Abstract
Despite the deceptively simple description of benign prostatic hyperplasia (BPH), the actual relationship between BPH, lower urinary tract symptoms (LUTS), benign prostatic enlargement, and bladder outlet obstruction is complex and requires a solid understanding of the definitional issues involved. The etiology of BPH and LUTS is still poorly understood, but the hormonal hypothesis has many arguments in its favor. There are many medical and minimally invasive treatment options available for affected patients. In the intermediate and long term, minimally invasive treatment options are superior to medical therapy in terms of symptom and flow rate improvement; tissue ablative surgical treatment options are superior to both minimally invasive and medical therapy.
Key words: Benign prostatic hyperplasia, Lower urinary tract symptoms, Bladder outlet obstruction, α-adrenergic receptor blockers, 5α-reductase inhibitors, Minimally invasive surgical therapy, Interstitial laser coagulation
Benign prostatic hyperplasia (BPH) refers to the nonmalignant growth of the prostate observed very commonly in aging men. Although on the surface this statement seems straightforward and simple, there are considerable definitional problems associated with the condition that subsequently lead to problems with epidemiologic definitions, calculations of incidence and prevalence rates, and, ultimately, difficulties with formalizing therapeutic algorithms.
BPH, the actual hyperplasia of the prostate gland, develops as a strictly age-related phenomenon in nearly all men, starting at approximately 40 years of age. In fact, the histologic prevalence of BPH, which has been examined in several autopsy studies around the world, is approximately 10% for men in their 30s, 20% for men in their 40s, reaches 50% to 60% for men in their 60s, and is 80% to 90% for men in their 70s and 80s. No doubt, when living long enough, most men will develop some histologic features consistent with BPH.1
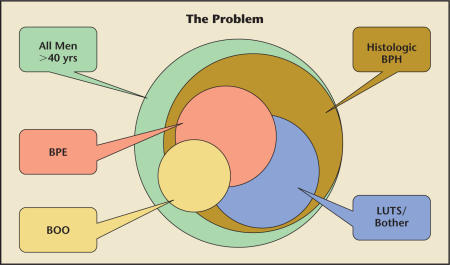
Histologic BPH, although identified by the International Classification of Diseases (ICD) code 600, does not necessarily constitute a problem to the patient. In fact, many men with histologic BPH will never see a doctor for this condition, nor do they ever need any treatment for it. The condition becomes a clinical entity if and when it is associated with subjective symptoms, the most common manifestation being lower urinary tract symptoms (LUTS). It must be recognized, however, that not all men with histologic BPH will develop significant LUTS, although other men who do not have histologic BPH will develop LUTS. Such men might have other conditions of the prostate (prostatitis or prostate cancer), other causes for subvesical outlet obstruction (urethral stricture, bladder neck sclerosis), conditions of the bladder (carcinoma in situ, inflammation, stones), or other conditions leading to the rather nonspecific constellation of symptoms commonly labeled as “LUTS” (Figure 1). The LUTS symptom complex can be conveniently divided into obstructive and irritative symptoms. Among the obstructive symptoms are hesitancy, straining, weak flow, prolonged voiding, partial or complete urinary retention, and, ultimately, overflow incontinence. The often more bothersome irritative symptoms consist of frequency, urgency with urge incontinence, nocturia, and painful urination, as well as small voided volumes. The prevalence of LUTS increases steadily with increasing age. Observations to this effect have been obtained from many cross-sectional studies in various countries and racial groups.2 Not all men with obstructive or irritative voiding symptoms will be bothered by these symptoms, and so will not seek medical attention. Considerable efforts have been expended to understand the reasons men do or do not consult a health care provider when experiencing LUTS. In many cases, these symptoms are accepted as a natural occurrence with aging, and men learn to live with them. Also, the threshold for men to seek consultation with a health care provider for LUTS differs greatly within and between racial groups. Ultimately, however, when men are significantly bothered by these symptoms, they will usually consult a health care provider in hopes of remedying the situation.
Figure 1.
Complex relationship between benign prostatic hyperplasia (BPH), lower urinary tract symptoms (LUTS), benign prostatic enlargement (BPE), and bladder outlet obstruction (BOO).
Another important part of the constellation of LUTS and BPH is the fact that, in aging men, the prostate tends to increase in size (Figure 1). This phenomenon has been investigated in longitudinal and cross-sectional studies in various ethnic groups, starting with the original autopsy study conducted by Berry and colleagues.3 Since then, many other studies have been performed, mostly using transrectal ultrasonography to measure the prostate in men in various decades of life. These studies demonstrate that across a wide spectrum of racial and ethnic groups, prostate size increases from 25 g to 30 g for men in their 40s to 30 g to 40 g for men in their 50s and to 35 g to 45 g for men in their 60s. At the same time, the transition zone of the prostate, which is quite small at approximately 15 g in men in their 40s, increases to approximately 25 g for men in their 60s and 70s.1 It is well understood that the immediate periurethral glans or transition zone of the prostate is the source of the size enlargement, slowly expanding and thus compressing the peripheral zone of the prostate. As Figure 1 indicates, certainly not all men with histologic BPH will develop benign prostatic enlargement (BPE). Furthermore, not all men with LUTS or bothersome symptomatology will have concomitant BPE, and not all men with BPE will have bothersome symptoms. Many men with significant LUTS and bother have a normalsized prostate, whereas many men with large prostates present with surprisingly few, if any, symptoms. In the past, this latter condition has been called “silent prostatism.”
The last part of the complex relationship is the issue of bladder outlet obstruction (BOO) (Figure 1). This refers to the presence of a pressure gradient at the bladder neck/prostatic urethra, which can be measured precisely by invasive urodynamic studies. As with the previous observation, not all men with enlarged prostates and bothersome LUTS will have BOO, whereas certainly there are other causes for BOO than BPH and BPE. For example, a primary bladder neck sclerosis, a urethral stricture, or other conditions might cause significant obstruction while not being associated with histologic BPH. BOO can be measured by invasive pressure-flow studies or noninvasively tested for by urinary flow rate recordings. It has been shown that the maximum urinary flow rate decreases with advancing age, either in the absence or presence of BPH and LUTS.4 Girman and colleagues4 have shown that the maximum urinary flow rate for men in their early 40s is approximately 20.3 mL/s, whereas it decreases for men in their 70s to 11.5 mL/s. Abrams5 and others have demonstrated that a peak or maximum urinary flow rate of less than 10 mL/s indicates the presence of a subvesical obstruction in 90% of patients, whereas in patients with a maximum urinary flow rate of greater than 15 mL/s, subvesical obstruction is present in only 30%. Of the men in the indeterminate group, with a peak flow rate of 10 to 15 mL/s, approximately 2 out of 3 will have subvesical obstruction.5
Thus, the commonly used term “BPH” actually refers to just a histologic condition, namely the presence of stromal-glandular hyperplasia within the prostate gland. This condition, although it is the most commonly cited and the one associated with a recognizable ICD-9 code, might or might not be associated with the presence of bothersome LUTS, anatomic enlargement of the prostate (BPE), and a compression of the urethra with compromised urinary flow and BOO.
Despite many decades of intense research, the etiology of BPH is still poorly understood. Of the dominant hypotheses, the hormonal or dihydrotestosterone (DHT) hypothesis is most often invoked. It is clear that male gender (with functioning testes present at the time of puberty) and aging are paramount to the development of BPH. Additional risk factors include a positive family history, because early BPH may occur as a familial disease. Despite intense epidemiologic research, smoking, obesity, and sexual activity or the lack thereof have not been conclusively linked to the development of BPH. Increased physical activity and alcohol taken in moderation seem to protect from BPH.
As mentioned earlier, BPH in itself might not cause any problem and thus might not call for immediate treatment. Patients most often seek consultation with a health care provider for bothersome LUTS. Much research has demonstrated that bothersome LUTS can interfere with activities of daily living, cause significant impairment of the disease-specific quality of life, and interfere with sexual functioning.6,7 In fact, there is increasing evidence that worse LUTS are associated with increased levels of sexual dysfunction. A large, multinational, survey-based study demonstrated that, independent of age, men with more severe LUTS also more often experienced sexual dysfunction.8 In this context, sexual dysfunction refers to erectile and ejaculatory functionality. The exact pathophysiology for this relationship has not been fully understood, and it is still unclear whether this is a causal or coincidental relationship, but it is noteworthy that men with sexual dysfunction often have LUTS, and vice versa.
BPE and BOO have been linked to outcomes other than symptom severity that are of significance and thus are worthy of the attention of health care providers. For example, the incidence rates of acute urinary retention episodes and subsequent surgical interventions are higher in men with larger prostate glands compared with those with smaller prostates. Also, subvesical obstruction or BOO might be responsible for secondary changes of the bladder anatomy and function, urinary tract infections, formation of bladder stones, and ultimately deterioration of the upper urinary tract with renal failure.
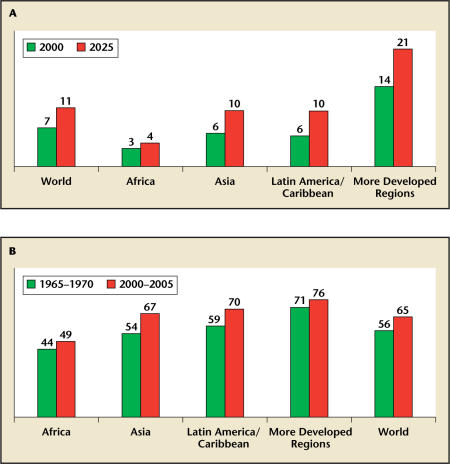
The high prevalence of histologic BPH, bothersome LUTS, BPE, and BOO has been emphasized, and the number of patients presenting with these symptoms to health care providers engaged in the care of such patients will likely increase significantly over the next decades. Estimates from the United Nations9 demonstrate that the percentage of the population aged 65 years or older increased significantly between 2000 and 2005, both in underdeveloped and more developed regions, and from 7% to 11% worldwide (Figure 2A). In addition, life expectancy has changed worldwide from 56 years for the observation period 1965 to 1970 to 65 years for 2000 to 2005. Again, the more developed regions have a longer life expectancy, but the incremental increase is greater in Africa, Asia, and Latin America and the Caribbean regions (Figure 2B).
Figure 2.
Trends in aging and life expectancy. (A) Percentage of population aged 65 years and older, by world region. (B) Trends in life expectancy at birth (in years), by world region. Data from United Nations.9
Diagnosis and Evaluation
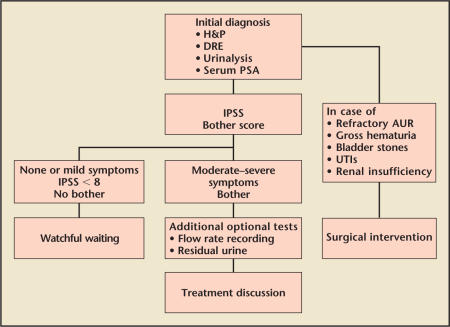
The evaluation of men presenting with LUTS to a health care provider was summarized by the American Urological Association (AUA) BPH Guidelines Committee and is illustrated in Figure 3.10 All patients should undergo a careful history, focusing on diseases specific to the genitourinary tracts, and a physical examination including a careful digital rectal examination (DRE). DRE is notoriously unreliable in assessing the size of the prostate. In fact, DRE has been shown to underestimate the size of the prostate, with the degree of underestimation increasing with the actual size of the prostate.11 However, despite these shortcomings, it is important to assess the prostate in terms of its shape, symmetry, nodularity, and firmness, because even today some men are found to have prostate cancer on the basis of DRE-detected subtle abnormalities in terms of symmetry or nodularity. In addition, urinalysis and a serum prostate-specific antigen (PSA) assay is recommended as part of the additional diagnosis. However, the performance of a serum PSA measurement should depend on the patient’s age and his circumstances. In a patient with a life expectancy estimated to be less than 10 years, and/or if the knowledge of the PSA level would not change the type of therapeutic intervention, serum PSA assay is not recommended.
Figure 3.
Guidelines for the evaluation of men with lower urinary tract symptoms and benign prostatic hyperplasia. H&P, history and physical examination; DRE, digital rectal examination; PSA, prostate-specific antigen; IPSS, International Prostate Symptom Score; AUR, acute urinary retention; UTI, urinary tract infection. Adapted from the American Urological Association Practice Guidelines Committee.10
Upon initial presentation, certain patients might be immediately referred to minimally invasive or surgical treatment. In the past, men presenting with refractory urinary retention were believed to require immediate surgical intervention. Nowadays, however, these patients are given a trial without catheter with concomitant administration of an α-adrenergic receptor blocker, such as alfuzosin or tamsulosin. Patients with gross hematuria might be treated with 5α-reductase inhibitors, such as dutasteride or finasteride, if any causes for the hematuria other than BPH have been excluded. Even patients with bladder stones do not necessarily need to be referred for surgery. Studies have shown that after cystolithotomy, patients might be successfully treated with α-adrenergic receptor blockade without requiring formal tissue ablative surgery. Patients with recurrent urinary tract infections clearly secondary to BPH, BPE, or BOO and those who already have developed deterioration of their bladder and/or upper urinary tract, however, might benefit from immediate surgical intervention.
The vast majority of patients are further evaluated by quantitative symptom score assessment. There is a large variety of self-administration questionnaires that may be given to patients to assess symptom frequency and severity, interference with daily activity, quality of life, issues of urinary continence or incontinence, sexual functioning, and other health-related general or disease-specific quality-of-life issues. The most common of these instruments is the AUA Symptom Score, also known as the International Prostate Symptom Score (IPSS).12 This is a 7-item questionnaire addressing the most common irritative and obstructive voiding symptoms. The questionnaire is self-administered and elicits a response score ranging from 0 to 35 points. Men scoring from 0 to 7 points are classified as not or mildly symptomatic, those scoring between 8 and 18 points as moderately symptomatic, and those scoring 19 points or greater as severely symptomatic. Multiple studies have demonstrated that there is a strong correlation between symptom frequency and severity as measured by the AUA Symptom Score/IPSS and other measures, such as the Symptom Problem Index, the BPH Impact Index,13 and other disease-specific quality-of-life measures. The most commonly used measure of sexual function is the International Index of Erectile Function, a multidimensional scale for the assessment of erectile dysfunction.14–16
It is generally recommended that those patients scoring less than 8 points and who exhibit no or insignificant bother due to these symptoms be classified as not or mildly symptomatic, and the recommendation most often made is for watchful waiting or yearly reevaluation. Those patients who score in the moderate or severe range on the IPSS and report bother from these symptoms might undergo additional or optional testing before a discussion of treatment options. This additional or optional testing can be modified depending on the patient’s presentation, the situation and training of the health care provider, and the socioeconomic circumstances. Although such tests are not always necessary, specifically before the initiation of medical therapy, they might be helpful in patients with a complex medical history, neurological diseases known to affect bladder function, prior failed BPH therapy, and certainly in those patients desiring minimally invasive or surgical therapy.
Urinary flow rate recording is a noninvasive way to determine the intensity or strength of the urinary stream. As discussed above, a maximum urinary flow rate of greater than 15 mL/s is considered nearly in the normal range, whereas a maximum flow rate of less than 10 mL/s is highly suggestive of outlet obstruction.
Measurement of postvoid residual urine can be performed by transabdominal ultrasonography or in-and-out catheterization, the former being the preferred method. Postvoid residual urine values differ substantially over time within an individual and between individuals. They have not been shown to be reliable predictors of the natural history of the disease and/or the response to treatment. However, it is widely accepted that rising amounts of residual urine and decreasing voiding efficiency are associated with worsening of the condition and a greater likelihood of acute urinary retention with subsequent need for surgery.
Invasive pressure-flow studies or formal urodynamic studies are the best tests to determine whether a patient is obstructed at the level of the bladder neck. Appropriate nomograms have been established for normative values regarding the pressure-flow parameters, and it is commonly accepted that the best marker of obstruction is the pressure within the bladder generated by the detrusor muscle at the time of the maximum urinary flow rate.17,18
Imaging studies that could be of use in the evaluation of men presenting with LUTS and suspected to have BPH, BPE, or BOO are ultrasound assessments of the prostate performed either transabdominally or transrectally. In fact, transrectal ultrasound of the prostate is the most common imaging modality for the assessment of prostate size and shape. Inasmuch as prostate size is predictive of the natural history of the disease and the subsequent need of surgery but also important in determining the appropriateness of certain therapeutic interventions, it is a recommended test in those patients seeking certain minimally invasive (transurethral microwave thermotherapy [TUMT], transurethral needle ablation [TUNA]) or surgical therapeutic options, while it is not needed or helpful prior to other minimally invasive interventions such as interstitial laser coagulation (ILC) of the prostate.
Imaging of the upper urinary tract by intravenous urography or computerized tomography is rarely indicated because patients with LUTS and BPH do not have an increased incidence of significant lesions (eg, renal tumors or stones) of the upper urinary tract compared with age-matched controls.
Endoscopic examination of the lower urinary tract by cystourethroscopy is also rarely indicated before embarking on surgical treatment. However, the anatomy of the prostate, the appearance of the bladder neck, the presence or absence of an intravesical lobe, and the condition of the bladder muscle and mucosa might alter the surgical approach (eg, transurethral resection vs incision of the prostate) and assessment of these factors is indicated before embarking on minimally invasive interventions such as ILC or other surgical procedures.10
Medical Therapy
There are many therapeutic options available to those men suffering from bothersome LUTS, BPE, or BOO. Depending on the individual circumstances and presentation, as well as the familiarity and comfort the health care provider has with the various interventions, a multitude of medical or surgical interventions might be contemplated.
For those men presenting with mild symptoms and those with moderate symptoms but limited bother due to their symptoms, watchful waiting (ie, a strategy of yearly reevaluation) and reassurance are certainly appropriate. This strategy is based on the observation that progression of symptoms in these patients is rare and development of serious complications is uncommon.
Among the medical therapy options, patients and physicians can choose from a large variety of phytotherapeutic or herbal preparations, α-adrenergic receptor blockers, 5α-reductase inhibitors, or choose combination therapy including the use of anticholinergics in case of a preponderance of irritative symptoms consistent with overactive bladder.
The use of phytotherapeutics has increased significantly over the last decade in the United States, whereas it has always been very popular in Europe. Among the more popular natural compounds are the fruit of the American dwarf palm tree (saw palmetto or Serenoa repens), an extract made from the bark of the African plum tree (Pygeum africanum), pumpkin seeds, rye pollen extracts, South African star grass roots, the root of the stinging nettle, or the purple cone flower. Many smaller and short-term studies have demonstrated improvement in symptoms with such compounds, but there is a paucity of well-conducted, long-term, or placebo-controlled studies for any of these products, and many of the results are conflicting. There are excellent reviews available regarding this topic.19,20 In general, there is limited evidence supporting the presumed mechanisms of action for these various compounds, and the precise pathophysiologic rationale for their use is less well understood compared with the 2 classes of chemicals that are commonly used for the treatment of bothersome LUTS associated with BPH. In addition, there is a significant lot-to-lot variability in the actual ingredients, and quality control of these products is, comparatively speaking, poor.21 Health care providers should counsel their patients appropriately. Nonetheless, if patients feel that they are subjectively improved, it will prove difficult for the health care provider to discourage the use of these over-the-counter agents.
By far the most commonly used class of drugs for the treatment of bothersome LUTS associated with BPH is the α-adrenergic receptor blockers. Here, a clear pathophysiologic rationale is present. The tone of the smooth muscle is mediated by α1-adrenergic receptors. An increase in the tone leads to a reduction in the urinary flow rate (ie, obstruction) and worsening of LUTS. Accordingly, a blockage of the receptor leads to improvement of the urinary flow rates and LUTS. Additionally, central α-receptors and the effect of these agents on those receptors will likely play an additional role in the improvement of LUTS in men with BPH. Of the 3 α1-adrenergic receptor subtypes, α1A, α1B, and α1D, by far the most important in the prostate is the α1A receptor, constituting approximately 80% according to immunohistochemistry and other analytical methods.10,22–26
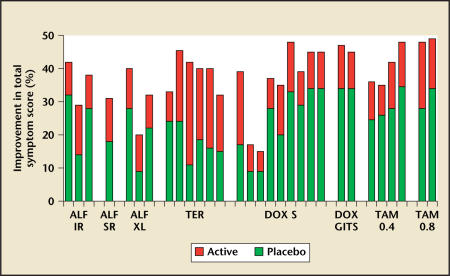
Among the available α1-adrenergic receptor blockers in the United States are the short-acting selective α1 blocker prazosin, the long-acting selective α1 blockers terazosin, doxazosin, alfuzosin, and the more subtype-selective α1A-receptor blocker tamsulosin. Although there are subtle differences between these drugs in terms of their side-effect profiles, they are fundamentally all equally effective in alleviating bothersome LUTS and improving urinary flow rates (Figure 4). Both terazosin (available as 1, 2, 5, and 10 mg) and doxazosin (available as 1, 2, 4, and 8 mg) require titration owing to the first dose effect to reach the maximum recommended doses of 10 and 8 mg, respectively. Tamsulosin is available in 0.4-mg tablets and might be increased to 2 tablets daily or 0.8 mg. Alfuzosin is available only as a single, 10-mg slow-release formulation, and no dose titration is recommended.
Figure 4.
Comparison of the improvement in International Prostate Symptom Score by various α-blockers. Effect of α1-adrenergic receptor antagonists on total symptom score in placebo-controlled studies. Total number of patients: alfuzosin (ALF), n = 2208; terazosin (TER), n = 3229; doxazosin (DOX), n = 3947; and tamsulosin (TAM), n = 1331. IR, immediate release; SR, sustained release; S, standard; GITS, gastrointestinal. Additional benefit with α-blockers over placebo is approximately 10% to 15%. Reproduced with permission from Djavan et al.27
Depending on the baseline symptom status of a patient, appropriate dose therapy with an α-adrenergic receptor blocker will improve the IPSS by 3 to 6 points or by as much as 50%; however, a significant proportion of this improvement is due to the so-called placebo effect.27
In contrast to the relatively equal efficacy of all 4 drugs currently available, there are some differences regarding the adverse event spectrum. Terazosin and doxazosin induce more dizziness, fatigue, and asthenia, whereas tamsulosin induces more ejaculatory disturbances. However, actual discontinuation due to any of these side effects is not common, and discontinuation rates are relatively similar among these compounds.
It is noteworthy that none of the α1-adrenergic receptor blockers have ever been shown to significantly alter urodynamic parameters, serum PSA level, or prostate volume. Thus, these drugs are not able to alter the natural history of the disease significantly.
In contrast, the second class of compounds has remarkable abilities in terms of altering the natural history of the disease. These compounds are called 5α-reductase inhibitors, and there are 2 drugs in this class, namely finasteride and dutasteride. Serum testosterone, an intrastromal cell in the prostate, is converted by the 5α-reductase isoenzyme to DHT, which is a far more potent androgenic steroid. DHT enters the epithelial cell, binds to the androgen receptor, and then induces alterations of the deoxyribonucleic acid, leading ultimately to such metabolic effects as protein synthesis and secretion and growth of the prostate.
Finasteride was introduced in the 1990s for the treatment of BPH.28 It has been shown to reduce DHT in the serum by 70% and in the prostate by up to 90%. At the same time, serum testosterone increases by 10%. Over the course of treatment, the serum PSA level is reduced by 50%, and over time total prostate volume decreases by 15% to 25% because of apoptosis and shrinkage of the glandular epithelial compartment in both the transition and peripheral zones of the prostate. It was later recognized that there were actually 2 isoenzymes of 5α-reductase, namely types I and II.29 Ten years after the introduction of finasteride to the marketplace, a second compound was approved that inhibits both 5α-reductase types I and II, namely dutasteride.30 Despite the difference in terms of their actual pathophysiologic effect on types I and II of the 5α-reductase isoenzymes, finasteride and dutasteride exhibit remarkably similar clinical efficacy, as evidenced by a direct head-to-head comparison trial. Serum DHT is suppressed by finasteride by approximately 70%, whereas dutasteride suppresses it by more than 90% because of the additional inhibition of type I isoenzyme. Serum PSA reduction, however, remains at approximately 50% with both compounds. Similarly, prostate volume is reduced by 15% to 30% with both drugs in a similar manner. Finasteride has a serum half-life of 6 to 8 hours, whereas that of dutasteride is 5 weeks. Improvement in IPSS is similar for finasteride and dutasteride and significantly superior to that with placebo. However, on balance, it is inferior to the improvement achieved with most α-adrenergic receptor blockers. Improvement in maximum urinary flow rate by approximately 2.0 mL/s is achieved, which is similar to that achieved by α-adrenergic receptor blockers. The fundamental difference between the 5α-reductase inhibitors and the α-receptor blockers is the ability to interfere with the natural history of the disease. In long-term studies, both drugs have been associated with a greater than 50% reduction in the risk of acute urinary retention and the risk for surgical intervention, and the relative benefit in terms of risk reduction increases with increasing prostate size and increasing serum PSA values.31–36
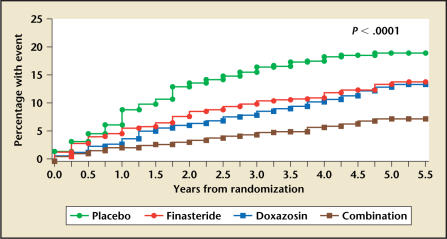
The field of medical therapy for BPH was revolutionized in 2003 when results of the Medical Therapy of Prostatic Symptoms trial were published. In this trial, more than 3000 men with bothersome LUTS and BPH were treated over 4 to 5 years with either placebo, doxazosin, finasteride, or a combination of doxazosin and finasteride.37,38 This trial was not designed to study the efficacy and safety of these drugs so much as to determine the ability of these compounds to prevent the progression of BPH. Progression was defined as either a worsening in the symptom score by 4 or more points, development of acute urinary retention, recurrent urinary tract infections, socially unacceptable incontinence, or development of renal failure. Whereas approximately 20% of the placebo-treated patients developed such progression over time, this risk was reduced by either doxazosin or finasteride by 30% to 40% in a similar manner. Combination therapy, however, reduced the risk by more than 60%, which was statistically superior to both placebo and either one of the single-arm therapies (Figure 5). When these data were further analyzed, it became apparent that the risk of urinary retention was mostly prevented by finasteride, whereas the risk of symptomatic progression was prevented by both drugs, although doxazosin performed slightly better. Not part of the composite endpoint was the risk of crossing over to surgical therapies for BPH. The risk of surgical therapy was not affected by doxazosin, whereas it was reduced significantly by finasteride and accordingly by combination medical therapy. The cumulative incidence of BPH progression, invasive therapy, or crossing over to open-label medical therapy throughout the trial was 26% in the placebo group, 22% and 18% in the doxazosin and finasteride groups, respectively, and 12% in the combination group. This study demonstrated clearly that in certain select patients, namely those with larger glands and likely higher serum PSA levels, combination therapy might be superior because it both improves the bothersome symptoms and prevents symptomatic and other forms of progression in the future.
Figure 5.
Cumulative incidence of overall progression of benign prostatic hyperplasia in the Medical Therapy of Prostatic Symptoms trial by treatment group. Reproduced with permission from McConnell et al.38
Medical therapy for BPH has thus been found to be very effective in the management of men with LUTS and BPH. However, given that the IPSS ranges from 0 to 35 points, critical voices have long raised concerns that the actual magnitude of improvement with either one of the medical therapies is, overall, disappointing. There are almost no medical therapy trials in which a margin of improvement of greater than 5 or 6 points is achieved, and in the vast majority of trials the margin of improvement is between 3 and 6 points for α-blockers and 2 and 4 points for the 5α-reductase inhibitors. Much of the symptomatic improvement in fact is due to the placebo effect. This disappointment with the magnitude of symptomatic improvement has prompted many physicians to suggest to their patients minimally invasive or surgical interventions to achieve greater improvement in the symptoms and thereby greater satisfaction on the part of their patients. The understandable concern, however, is that more-invasive treatments (ie, minimally invasive or surgical interventions) are associated with a greater risk for adverse events.
Minimally Invasive Therapy and Surgery
The AUA Guidelines recommend a host of minimally invasive therapies for the treatment of bothersome LUTS with BPH. Among the recommended treatments are TUMT, TUNA, and in select patients, the placement of a urethral stent. The AUA Guidelines Committee designates ILC and water-induced thermotherapy as emerging technologies and both ethanol injection and high-intensity focused ultrasound as investigational.10
Minimally invasive therapies are chosen by patients and health care providers because they fill a critical need between medications and surgical procedures. Patients may have adverse effects from drugs or may not experience the hoped for improvement in symptoms, or they may find the need for daily medication both bothersome and costly. On the other hand, these interventions done in the office are well suited for those patients not willing or medically not fit to have a surgical procedure done under general anesthesia.
There are many surgical therapies available, all of which require some form of anesthesia, be it spinal, epidural, or general. They differ in the energy employed and in the method by which tissue is incised, resected, or vaporized. The recommended surgical therapies are transurethral incision of the prostate, transurethral resection of the prostate (TURP), electrovaporization of the prostate, transurethral laser vaporization or coagulation, transurethral Holmium laser resection or enucleation, and open prostatectomy. The potassium-titanyl-phosphate (KTP) laser prostatectomy is another form of vaporization of the prostate and is designated as an emerging technology in the AUA Guidelines.
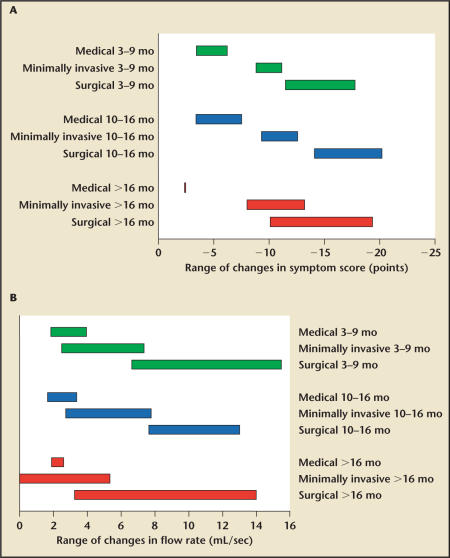
Both in the intermediate and long term, minimally invasive treatment options are superior to medical therapy in terms of symptom and flow rate improvement, whereas the tissue ablative surgical treatment options are superior to both minimally invasive and medical therapy options (Figure 6A and B).
Figure 6.
Comparisons of (A) symptom score and (B) flow rate improvement by treatment modality and follow-up. Data from the American Urological Association Practice Guidelines Committee.10
There are fundamental differences between the trials conducted with medical therapy versus minimally invasive interventions. Although all minimally invasive interventions can be conducted in the outpatient or clinic setting without the use of regional or general anesthesia, there are substantive and important design differences that are worthy of consideration. Most medical therapy trials are preceded by a placebo lead-in. During placebo lead-in, all patients receive placebo; thereafter, they are randomized to either placebo or active therapy. At the time of randomization, the symptom score is reassessed, and the change from randomization to endpoint is calculated as the actual symptom improvement. This ignores the fact that the patient already experienced improvement during the lead-in period owing to the placebo effect. In minimally invasive interventions, however, there is no such thing as a placebo lead-in or a “sham control lead-in.” Rather, patients are treated and followed, and the therapeutic benefit is calculated from the treatment to the endpoint of observation. Thus, one might suspect that minimally invasive treatment trials result in a numerically larger symptom score improvement, because of the fundamental differences in trial design. One should note, of course, that a placebo or sham lead-in period would be next to impossible to carry out in a trial of a minimally invasive intervention. It would require, for example, performing a sham TUMT, followed by another assessment 4 weeks later, and then the patients would be randomized to receive another sham TUMT or a real TUMT—a protocol design unlikely to be approved by any investigational review board in the United States or elsewhere!
Given this and also the notion that minimally invasive treatments are offered to patients who fail on medical therapy, it would be most important to determine whether there are real differences in efficacy and safety, both in the short and long term, between medical therapy and minimally invasive surgical therapy (MIST). However, owing to the difficulty in designing and carrying out such trials, there is an extreme paucity of data regarding the subject.
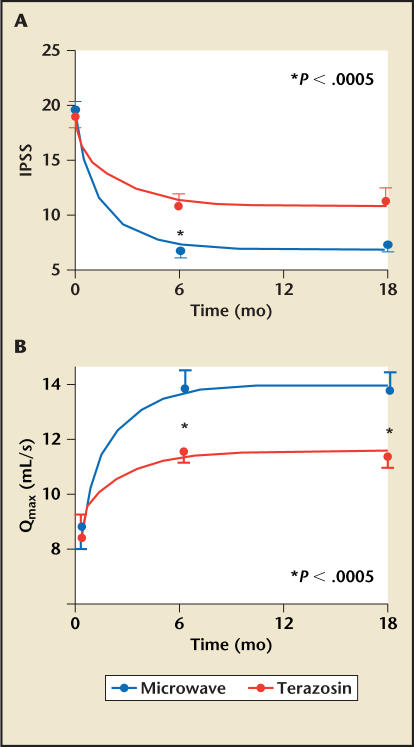
In 1999, Dvajan and colleagues39 conducted a trial comparing TUMT with α-blocker therapy in a randomized, controlled trial. In this study, 52 patients with symptomatic BPH received terazosin, and 51 underwent high-energy TUMT with topical anesthesia. At 2 weeks of follow-up, the terazosin group exhibited greater improvement compared with the TUMT group in terms of IPSS, peak flow rate, and quality-of-life score. At 12 weeks and 6 months, however, this pattern was reversed: the TUMT group achieved significantly greater improvement compared with the terazosin group in all 3 parameters. By 6 months, a 50% or greater improvement in symptom score was achieved in 78.4% of patients in the TUMT group, compared with 32.7% in the terazosin group. Nine patients in the terazosin group and 1 in the TUMT group withdrew because of side effects or lack of efficacy from the study. The conclusion of this pilot study was that terazosin afforded more rapid improvement in symptoms, voiding function, and quality of life, whereas high-energy TUMT offered markedly superior outcomes at 12 weeks to 6 months (Figure 7).
Figure 7.
Improvement in (A) International Prostate Symptom Score (IPSS) and (B) peak urinary flow rate (Qmax) over time with terazosin versus transurethral microwave thermotherapy. Updated from Djavan et al.39
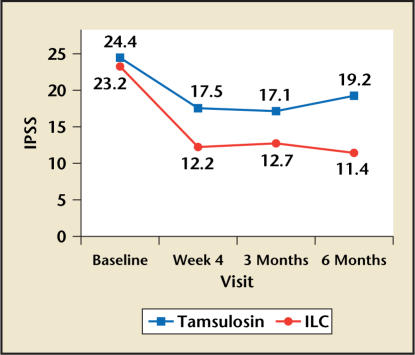
It was nearly 5 years before a second trial compared another minimally invasive treatment with a classic medical therapy. In this multicenter trial, patients were randomized to receive either tamsulosin (0.4 mg daily) or to be treated by ILC with the Indigo® Optima laser (Ethicon Endo-Surgery, Cincinnati, OH).40 This study is not completely enrolled, nor is the follow-up complete. Preliminary data of 40 patients followed up to 6 months suggest that the tamsulosintreated patients experience an improvement in IPSS from 24.4 to 19.2 points, whereas the ILC-treated patients have a numerically larger improvement, from 23.2 to 11.4 points for the same period of observation (Figure 8). The improvements in irritative and obstructive subscores and the quality-of-life improvements were also superior in the ILC group (see Table 2 in the article by Dr. Brawer in this supplement). Nine of 11 patients in the ILC group and 5 of 14 in the tamsulosin group considered themselves significantly improved at 6 months of follow-up. Adverse events, including retention, were rare. Ongoing follow-up of the treated patients and further enrollment will likely shed additional light on the differences between medical therapy and MIST for LUTS and BPH.
Figure 8.
Improvements in mean International Prostate Symptom Score (IPSS) in a randomized trial of tamsulosin versus interstitial laser coagulation (ILC) with the Indigo Optima laser. Presented by Roehrborn and associates at the American Urological Association Annual Meeting, May 25, 2005, San Antonio, TX.
There is evidence to suggest that ILC compares favorable with the other end of the spectrum, that is, with a TURP.41 In a randomized multicenter study involving 72 men with BPH, the symptomatic and quality-of-life improvement was similar between the ILC- and TURP-treated patients, while the flow rate improvements favored the TURP procedure slightly, but not significantly (16.5 vs 13.9 mL/s, respectively). In addition, adverse events were less common in the ILC group, particularly relating to sexual function.
A third and very ambitious effort to compare medical therapy and minimally invasive treatments was recently undertaken by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases. The so-called MIST Consortium was scheduled to randomize patients to best medical therapy, consisting of an α-blocker and a 5α-reductase inhibitor combined, versus transurethral needle ablation, versus TUMT. The MIST Consortium, however, experienced great difficulty in patient enrollment and randomization, and thus the Data Safety and Monitoring Board recommended termination of the study due to lack of recruitment. Although this is certainly a regrettable development, further data from the continuing trial of tamsulosin versus ILC therapy with the Indigo Optima laser will be awaited with great anticipation. These data could shed more light on the actual differences between medical therapy and minimally invasive therapeutic interventions for BPH.
Summary
Despite the deceptively simple description of BPH, the actual relationship between BPH, LUTS, BPE, and BOO is rather complex and requires a solid understanding of the definitional issues involved. The etiology of BPH and LUTS is still poorly understood, but the hormonal hypothesis has many arguments in its favor. There are many medical and minimally invasive treatment options available for affected patients. Although it is commonly believed that medical therapy is inferior to MIST, there is a paucity of studies evaluating this question in a direct side-by-side comparison.
Main Points.
“Benign prostatic hyperplasia” (BPH) refers to the presence of stromal-glandular hyperplasia within the prostate gland; this condition, may or may not be associated with bothersome lower urinary tract symptoms (LUTS), anatomic enlargement of the prostate, and a compression of the urethra with compromised urinary flow and bladder outlet obstruction (BOO).
Bothersome LUTS can interfere with activities of daily living, cause significant impairment of disease-specific quality of life, and interfere with sexual functioning; BOO might be responsible for secondary changes of the bladder anatomy and function, urinary tract infections, formation of bladder stones, and ultimately deterioration of the upper urinary tract with renal failure.
All patients presenting with LUTS should undergo a careful history, focusing on diseases specific to the genitourinary tracts, and a physical examination including a careful digital rectal examination; most patients are further assessed by quantitative symptom score assessment, such as the International Prostate Symptom Score (IPSS).
Patients with moderate or severe scoring on the IPSS might undergo additional or optional testing, such as urinary flow rate recording, measurement of postvoid residual volumes, invasive pressure-flow studies, imaging studies, and (rarely) cystourethroscopy.
Among the medical therapy options, patients and physicians can choose from a large variety of phytotherapeutic or herbal preparations, α-adrenergic receptor blockers, 5α-reductase inhibitors, or combination therapy including the use of anticholinergics (in cases of overactive bladder).
In the intermediate and long term, minimally invasive treatment options are superior to medical therapy in terms of symptom and flow rate improvement; tissue ablative surgical treatment options are superior to both minimally invasive and medical therapy.
References
- 1.Roehrborn C, McConnell J. Etiology, pathophysiology, epidemiology and natural history of benign prostatic hyperplasia. In: Walsh P, Retik A, Vaughan E, Wein A, editors. Campbell’s Urology. 8th ed. Philadelphia: Saunders; 2002. pp. 1297–1336. [Google Scholar]
- 2.Girman CJ. Population-based studies of the epidemiology of benign prostatic hyperplasia. Br J Urol. 1998;82(suppl 1):34–43. doi: 10.1046/j.1464-410x.1998.0820s1034.x. [DOI] [PubMed] [Google Scholar]
- 3.Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984;132:474–479. doi: 10.1016/s0022-5347(17)49698-4. [DOI] [PubMed] [Google Scholar]
- 4.Girman CJ, Panser LA, Chute CG, et al. Natural history of prostatism: urinary flow rates in a community-based study. J Urol. 1993;150:887–892. doi: 10.1016/s0022-5347(17)35640-9. [DOI] [PubMed] [Google Scholar]
- 5.Abrams P. Objective evaluation of bladder outlet obstruction [review] Br J Urol. 1995;76(suppl 1):11–15. [PubMed] [Google Scholar]
- 6.Girman CJ, Jacobsen SJ, Rhodes T, et al. Association of health-related quality of life and benign prostatic enlargement. Eur Urol. 1999;35:277–284. doi: 10.1159/000019861. [DOI] [PubMed] [Google Scholar]
- 7.Girman CJ, Jacobsen SJ, Tsukamoto T, et al. Health-related quality of life associated with lower urinary tract symptoms in four countries. Urology. 1998;51:428–436. doi: 10.1016/s0090-4295(97)00717-6. [DOI] [PubMed] [Google Scholar]
- 8.Rosen R, Altwein J, Boyle P, et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7) Eur Urol. 2003;44:637–649. doi: 10.1016/j.eururo.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 9.United Nations. World Population Prospects: The 2002 Revision (medium scenario) New York: United Nations; 2003. [Google Scholar]
- 10.American Urological Association Practice Guidelines Committee. AUA guidelines on management of benign prostatic hyperplasia (2003). Chapter 1: diagnosis and treatment recommendations. J Urol. 2003;170(2 Pt 1):530–547. doi: 10.1097/01.ju.0000078083.38675.79. [DOI] [PubMed] [Google Scholar]
- 11.Roehrborn CG, Girman CJ, Rhodes T, et al. Correlation between prostate size estimated by digital rectal examination and measured by transrectal ultrasound. Urology. 1997;49:548–557. doi: 10.1016/s0090-4295(97)00031-9. [DOI] [PubMed] [Google Scholar]
- 12.Barry MJ, Fowler FJ, Jr, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–1557. doi: 10.1016/s0022-5347(17)36966-5. discussion 1564. [DOI] [PubMed] [Google Scholar]
- 13.Barry MJ, Fowler FJ, Jr, O’Leary MP, et al. Measuring disease-specific health status in men with benign prostatic hyperplasia. Measurement Committee of the American Urological Association. Med Care. 1995;33(4 suppl):AS145–AS155. [PubMed] [Google Scholar]
- 14.Rosen RC, Cappelleri JC, Gendrano N., 3rd The International Index of Erectile Function (IIEF): a state-of-the-science review. Int J Impot Res. 2002;14:226–244. doi: 10.1038/sj.ijir.3900857. [DOI] [PubMed] [Google Scholar]
- 15.Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–326. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 16.Rosen RC, Riley A, Wagner G, et al. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 17.Abrams P. In support of pressure-flow studies for evaluating men with lower urinary tract symptoms [editorial] [see comments] Urology. 1994;44:153–155. doi: 10.1016/s0090-4295(94)80119-3. [DOI] [PubMed] [Google Scholar]
- 18.Eri LM, Wessel N, Berge V. Test-retest variation of pressure flow parameters in men with bladder outlet obstruction. J Urol. 2001;165:1188–1192. [PubMed] [Google Scholar]
- 19.Lowe FC. Phytotherapy in the management of benign prostatic hyperplasia. Urology. 2001;58(6) suppl 1:71–76. doi: 10.1016/s0090-4295(01)01303-6. discussion 76–77. [DOI] [PubMed] [Google Scholar]
- 20.Lowe FC, Dreikorn K, Borkowski A, et al. Review of recent placebo-controlled trials utilizing phytotherapeutic agents for treatment of BPH. Prostate. 1998;37:187–193. doi: 10.1002/(sici)1097-0045(19981101)37:3<187::aid-pros8>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 21.Feifer AH, Fleshner NE, Klotz L. Analytical accuracy and reliability of commonly used nutritional supplements in prostate disease. J Urol. 2002;168:150–154. discussion 154. [PubMed] [Google Scholar]
- 22.Schwinn DA. The role of alpha1-adrenergic receptor subtypes in lower urinary tract symptoms. BJU Int. 2001;88(suppl 2):27–34. doi: 10.1046/j.1464-410x.2001.00116.x. discussion 49’50. [DOI] [PubMed] [Google Scholar]
- 23.Schwinn DA, Kwatra MM. Expression and regulation of alpha 1-adrenergic receptors in human tissues. Adv Pharmacol. 1998;42:390–394. [PubMed] [Google Scholar]
- 24.Smith MS, Schambra UB, Wilson KH, et al. Alpha1-adrenergic receptors in human spinal cord: specific localized expression of mRNA encoding alpha1-adrenergic receptor subtypes at four distinct levels. Brain Res Mol Brain Res. 1999;63:254–261. doi: 10.1016/s0169-328x(98)00287-3. [DOI] [PubMed] [Google Scholar]
- 25.McConnell JD. Medical management of benign prostatic hyperplasia with androgen suppression. Prostate Suppl. 1990;3:49–59. doi: 10.1002/pros.2990170506. [DOI] [PubMed] [Google Scholar]
- 26.McConnell JD. The pathophysiology of benign prostatic hyperplasia. J Androl. 1991;12:356–363. [PubMed] [Google Scholar]
- 27.Djavan B, Chapple C, Milani S, Marberger M. State of the art on the efficacy and tolerability of alpha1-adrenoceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Urology. 2004;64:1081–1088. doi: 10.1016/j.urology.2004.07.031. [DOI] [PubMed] [Google Scholar]
- 28.Gormley GJ, Stoner E, Bruskewitz RC, et al. The effect of finasteride in men with benign prostatic hyperplasia. The Finasteride Study Group. N Engl J Med. 1992;327:1185–1191. doi: 10.1056/NEJM199210223271701. [DOI] [PubMed] [Google Scholar]
- 29.Russell DW, Wilson JD. Steroid 5alpha-reductase: two genes/two enzymes. Annu Rev Biochem. 1994;63:25–61. doi: 10.1146/annurev.bi.63.070194.000325. [DOI] [PubMed] [Google Scholar]
- 30.Roehrborn CG, Boyle P, Nickel JC, et al. Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology. 2002;60:434–441. doi: 10.1016/s0090-4295(02)01905-2. [DOI] [PubMed] [Google Scholar]
- 31.Roehrborn CG, Marks LS, Fenter T, et al. Efficacy and safety of dutasteride in the four-year treatment of men with benign prostatic hyperplasia. Urology. 2004;63:709–715. doi: 10.1016/j.urology.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 32.Roehrborn CG, McConnell J, Bonilla J, et al. Serum prostate-specific antigen is a strong predictor of future prostate growth in men with benign prostatic hyperplasia. PROSCAR long-term efficacy and safety study. J Urol. 2000;163:13–20. [PubMed] [Google Scholar]
- 33.Roehrborn CG, Boyle P, Gould AL, Waldstreicher J. Serum prostate specific antigen (PSA) is a reliable surrogate for prostate volume. Urology. 1999;53:581–589. doi: 10.1016/s0090-4295(98)00655-4. [DOI] [PubMed] [Google Scholar]
- 34.Roehrborn CG, Bruskewitz R, Nickel JC, et al. Sustained decrease in incidence of acute urinary retention and surgery with finasteride for 6 years in men with benign prostatic hyperplasia. J Urol. 2004;171:1194–1198. doi: 10.1097/01.ju.0000112918.74410.94. [DOI] [PubMed] [Google Scholar]
- 35.Roehrborn CG, Malice M, Cook TJ, Girman CJ. Clinical predictors of spontaneous acute urinary retention in men with LUTS and clinical BPH: a comprehensive analysis of the pooled placebo groups of several large clinical trials. Urology. 2001;58:210–216. doi: 10.1016/s0090-4295(01)01155-4. [DOI] [PubMed] [Google Scholar]
- 36.Roehrborn CG, McConnell JD, Lieber M, et al. Serum prostate specific antigen concentration is a powerful predictor of acute urinary retention and need for prostate related surgery in men with clinical benign prostatic hyperplasia. PLESS Study Group. Urology. 1999;53:473–480. doi: 10.1016/s0090-4295(98)00654-2. [DOI] [PubMed] [Google Scholar]
- 37.Bautista OM, Kusek JW, Nyberg LM, et al. Study design of the Medical Therapy of Prostatic Symptoms (MTOPS) trial. Control Clin Trials. 2003;24:224–243. doi: 10.1016/s0197-2456(02)00263-5. [DOI] [PubMed] [Google Scholar]
- 38.McConnell J, Roehrborn C, Bautista O, et al. The long-term effects of doxazosin, finasteride and the combination on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2385–2396. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- 39.Djavan B, Roehrborn CG, Shariat S, et al. Prospective randomized comparison of high energy transurethral microwave thermotherapy versus alpha-blocker treatment of patients with benign prostatic hyperplasia. J Urol. 1999;161:139–143. [PubMed] [Google Scholar]
- 40.Roehrborn CR, Rhee EY, Miller SD, et al. Initial results of a randomized multi-center trial comparing the efficacy and safety of Indigo Optima laser treatment with tamsulosin in men with LUTS and BPH [abstract 1565] J Urol. 2005;173(4 suppl):424. [Google Scholar]
- 41.Kursh ED, Concepcion R, Chan S, et al. Interstitial laser coagulation versus transurethral prostate resection for treating benign prostatic obstruction: a randomized trial with 2-year follow-up. Urology. 2003;61:573–578. doi: 10.1016/s0090-4295(02)02420-2. [DOI] [PubMed] [Google Scholar]