Abstract
A protein antigen from an Eimeria protozoan has recently been reported to induce antitumor activity in mice. This activity most likely results from the strong induction of interkeukin-12 (IL-12) and gamma interferon (IFN-γ), which are also essential factors in the establishment of protective immunity against viral infection. We evaluated recombinant Eimeria antigen (rEA) as a potential immunotherapeutic agent in mouse and hamster models of acute phleboviral disease. Punta Toro virus (PTV) was highly sensitive to a single dose of nanogram quantities of rEA in the mouse infection model. Intraperitoneal treatment with rEA also reduced virus load and liver damage associated with PTV infection. IL-12 was elicited following exposure of uninfected mice to quantities of rEA of 10 ng or greater, and the levels peaked at between 3 and 8 h postexposure. IFN-γ release was induced more slowly and required less rEA (1 ng) to produce a significant rise in systemic levels. The induction of IL-12 and IFN-γ involved in the coordination of innate and adaptive immune responses to microbial pathogens required myeloid differentiation factor 88, a signaling adaptor shared by most members of the Toll-like receptor (TLR) family. Despite encouraging results in the murine system, rEA failed to protect hamsters challenged with PTV. Our findings suggest that hamsters may lack functional TLR11, which has recently been shown to recognize a profilin-like protein homologous to rEA from the protozoan Toxoplasma gondii. Further investigation into the immunostimulatory capacity of rEA in other mammalian systems is necessary.
Rift Valley fever virus (RVFV) is a significant pathogen of humans and domesticated ungulates. Recent disease outbreaks outside of sub-Saharan Africa (6-8) suggest that RVFV can be readily introduced and cause significant disease in other areas where susceptible hosts and its arthropod vector, the mosquito, are plentiful. Due to the relative ease by which it can be propagated and aerosolized, weaponization and intentional release are major public health concerns. To this end, RVFV has been classified as a category A pathogen by the National Institute of Allergy and Infectious Diseases (4), and handling requires maximum-level containment facilities that are not readily available to most researchers. Punta Toro virus (PTV) is a closely related, less biohazardous phlebovirus that produces in mice and hamsters a fatal hepatic disease similar to that caused by RVFV (9, 15). The PTV mouse disease model has facilitated the discovery of antivirals that are active against more biohazardous phleboviruses, such as RVFV and Sandfly fever viruses, that may be relevant to the treatment of human disease (20).
In order to explain the significant paucity of the number of small intestinal cancers in all species compared to the number of large intestinal cancers, Rosenberg et al. have proposed the existence of a protective factor against cancer in the small intestine (19). A search for this factor led to the isolation of a protein that acts as an immunomodulator in vitro and in vivo. This protein was isolated from bovine intestinal tissue infected with the endemic pathogenic protozoan of the Eimeria genus (Apicomplexa phylum). The Eimeria antigen (EA) protein is homologous to a protein of unknown function isolated from the avian protozoan Eimeria acervalina (13) and profilin-like proteins from other members of the Apicomplexa phylum (27).
Dendritic cells (DCs) are involved in the regulation of both the innate and the adaptive immune responses and are potent antigen-presenting cells (5). DCs have evolved innate programs that coordinate the release of immunoregulatory cytokines and chemokines, which activate and direct natural killer cells and other lymphocytes. In vitro studies of recombinant EA (rEA) have shown that it modulates the immune system by activating DCs to release interleukin-12 (IL-12), IL-6, and tumor necrosis factor alpha (19). In addition, gamma interferon (IFN-γ) and monocyte chemoattractant protein type 1 are also detected systemically after treatment of mice with rEA. This immunostimulatory activity likely contributes significantly to the enhanced resistance to cancer observed in vivo (19). Since the cell-mediated immunity essential to combating cancer is also critical for host defense against viruses, the ability of rEA to elicit protective immunity to PTV infection in several rodent phleboviral disease models was investigated.
MATERIALS AND METHODS
Animals.
Female C57BL/6 mice (weight, 12 to 14 g) and golden Syrian hamsters (weight, 90 to 100 g) were obtained from Charles River Laboratories (Wilmington, MA). All animals were held for a minimum of 48 h prior to use. Myeloid differentiation factor 88 (MyD88)-deficient mice were kindly provided by Shizuo Akira (Osaka University). Toll-like receptor 3 (TLR3)-deficient mice were derived at Yale University (2) and were provided by Richard Flavell. Both MyD88−/− and TLR3−/− mice were of the C57BL/6 mouse background. Animal procedures and breeding complied with the guidelines set forth by the USDA and the Utah State University Institutional Animal Care and Use Committee.
Virus.
The Adames strain of PTV was obtained from Dominique Pifat of the U.S. Army Medical Research Institute for Infectious Diseases, Ft. Detrick (Frederick, MD). Virus stock was prepared following four passages of the original virus stock through LLC-MK2 (rhesus monkey kidney) cells. PTV was inoculated into mice and hamsters by the subcutaneous route.
Test materials.
rEA was produced by previously described methods (19). In brief, cDNA was isolated from Eimeria tenella using appropriate primers and was used to transform an Escherichia coli bacterium for protein expression. Following protein induction, the bacteria were harvested, pelleted, and disrupted with a French press. The protein was isolated from the cellular debris by two ammonium sulfate precipitation steps, and three chromatographic steps (gradient hydrophobic interaction chromatography, gradient anion-exchange chromatography, and size-exclusion chromatography). Approximately 50 mg of pure protein was obtained from 1 liter of cell culture, with purity typically being >98%, as assayed by C8 reversed-phase high-pressure liquid chromatography and mass spectrometry. Purified rEA was formulated with 0.1% bovine serum albumin in phosphate-buffered saline (0.1% BSA-PBS). Preparations of rEA were tested for endotoxin by the Limulus lysate assay (Associates of Cape Cod, Inc., East Falmouth, MA). The highest dose of rEA (1 μg) used for treatment contained approximately 0.04 endotoxin units or the equivalent of 4 pg of contaminating lipopolysaccharide (LPS). Ribavirin was supplied by ICN Pharmaceuticals, Inc. (Costa Mesa, CA). Ampligen, poly(I:C12U), was provided by Hemispherx Biopharma (Philadelphia, PA). Sterile saline was used for dissolution and dilution of ribavirin and poly(I:C12U). All materials were administered by the intraperitoneal (i.p.) route.
Virus challenge studies.
Groups of 15 to 21 mice or hamsters (25 to 31 for the placebo group) were treated with rEA at various doses and on various schedules, starting before or after subcutaneous inoculation with 2 × 104 50% cell culture infectious doses (CCID50) of PTV for mouse challenges and 20 CCID50 for hamsters. Ribavirin was administered twice a day for 5 to 6 days, with treatment starting 4 h before virus inoculation. Five animals from each group (up to 10 animals for the placebo group) were killed on day 3 of infection; and their livers were scored on a scale of 0 to 4 for hepatic icterus, with 0 being normal and 4 being maximal yellow coloration. Serum was collected for assay of alanine aminotransferase (ALT) activity, and virus titers were determined for both liver and serum samples as described below. The remaining animals in each group were observed for 21 days. For comparison, three sham-infected animals were included as healthy controls in order to establish baselines for all parameters tested. To assess the potential toxicity associated with the test material, three uninfected animals for each dose tested were evaluated for normal weight gain and appearance.
Assessment of liver and serum virus loads.
Virus titers were determined by using an infectious cell culture assay, as described previously (21). Briefly, specific volumes of liver homogenate or serum were serially diluted and added to triplicate wells of LLC-MK2 cell monolayers in 96-well microplates. The viral cytopathic effect was determined 5 to 6 days after virus exposure, and the 50% endpoints were calculated as described previously (16).
Serum ALT determinations.
Serum ALT release serves as an indicator of liver damage and malfunction. ALT activity was measured by a kinetic assay by using the ALT (serum glutamic pyruvic transaminase) reagent set from Pointe Scientific, Inc. (Lincoln Park, MI). The reagent volumes were modified for use with 96-well microplates following the manufacturer's recommendations.
Cytokine profiling.
Groups of mice were treated as indicated with various dose amounts of rEA or vehicle, and serum was collected at the indicated times. Analysis of systemic IFN-γ and IL-12 levels following treatment was done using standard enzyme-linked immunosorbent assay (ELISA) reagents from eBioscience (San Diego, CA). Measurement of IFN-α and IFN-β production was performed using ELISA kits from R&D Systems (Minneapolis, MN). For experiments with MyD88−/−, MyD88+/−, MyD88+/+ (C57BL/6), and TLR3−/− mice, 6- to 8-week-old animals were used and IFN-γ release was assessed using a high-sensitivity ELISA kit from eBioscience.
Statistical analysis.
Fisher's exact test (two tailed) was used to evaluate increases in total survivors. The log-rank test was used for comprehensive survival analysis using JMP statistical software (SAS, Cary, NC). The Mann-Whitney test (two tailed) was performed to analyze the differences in the mean numbers of days to death, virus titers, and serum ALT levels. In cases in which the virus titers were below the 2.8-log10 limit of detection, a value of 2.8 was assigned for the purpose of statistical analysis. Wilcoxon ranked-sum analysis was used to compare mean liver scores.
RESULTS
Protection against PTV through prophylactic and therapeutic rEA treatment.
In the initial evaluation of rEA for anti-PTV activity, a two-dose schedule was used, as it was thought that it would provide the best protection. Doses of 0.1 or 1 μg were given beginning 4 h prior to PTV challenge, with a follow-up treatment given at 48 h postinfection. As shown in Table 1, both rEA treatments protected 100% of the mice and the 1-μg dose significantly reduced the hepatic icterus commonly seen with PTV infection. No overt toxicity was evident, as uninfected animals in a parallel study appeared to be healthy and gained weight through the course of treatment (data not shown). The ability of rEA to reduce the liver and serum virus titers resulting from PTV infection was also examined. On average, a greater than 1-log reduction in liver virus load was observed with rEA treatments compared to the placebo-treated animals (Table 1). Liver virus was not detectable in the positive control ribavirin-treated group. In the case of systemic virus sampled from serum, rEA significantly reduced the viral burden by more than 2 logs (Table 1). Further, serum ALT levels, which serve to indicate liver disease when elevated, were found to be markedly reduced in the rEA-treated mice and near the levels seen in ribavirin-treated mice. Collectively, with the exception of the liver scores, there were no appreciable differences between the two dosages of rEA tested in their ability to reduce disease severity, as determined by the measurement of various parameters, or to protect animals from death due to PTV infection.
TABLE 1.
Effect of prophylactic two-dose rEA treatment of mice challenged with PTV
| Treatmenta | Dosage | No. of survivors/ total no. | Mean day of deathb ± SD | Log-rank probability > chi square | Disease parameterc
|
|||
|---|---|---|---|---|---|---|---|---|
| Mean virus titerd ± SD
|
Mean ALT levele ± SD | Mean liver scoref ± SD | ||||||
| Liver | Serum | |||||||
| rEA | 1 μg/day | 11/11g | <0.0001 | <3.0 ± 0.6 | <4.6 ± 1.2g | 123 ± 64g | 0.8 ± 0.7h | |
| 0.1 μg/day | 10/10g | <0.0001 | <3.1 ± 0.7 | <4.7 ± 1.4g | 89 ± 52g | 1.8 ± 1.0 | ||
| Ribavirin | 75 mg/kg/day | 10/10g | <0.0001 | <2.8h | <3.3 ± 1.2g | 39 ± 7g | 0.0 ± 0.0g | |
| 0.1% BSA-PBS | 2/21 | 5.3 ± 1.4 | <4.2 ± 1.4 | 6.8 ± 0.5 | 2,250 ± 1,313 | 1.9 ± 1.3 | ||
| Sham infected | 3/3 | <2.8 | <2.8 | 42 ± 11 | 0.0 ± 0.0 | |||
rEA treatment was given i.p. 4 h before virus challenge and 48 h after virus challenge. Ribavirin was given i.p. twice per day for 5 days beginning 4 h before virus challenge.
Mean day of death for mice dying prior to day 21.
Determined on day 3 of infection; 10 mice per group.
Data represent the log10 CCID50/g of liver or ml of serum. The assay detection limit was 2.8 log10 CCID50/g or ml; a value of <2.8 was assigned for samples presenting with no detectable virus.
ALT levels were measured in international units per liter.
Scores ranged from 0 (normal liver) to 4 (maximal discoloration).
P < 0.001 compared to the 0.1% BSA-PBS placebo-treated controls.
P < 0.05 compared to the 0.1% BSA-PBS placebo-treated controls.
Having had success in the initial trial, in which mice were treated with rEA prior to infectious challenge, a second experiment investigating therapeutic use was performed. In that study, rEA was given as a single dose 24 h after virus challenge. Several log dilutions were tested in an attempt to determine the limits of protection. Remarkably, as shown in Table 2, all doses down to 1 ng examined protected 100% of the mice from an inoculum of PTV consisting of an 85% lethal dose. Analysis of the liver virus burden on day 3 of the infection indicated that only the highest doses were able to slightly reduce the virus titers at the time assayed. Interestingly, dose-responsiveness was not evident with liver scores as hepatic icterus was reduced by 17 to 43% across all treatments (Table 2). Further evaluation of liver disease, as determined by measurement of ALT levels, indicated that treatment with a rEA dose range of 1 to 0.01 μg produced highly significant reductions in ALT levels (>94% compared to the placebo group), and even the 0.001-μg dose was effective, but to a lesser degree. As revealed in Table 2, serum virus titers were significantly decreased with all doses tested, with the two highest doses producing the greatest reductions. The data indicate that although 100% protection was observed with all treatment doses evaluated, the higher doses were more effective at reducing disease severity, as determined by measurement of various parameters associated with PTV infection.
TABLE 2.
Dose effect of single-dose therapeutic rEA treatment on mice challenged with PTV
| Treatmenta | Dosage | No. of survivors/ total no. | Mean day of deathb ± SD | Log-rank probability > chi square | Disease parameterc
|
|||
|---|---|---|---|---|---|---|---|---|
| Mean virus titerd ± SD
|
Mean ALT levele ± SD | Mean liver scoref ± SD | ||||||
| Liver | Serum | |||||||
| rEA | 1 μg | 11/11g | <0.0001 | <3.1 ± 0.4 | <4.0 ± 1.1g | 57 ± 59g | 2.6 ± 0.2 | |
| 0.1 μg | 11/11g | <0.0001 | <3.2 ± 0.7 | <3.6 ± 1.3h | 139 ± 95g | 2.7 ± 0.3 | ||
| 0.01 μg | 11/11g | <0.0001 | 3.6 ± 0.1 | 5.0 ± 0.7g | 125 ± 159g | 2.0 ± 0.6 | ||
| 0.001 μg | 11/11g | <0.0001 | 3.6 ± 0.2 | 5.7 ± 0.5h | 914 ± 959 | 2.9 ± 0.5 | ||
| Ribavirin | 75 mg/kg/day | 11/11g | <0.0001 | <2.8h | <2.8g | 2 ± 3g | 1.2 ± 0.4g | |
| 0.1% BSA-PBS | 3/20 | 5.2 ± 0.8 | <3.7 ± 0.6 | 6.7 ± 0.6 | 2,568 ± 1,519 | 3.5 ± 0.6 | ||
| Sham infected | 3/3 | <2.8 | <2.8 | 42 ± 11 | 0.0 ± 0.0 | |||
Single-dose rEA treatment was administered i.p. 24 h after virus challenge. Ribavirin was given i.p. twice per day for 5 days beginning 4 h before virus challenge.
Mean day of death of mice dying prior to day 21.
Determined on day 3 of infection; 5 mice per group (10 mice in the placebo group).
Data represent the log10 cell culture CCID50/g of liver or ml of serum. The assay detection limit was 2.8 log10 CCID50/g or ml; a value of <2.8 was assigned for samples presenting with no detectable virus.
ALT levels were measured in international units per liter.
Scores ranged from 0 (normal liver) to 4 (maximal discoloration).
P < 0.001 compared to the 0.1% BSA-PBS placebo-treated controls.
P < 0.05 compared to the 0.1% BSA-PBS placebo-treated controls..
To determine how late after the infectious challenge rEA could be administered and still maintain adequate levels of protection against PTV, an experiment in which the onset of treatment was delayed past 24 h was performed. As seen in Table 2, the 24-h treatment with 0.1 μg of rEA was highly effective at protecting all infected mice and limiting disease manifestations (Table 3). When treatment was delayed to 36 h, 70% of the animals survived the infection and a significant decrease in systemic viral load and hepatic icterus resulted. Despite the latter finding, serum ALT levels were elevated and comparable to those seen in the placebo-treated animals. Treatments administered 48 and 60 h postinfection failed to provide statistically significant levels of protection against mortality, although in the group treated at 48 h postinfection, it was notable that 50% of the PTV-challenged mice were protected (Table 3). Furthermore, no appreciable reduction in the values of any of the associated parameters of disease measured was noted for these treatment groups. Thus, in the PTV mouse infection model, rEA needs to be given within 24 h of challenge for optimal efficacy, with more limited protection seen from 36 to 48 h.
TABLE 3.
Effect of delayed rEA therapy on mice challenged with PTV
| Treatmenta | Time of initiation of treatment (h) | No. of survivors/ total no. | Mean day of deathb ± SD | Log-rank probability > chi square | Disease parameterc
|
|||
|---|---|---|---|---|---|---|---|---|
| Mean virus titerd ± SD
|
Mean ALT levele ± SD | Mean liver scoref ± SD | ||||||
| Liver | Serum | |||||||
| rEA | 24 | 10/10g | 0.0001 | <3.1 ± 0.8 | <2.8g | 80 ± 12g | 2.2 ± 0.3h | |
| 36 | 7/10i | 4.7 ± 0.6 | 0.0113 | <3.4 ± 0.9 | <3.8 ± 1.4i | 2,511 ± 1,884 | 2.4 ± 0.9i | |
| 48 | 5/10 | 4.2 ± 1.1 | 0.2046 | <3.3 ± 0.1 | 6.4 ± 1.1 | 2,590 ± 1,393 | 3.8 ± 0.4 | |
| 60 | 2/10 | 4.0 ± 1.3 | 0.4789 | <3.3 ± 0.1 | 6.6 ± 0.7 | 3,269 ± 1,716 | 3.7 ± 0.3 | |
| Ribavirin | −4 | 10/10g | 0.0001 | <2.8i | <2.8g | 13 ± 9g | 0.0 ± 0.0g | |
| 0.1% BSA-PBS | 24 | 4/20 | 4.8 ± 1.5 | <3.2 ± 0.9 | 6.2 ± 0.6 | 2,461 ± 1,677 | 3.5 ± 0.8 | |
| Sham infected | 3/3 | <2.8 | <2.8 | 11 ± 13 | 0.0 ± 0.0 | |||
Single-dose 0.1-μg rEA treatment was administered i.p. at the indicated times after virus challenge. Ribavirin (75 mg/kg/day) was given i.p. twice per day for 5 days.
Mean day of death for mice dying prior to day 21.
Determined on day 3 of infection; 5 mice per group (10 mice in the placebo group).
Data represent the log10 CCID50/g of liver or ml of serum. The assay detection limit was 2.8 log10 CCID50/g or ml; a value of <2.8 was assigned for samples presenting with no detectable virus.
ALT levels were measured in international units per liter.
Score of 0 (normal liver) to 4 (maximal discoloration).
P < 0.001 compared to the 0.1% BSA-PBS placebo-treated controls.
P < 0.01 compared to the 0.1% BSA-PBS placebo-treated controls.
P < 0.05 compared to the 0.1% BSA-PBS placebo-treated controls.
Induction of systemic IL-12 and IFN-γ following rEA treatment.
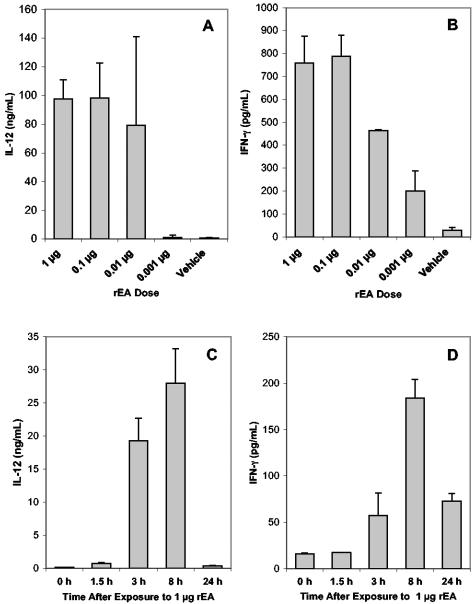
Exposure to 0.01 μg rEA has recently been reported to elicit copious amounts of IL-12 and IFN-γ in adult BALB/c mice within 6 h of treatment (19). In light of our findings that the lower doses of rEA had lost some of their ability to reduce the values for the disease parameters measured, the induction of IL-12 and IFN-γ in the weanling C57BL/6 mice used in the PTV disease model was examined in an attempt to correlate cytokine production with disease severity. As demonstrated in Fig. 1A, the highest doses of rEA were all very effective in eliciting IL-12 release at 6 h; however, a dramatic decrease was observed with the 0.001-μg dose. In the case of IFN-γ, significant reductions in levels in serum were seen with the 0.01- and 0.001-μg doses (Fig. 1B), which may explain the reduced capacity of these treatments to limit disease manifestations (Table 2). Appreciable levels of systemic IFN-α and IFN-β were not induced by any of the rEA doses tested (data not shown). The response kinetics following treatment of uninfected animals with 1 μg of rEA were also evaluated. IL-12 levels increased dramatically after the 1.5-h sampling time, with nearly equivalent levels seen at the 3- and 8-h time points (Fig. 1C). As revealed in Fig. 1D, IFN-γ was present at modest levels in the serum at 3 h, with the highest levels observed at the 8-h sampling time. As with the samples obtained at 6 h, neither IFN-α nor IFN-β was found to be elicited by 1 μg of rEA at the 1.5-, 3-, 8-, and 24-h sampling times evaluated (data not shown).
FIG. 1.
IL-12 and IFN-γ induction in uninfected weanling mice following rEA exposure. Three- to 4-week old mice were injected i.p. with 1, 0.1, 0.01, or 0.001 μg of rEA; and systemic IL-12 (A and C) and IFN-γ (B and D) levels were determined in serum samples collected 6 h postexposure (A and B) or at the indicated times (C and D). The data represent the means and standard deviations for three animals per group.
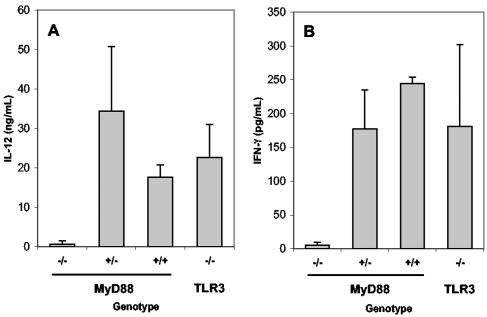
IL-12 and IFN-γ induction by rEA requires MyD88.
Many known immunomodulatory agents are recognized by members of the TLR family (25). Thus, we investigated the capacity of rEA to elicit IL-12 and IFN-γ in mice lacking TLR3 or the MyD88 adaptor, which is required by the majority of TLRs (with the exception of TLR3) for signaling (1). As shown in Fig. 2, TLR3-deficient mice produced significant levels of IL-12 and IFN-γ following exposure to rEA. In contrast, MyD88−/− mice failed to mount a response to rEA, as only basal levels of cytokines were observed, whereas heterozygote and wild-type littermates produced normal levels of IL-12 and IFN-γ. These data suggest that MyD88 is crucial to the immunostimulatory activity induced by rEA in mice.
FIG. 2.
IL-12 and IFN-γ induction requires the TLR signaling pathway adaptor, MyD88. MyD88-deficient, TLR3-deficient, and wild-type mice (6 to 8 weeks of age) were injected i.p. with 1 μg of rEA, and the serum levels of IL-12 (A) and IFN-γ (B) were measured at 6 h postexposure. The data represent the means and standard deviations for groups of four to six animals from four separate experiments.
Treatment of PTV infection in hamsters with rEA.
PTV has previously been reported to induce in hamsters acute disease that is believed to more closely resemble that caused by RVFV (3, 9). Therefore, we also evaluated rEA in the hamster disease model, in light of the vigorous protection against highly lethal PTV infection induced in mice. Since complete protection at the level of survival was seen at the lowest dose tested in mice (Table 2), 1 μg of rEA was chosen as the top dosage for the hamster challenge. On a per-weight basis, this roughly amounted to the 0.1-μg dose given to mice, which was at a minimum 100 times the dose observed to provide complete protection of infected animals from mortality (Table 2). In contrast to the clear protective effects elicited by rEA in the mouse infection model, no significant effect was seen in the hamster system when times to death and rates of survival were compared by the several statistical methods used (Table 4). In fact, it appeared that rEA treatment may worsen the prognosis, as in all cases the hamsters in the placebo group survived 1 to 2 days longer than those treated with rEA. Consistent with the observed accelerated disease progression, dramatically elevated systemic and liver virus titers were seen only in rEA-treated animals on day 3 of the infection (Table 4). The lack of efficacy in the hamster model was not likely due to obvious toxicity, since all doses of rEA evaluated were well tolerated by uninfected animals (data not shown). Essentially no liver discoloration or elevation in serum ALT levels was noted in this study. This was likely due to the time at which the samples were collected (day 3), which was apparently too early in the course of disease but which was chosen since mortality in a small percentage of animals usually occurs by day 4. All challenged hamsters treated with ribavirin and poly(I:C12U) survived the infection and, with the exception of one animal which presented with liver virus, had undetectable levels of virus (Table 4). Poly(I:C12U), which is a mismatched double-stranded RNA with previously documented immunotherapeutic activity against PTV infection in mice (22), was included as an additional control to demonstrate the responsiveness of the hamster model to immunostimulatory material.
TABLE 4.
Dose effect of single-dose prophylactic rEA treatment on hamsters challenged with PTV
| Treatmenta | Dosage | No. of survivors/ total no. | Mean day of deathb ± SD | Log-rank probability > chi square | Mean virus titerc ± SD
|
|
|---|---|---|---|---|---|---|
| Liver | Serum | |||||
| rEA | 1 μg | 5/11 | 6.7 ± 2.7 | 0.7929 | 6.6 ± 2.2d | <3.9 ± 2.6 |
| 0.1 μg | 2/11 | 7.3 ± 2.1 | 0.0675 | <5.0 ± 2.9 | <4.7 ± 3.0 | |
| 0.01 μg | 4/11 | 6.0 ± 1.5 | 0.3310 | <5.9 ± 2.7e | <4.1 ± 3.0 | |
| poly(I:C12U) | 100 μg | 11/11d | 0.0048 | <3.4 ± 1.3 | <2.8 | |
| Ribavirin | 75 mg/kg/day | 11/11d | 0.0048 | <2.8 | <2.8 | |
| 0.1% BSA-PBS | 10/21 | 8.3 ± 3.8 | <2.8 | <2.8 | ||
| Sham infected | 3/3 | <2.8 | <2.8 | |||
Single-dose rEA and poly(I:C12U) treatment was administered i.p. at 4 h before virus challenge. Ribavirin was given i.p. twice per day for 6 days beginning 4 h before virus challenge.
Mean day of death of hamsters dying prior to day 21.
Determined on day 3 of infection; five hamsters per group. Data represent the log10 CCID50/g of liver or ml of serum. The assay detection limit was 2.8 log10 CCID50/g or ml; a value of <2.8 was assigned for samples presenting with no detectable virus.
P < 0.01 compared to the 0.1% BSA-PBS placebo-treated controls.
P < 0.05 compared to the 0.1% BSA-PBS placebo-treated controls.
DISCUSSION
In the mouse PTV infection model, prophylactic and therapeutic interventions with nanogram amounts of rEA were found to be highly effective. Although the dose at which the viral burden was reduced and the extent of liver disease waned was determined to be in the 0.1-μg range, treatment with 100-fold less rEA still provided complete protection in the context of survival. Potentially, picogram quantities of rEA may provide adequate protection against PTV-associated mortality. It is unlikely that the extremely low-levels of E. coli LPS present in the rEA preparations tested contributed to the induced protective effect, since treatment with a 50-fold excess (200 pg) of highly purified LPS provided no protection against PTV infection and rEA was equally effective in TLR4-deficient, C3H/HeJ mice (data not shown). Therapy with rEA was successful, as long as it was administered within 24 h of viral challenge, with more limited efficacy seen out to 36 h. Treatments postponed for 48 h or more failed to reduce the disease and death associated with PTV infection. Considering the acute nature of PTV infection in mice, in which the mean time of death for most animals is 4 to 5 days, significant protection out to 36 h is considered remarkable. Moreover, like many infectious diseases, PTV disease is greatly exacerbated by handling stress. Thus, successful therapy becomes more difficult for treatments scheduled at later times during the course of infection. While ribavirin was more effective than the single-dose rEA treatment at reducing liver disease manifestations, it was administered twice per day for 5 days and was generally associated with noticeable weight loss during treatment.
Several of us have previously shown that rEA is a potent inducer of IL-12, IFN-γ, and other proinflammatory cytokines in BALB/c mice (19). Since mice of a different strain and age were required for the PTV disease model and variation may exist between the lots of rEA preparations used previously, additional in vivo cytokine analyses were performed with the rEA used in the challenge studies. Our serum IL-12 and IFN-γ profiles for the 10-ng dose obtained with weanling C57BL/6 mice were comparable to the levels in plasma found by Rosenberg and colleagues (19). Consistent with the increased viral loads present at the 1- and 10-ng doses of rEA, lower levels of IFN-γ were seen with these doses and the level of IL-12 production declined precipitously with the 1-ng dose. IL-12 is a Th1-promoting cytokine primarily produced by DCs and phagocytes. It stimulates NK cell function and T-cell development, including the synthesis and release of IFN-γ, which can further enhance IL-12 production and which plays a vital role in combating viral infections (10, 18). Our data indicate that IL-12 levels rose abruptly several hours following exposure to rEA and likely peaked somewhere between the 3- and 8-h time points. On the other hand, IFN-γ levels began to rise at 3 h, with an apparent peak in serum levels occurring at about 8 h after rEA exposure. In contrast to the IL-12 levels, the IFN-γ levels remained elevated at the 24-h sampling time. Considering that the effect of IL-12 is as an inducer of IFN-γ, it was not surprising to see IL-12 release preceding that of IFN-γ. It would be interesting to further ascertain the effects of rEA, perhaps by study of the material's efficacy in IL-12- and IFN-γ-knockout mice or by neutralization of these cytokines with antibodies to confirm their involvement. Caution must be used when interpreting the results of such studies, since a lack of efficacy may be due in part to the absence of rEA-independent, PTV-induced IL-12 and IFN-γ antiviral responses. Indeed, we have data indicating that IL-12 and IFN-γ are induced following infectious challenge with PTV and likely play an important role in host defense against PTV infection.
Since type I IFNs are important factors in establishing host resistance to viral infection, the ability of rEA to elicit IFN-α and/or IFN-β was also investigated. At the rEA doses and sampling times tested, we did not find any increase in IFN-α or IFN-β levels following treatment. It is conceivable that during active infection, rEA may enhance the type I IFN response, which has been shown to be crucial to protective immunity against PTV (15, 22). However, unlike most immunomodulators that have been effective against PTV, it appears that rEA triggers a different type of response that leads to robust protection without the direct induction of type I IFNs.
TLRs are crucial to innate resistance and adaptive immunity to infectious agents (12, 23). A number of pathogen-associated molecules are known to stimulate IL-12 through interactions with TLRs (24). We initially screened rEA for activity against a panel of human TLRs (TLRs 2, 3, 4, 5, 7, 8, and 9), which failed to produce positive results (data not shown). The potential involvement of a TLR family member was further explored by using mice lacking the MyD88 adaptor required for most TLR signaling. Exposure of these animals to rEA failed to elicit IL-12 and IFN-γ, as seen with mice having one or more functional copies of the gene. Thus, our findings suggest that, indeed, a member of the TLR family of receptors is involved in immunomodulation by rEA. In support of our data, Yarovinsky and Sher recently identified TLR11 as the host receptor that recognizes profilin protein from Toxoplasma gondii and other apicomplexan protozoan profilins (27). In their cell-based assay system, rEA, which has limited homology to other profilins, also triggers TLR11 activation (F. Yarovinsky and A. Sher, personal communication), strongly suggesting that this receptor is mediating the induction of protective immunity to PTV challenge in mice.
The evaluation of rEA for its antiphleboviral activity in hamsters is the first reported antiviral study by use of this PTV model first described over a decade ago (3). In comparison to the mouse model, the hamster model may provide a better reflection of human disease (3, 9) and is much more susceptible to terminal PTV infection. This was most prominently reflected by the age-independent susceptibility of hamsters, whereas most strains of mice become refractory to the virus by 6 weeks of age (15). Also remarkable is that, in comparison to mice on a per-weight basis, ∼1,000-fold less virus is needed to induce productive disease and mortality in hamsters. As seen with the mouse model, ribavirin and poly(I:C12U) were both effective for the treatment of PTV infection. In contrast to rEA, poly(I:C12U) induces type I interferon in both mice and hamsters (11, 22). Approximately 10 times more poly(I:C12U) was needed for adequate survival protection against PTV infection in hamsters than in mice. It appears that PTV infection in hamsters is more aggressive and, consequently, more difficult to treat, thereby requiring more poly(I:C12U). Alternatively, poly(I:C12U) may be less reactive in hamsters than in mice due to species differences. Also noteworthy was the lack of liver disease, as measured by discoloration and serum ALT levels. While mortality in both models generally starts by day 4 of infection, the time of death for PTV-infected weanling mice is far less variable than that seen for hamsters. This was reflected by the mean time of death for placebo-treated mice, which was in the range of 5.1 ± 1.2 days, compared to that for hamsters, which was 8.3 ± 3.8 days. As a result, at the time when samples were collected (day 3 of infection), hamsters were not far enough along in the infection to present with advanced liver disease, as described by Fisher and colleagues (9).
As predicted on the basis of the recent discovery identifying Toxoplasma gondii profilin as a TLR11 ligand (27), there is now evidence that the related Eimeria and all other apicomplexan protozoan profilins that have been examined are also recognized by TLR11 (26). To date, mice are the only known vertebrates to express a functional TLR11 (17). Additional investigations have uncovered the finding that mouse TLR11 has >70% identity with rat TLR11; however, homologs could not be found in the other genomes (chimp, dog, cat, fugu, and frog genomes) that have been explored (14). Thus, it was of great interest to evaluate rEA in the hamster system since this would provide insight into whether a functional TLR11 exists in this species. We found that rEA, which is markedly efficacious in mice, failed to improve the survival outcomes or to protect hamsters from PTV disease. Unfortunately, due to the lack of reagents available for hamster immunological studies, we could not investigate IL-12 or IFN-γ induction following rEA treatment. Nevertheless, our findings suggest that hamsters may not express functional TLR11 or that the receptor may not recognize rEA, as is the case for mouse TLR11.
With regard to the application of these data to humans, initial results from ongoing phase I clinical trials with cancer patients have shown a modest IL-12 response to repeated administration of rEA. In addition, other anecdotal evidence suggests that some beneficial therapeutic effect can be achieved with rEA (B. Rosenberg et al., unpublished data). Preliminary studies in vitro have demonstrated that rEA can significantly enhance IFN-γ release from human peripheral blood mononuclear cells, suggesting that another mechanism of immune activation may be involved, since a functional homolog to mouse TLR11 does not appear to exist for humans (17, 28). Further studies are under way to determine the applicability and mechanism of action of rEA in humans and other species.
Acknowledgments
We thank Heather Greenstone for critical review of the manuscript. We also thank Kevin Isakson, Andrew Sanders, and Matthew Heiner for technical support.
This work was supported by contract NO1-AI-15435 from the Virology Branch, National Institute of Allergy and Infectious Diseases, National Institutes of Health.
REFERENCES
- 1.Akira, S., and K. Takeda. 2004. Toll-like receptor signalling. Nat. Rev. Immunol. 4:499-511. [DOI] [PubMed] [Google Scholar]
- 2.Alexopoulou, L., A. C. Holt, R. Medzhitov, and R. A. Flavell. 2001. Recognition of double-stranded RNA and activation of NF-kappaB by Toll-like receptor 3. Nature 413:732-738. [DOI] [PubMed] [Google Scholar]
- 3.Anderson, G. W., Jr., M. V. Slayter, W. Hall, and C. J. Peters. 1990. Pathogenesis of a phleboviral infection (Punta Toro virus) in golden Syrian hamsters. Arch. Virol. 114:203-212. [DOI] [PubMed] [Google Scholar]
- 4.Anonymous. 2002. The counter-bioterrorism research agenda of the National Institute of Allergy and Infectious Diseases (NIAID) for CDC category A agents. National Institute of Allergy and Infectious Diseases, Bethesda, Md.
- 5.Banchereau, J., F. Briere, C. Caux, J. Davoust, S. Lebecque, Y. J. Liu, B. Pulendran, and K. Palucka. 2000. Immunobiology of dendritic cells. Annu. Rev. Immunol. 18:767-811. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. 2000. Outbreak of Rift Valley fever—Saudi Arabia, August-October, 2000. Morb. Mortal. Wkly. Rep. 49:905-908. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. 2000. Outbreak of Rift Valley fever—Yemen, August-October 2000. Morb. Mortal. Wkly. Rep. 49:1065-1066. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 1994. Rift Valley fever—Egypt, 1993. Morb. Mortal. Wkly. Rep. 43:693, 699-700. [PubMed] [Google Scholar]
- 9.Fisher, A. F., R. B. Tesh, J. Tonry, H. Guzman, D. Liu, and S. Y. Xiao. 2003. Induction of severe disease in hamsters by two sandfly fever group viruses, Punta Toro and Gabek Forest (Phlebovirus, Bunyaviridae), similar to that caused by Rift Valley fever virus. Am. J. Trop. Med. Hyg. 69:269-276. [PubMed] [Google Scholar]
- 10.Goodbourn, S., L. Didcock, and R. E. Randall. 2000. Interferons: cell signalling, immune modulation, antiviral response and virus countermeasures. J. Gen. Virol. 81:2341-2364. [DOI] [PubMed] [Google Scholar]
- 11.Gowen, B. B., D. L. Barnard, D. F. Smee, M. H. Wong, A. M. Pace, K. H. Jung, S. G. Winslow, K. W. Bailey, L. M. Blatt, and R. W. Sidwell. 2005. Interferon alfacon-1 protects hamsters from lethal pichinde virus infection. Antimicrob. Agents Chemother. 49:2378-2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoebe, K., E. Janssen, and B. Beutler. 2004. The interface between innate and adaptive immunity. Nat. Immunol. 5:971-974. [DOI] [PubMed] [Google Scholar]
- 13.Laurent, F., C. Bourdieu, M. Kazanji, P. Yvore, and P. Pery. 1994. The immunodominant Eimeria acervulina sporozoite antigen previously described as p160/p240 is a 19-kilodalton antigen present in several Eimeria species. Mol. Biochem. Parasitol. 63:79-86. [DOI] [PubMed] [Google Scholar]
- 14.Lauw, F. N., D. R. Caffrey, and D. T. Golenbock. 2005. Of mice and man: TLR11 (finally) finds profilin. Trends Immunol. 26:509-511. [DOI] [PubMed] [Google Scholar]
- 15.Pifat, D. Y., and J. F. Smith. 1987. Punta Toro virus infection of C57BL/6J mice: a model for phlebovirus-induced disease. Microb. Pathog. 3:409-422. [DOI] [PubMed] [Google Scholar]
- 16.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 17.Roach, J. C., G. Glusman, L. Rowen, A. Kaur, M. K. Purcell, K. D. Smith, L. E. Hood, and A. Aderem. 2005. The evolution of vertebrate Toll-like receptors. Proc. Natl. Acad. Sci. USA 102:9577-9582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romani, L., P. Puccetti, and F. Bistoni. 1997. Interleukin-12 in infectious diseases. Clin. Microbiol. Rev. 10:611-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenberg, B., D. A. Juckett, C. F. Aylsworth, N. V. Dimitrov, S. C. Ho, J. W. Judge, S. Kessel, J. Quensen, K. P. Wong, I. Zlatkin, and T. Zlatkin. 2005. Protein from intestinal Eimeria protozoan stimulates IL-12 release from dendritic cells, exhibits antitumor properties in vivo and is correlated with low intestinal tumorigenicity. Int. J. Cancer 114:756-765. [DOI] [PubMed] [Google Scholar]
- 20.Sidwell, R. W., J. H. Huffman, D. L. Barnard, D. F. Smee, R. P. Warren, M. A. Chirigos, M. Kende, and J. Huggins. 1994. Antiviral and immunomodulating inhibitors of experimentally-induced Punta Toro virus infections. Antivir. Res. 25:105-122. [DOI] [PubMed] [Google Scholar]
- 21.Sidwell, R. W., J. H. Huffman, B. B. Barnett, and D. Y. Pifat. 1988. In vitro and in vivo phlebovirus inhibition by ribavirin. Antimicrob. Agents Chemother. 32:331-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sidwell, R. W., J. H. Huffman, D. F. Smee, J. Gilbert, A. Gessaman, A. Pease, R. P. Warren, J. Huggins, and M. Kende. 1992. Potential role of immunomodulators for treatment of phlebovirus infections of animals. Ann. N. Y. Acad. Sci. 653:344-355. [DOI] [PubMed] [Google Scholar]
- 23.Takeda, K., T. Kaisho, and S. Akira. 2003. Toll-like receptors. Annu. Rev. Immunol. 21:335-376. [DOI] [PubMed] [Google Scholar]
- 24.Trinchieri, G. 2003. Interleukin-12 and the regulation of innate resistance and adaptive immunity. Nat. Rev. Immunol. 3:133-146. [DOI] [PubMed] [Google Scholar]
- 25.Ulevitch, R. J. 2004. Therapeutics targeting the innate immune system. Nat. Rev. Immunol. 4:512-520. [DOI] [PubMed] [Google Scholar]
- 26.Yarovinsky, F., and A. Sher. 2006. Toll-like receptor recognition of Toxoplasma gondii. Int. J. Parasitol. 36:255-259. [DOI] [PubMed] [Google Scholar]
- 27.Yarovinsky, F., D. Zhang, J. F. Andersen, G. L. Bannenberg, C. N. Serhan, M. S. Hayden, S. Hieny, F. S. Sutterwala, R. A. Flavell, S. Ghosh, and A. Sher. 2005. TLR11 activation of dendritic cells by a protozoan profilin-like protein. Science 308:1626-1629. [DOI] [PubMed] [Google Scholar]
- 28.Zhang, D., G. Zhang, M. S. Hayden, M. B. Greenblatt, C. Bussey, R. A. Flavell, and S. Ghosh. 2004. A toll-like receptor that prevents infection by uropathogenic bacteria. Science 303:1522-1526. [DOI] [PubMed] [Google Scholar]