubMed] [Google Scholar]
- 55.Yalla SV, Sullivan MP, Lecamwasam HS. Correlation of American Urological Association symptoms index with obstructive and nonobstructive prostatism. J Urol. 1995;153:674–679. [PubMed] [Google Scholar]
- 56.Sirls LT, Kirkemo AK, Jay J. Lack of correlation of the American Urological Association symptom 7 index with urodynamic bladder outlet obstruction. Neurourol Urodyn. 1996;15:447–457. doi: 10.1002/(SICI)1520-6777(1996)15:5<447::AID-NAU2>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 57.Van Ventrooij GEPM, Boon TA. The value of symptom score, quality of life score, maximal urinary flow rate, residual volume and prostate size for the diagnosis of obstructive benign prostatic hyperplasia: a urodynamic analysis. J Urol. 1996;155:2014–2018. doi: 10.1097/00005392-199606000-00057. [DOI] [PubMed] [Google Scholar]
- 58.George N, Slade N. Hesitance and poor stream in men without bladder outflow obstruction - the anxious bladder. Br J Urol. 1979;51:506–509. doi: 10.1111/j.1464-410x.1979.tb03589.x. [DOI] [PubMed] [Google Scholar]
- 59.Abrams PH, Griffiths D. The assessment of prostatic obstruction from urodynamic measurements and from residual urine. Br J Urol. 1979;51:129–134. doi: 10.1111/j.1464-410x.1979.tb02846.x. [DOI] [PubMed] [Google Scholar]
- 60.Gleason DM, Lattimer J. The pressure-flow study: a method for measuring bladder neck resistance. J Urol. 1962;87:844–852. doi: 10.1016/S0022-5347(17)65057-2. [DOI] [PubMed] [Google Scholar]
- 61.Griffiths DJ. The mechanics of the urethra and of micturition. Br J Urol. 1973;45:497–507. doi: 10.1111/j.1464-410x.1973.tb06812.x. [DOI] [PubMed] [Google Scholar]
- 62.McGuire EJ. The role of urodynamic investigation in the assessment of benign prostatic hyperplasia. J Urol. 1992;148:1133–1136. doi: 10.1016/s0022-5347(17)36841-6. [DOI] [PubMed] [Google Scholar]
- 63.McGuire EM, Woodside JR, Borden TA. Prognostic value of urodynamic testing in myelodysplasic children. J Urol. 1981;126:205–209. doi: 10.1016/s0022-5347(17)54449-3. [DOI] [PubMed] [Google Scholar]
- 64.Griffiths D, Hofner K, van Mastrigt R, et al. Standardisation of terminology in lower urinary tract function: pressure flow studies of voiding, urethral resistance and urethral obstruction. Neurourol Urodyn. 1997;6:1–18. doi: 10.1002/(sici)1520-6777(1997)16:1<1::aid-nau1>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 65.Blake C, Abrams P. Non invasive techniques for the measurement of isovolumetric bladder pressure. J Urol. 2004;171:12–19. doi: 10.1097/01.ju.0000102685.44036.b9. [DOI] [PubMed] [Google Scholar]
- 66.Schafer W, Kirschner-Hermans R, Jakse G. Non invasive presure/flow measurement for precise grading of bladder outflow obstruction. J Urol. 1994;151(supp):323A. [abstract] [Google Scholar]
- 67.McRae LP, Bottaccini MR, Gleason DM. Non invasive quantitive method for measuring isovolumetric bladder pressure and urethral resistance in the male: I. Experimental validation of the theory. Neurourol Urodyn. 1995;14:101–114. doi: 10.1002/nau.1930140202. [DOI] [PubMed] [Google Scholar]
- 68.Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function. BJU Int. 1999;84:14–15. doi: 10.1046/j.1464-410x.1999.00121.x. [DOI] [PubMed] [Google Scholar]
- 69.Lim CS, Abrams P. The Abrams-Griffiths nomogram. World J Urol. 1995;13:34–39. doi: 10.1007/BF00182664. [DOI] [PubMed] [Google Scholar]