Abstract
We have characterized a new clinical strain of Trichophyton rubrum highly resistant to terbinafine but exhibiting normal susceptibility to drugs with other mechanisms of action. Resistance to terbinafine in this strain is caused by a missense mutation in the squalene epoxidase gene leading to the amino acid substitution F397L.
Terbinafine, whose target is squalene epoxidase (SE), part of the ergosterol biosynthesis pathway, is used extensively in the treatment of dermatophytosis, a common infection caused by dermatophytes. Nevertheless, the occurrence of terbinafine-resistant clinical isolates is rare, and only one case has been documented and thoroughly investigated (7, 14, 17); the resistance mechanism was identified as a single amino acid substitution in SE. Except for this one case, terbinafine failure in patients suffering from nail infections due to Trichophyton rubrum has been shown not to be related to high MICs or resistance development during therapy (1, 9). The same conclusion was drawn by Hofbauer et al. (11) in a veterinary study. In vitro, the frequency of spontaneous resistance of T. rubrum to terbinafine is low and it is also difficult to induce resistance (16). Nevertheless, dermatophytes with abnormally low susceptibility to terbinafine do exist (8, 10, 18). Here, we have identified such a clinical strain (NFI5166), originally isolated by C. Burri (Chur, Switzerland), and characterized it at a biological, biochemical, and molecular level.
NFI5166 was tested in comparison with NFI1895, a well-characterized internal reference clinical strain from the Novartis Fungal Index (NFI) collection. MICs against T. rubrum were determined in broth macrodilution assays based on the CLSI (formerly NCCLS) M38-A protocol (15) as described previously (11). NFI5166 was strongly resistant to terbinafine, with a drug MIC of 64 μg/ml compared to <1 ng/ml for NFI1895 (Table 1). This drug MIC was even higher than those for the previously analyzed terbinafine-resistant strains NFI5146 to NFI5150 (4 μg/ml) (14), which were isolated from a different patient. NFI5166 was also strongly (>100-fold) cross-resistant to other SE inhibitors tested (naftifine, butenafine, and tolnaftate). Susceptibility to fluconazole and griseofulvin was similar to that of the wild-type strain NFI1895. The MIC of itraconazole for NFI5166 was 64-fold higher than that for NFI1895 but was similar to those seen for other wild-type strains tested (data not shown). Systematic cross-resistance to SE inhibitors suggested a target-based mechanism of resistance. Preparation of microsomes and assay of SE activity were performed as previously described (4, 6, 7). NFI5166 SE-specific activity of 0.013 nmol/h/mg protein was about threefold lower than for strains NFI1895, NFI5146, and NFI5150 (7). The 50% inhibitory concentration of terbinafine was 1.3 μg/ml for SE from NFI5166 versus 0.006 μg/ml for the microsomal activity of NFI1895. These results reinforced the hypothesis that an alteration of SE was involved in the resistance phenotype of NFI5166.
TABLE 1.
MICs of several antifungals against T. rubrum NFI5166 and the reference strain NFI1895 determined using the broth macrodilution method
| Compound | Antifungal MIC (μg/ml)
|
|
|---|---|---|
| NFI5166 | NFI1895 | |
| Terbinafine | 64 | 0.0002 |
| Naftifine | 64 | 0.04 |
| Butenafine | 1 | 0.0005 |
| Tolnaftate | 0.25 | 0.0002 |
| Fluconazole | 8 | 4 |
| Itraconazole | 0.5 | 0.008 |
| Griseofulvin | 2 | 2 |
To further characterize the strain, NFI5166 SE was cloned and sequenced as described previously (17). The SE sequence from NFI5166 contained a missense substitution, 1189TTC→CTC, introducing the amino acid substitution F397L in the open reading frame. This position is very close to L393F, the previous substitution found in SE from NFI5146 and NFI5150 (17). Interestingly, we found the same amino acid substitution, F397L, in the SE gene from NFI5182-06, a laboratory strain previously isolated from a potato dextrose agar plate containing 0.06 μg/ml terbinafine inoculated with a high CFU of NFI5182 (ATCC 18759) (16). The MIC of terbinafine against NFI5182-06 was 4 μg/ml compared to 0.004 μg/ml for NFI5182. Overall, the susceptibility pattern of NFI5182-06 compared to that of wild-type NFI5182 (broth microdilution method [16]; data not shown) was similar to that of NFI5166, with resistance to SE inhibitors and normal susceptibility to antifungals with a different mode of action.
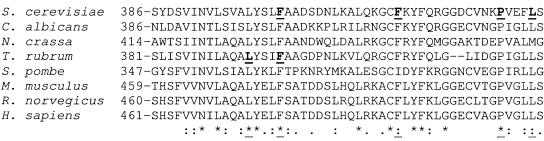
To further demonstrate that this amino acid substitution is at least partly responsible for the resistance phenotype of NFI5166 and NFI5182-06, we used the model Candida albicans SE cloned into the expression vector pYES2 and Saccharomyces cerevisiae as the recipient organism (17). The mutation F402L, corresponding to the alteration F397L identified in SE from NFI5166 (Fig. 1), was introduced into the C. albicans SE sequence (17) by use of a QuikChange site-directed mutagenesis kit (Stratagene). After transformation of S. cerevisiae INVSc1 and selection on medium lacking uracil, glucose was replaced by galactose to induce the expression of C. albicans SE (5). A microdilution assay using a 96-well plate (Greiner) (17) was used to test drug susceptibility. INVSc1 expressing CaSE-F402L was ≥16-fold less susceptible to terbinafine than the transformants expressing wild-type CaSE (Table 2).
FIG. 1.
Protein sequence alignment (ClustalW) (2) of fungal and mammalian SEs in the region in which several amino acid substitutions (wild-type residues are underlined), affecting the susceptibility of fungi to terbinafine, were found. Key: *, identical between sequences, :, conserved substitution; ·, semiconserved substitution; _, wild type.
TABLE 2.
MIC of terbinafine required to reach 90% growth inhibition of S. cerevisiae INVSc1, transformed with various CaSE constructs, in liquid RPMI 1640 medium
| Construct | Mutation | 90% MIC (μg/ml) |
|---|---|---|
| None | 8 | |
| pYES2 | 4-8 | |
| CaSE | None | 8 |
| CaSE | F402L | >128 |
The main features of NFI5166 are very similar to those of the previously reported set of resistant isolates from a single patient, NFI5146 to NFI5150, which can be considered a single strain (7, 14, 17). Both the new isolate, NFI5166, and the strain reported earlier, NFI5146 (the baseline isolate), are cross-resistant to all tested SE inhibitors, are normally susceptible to other antifungals with a different mode of action, have microsomal SE activity much less sensitive to terbinafine than wild-type strains, and contain single amino acid substitutions in their SE. However, the amino acid substitutions, F397L in NFI5166 versus L393F in NFI5146, differ between the strains although they are close together. This region may thus be involved in the high-affinity binding of terbinafine to SE, as demonstrated by the lower sensitivity of the enzymatic activity to terbinafine of the enzymes bearing these amino acid substitutions (7, 17). This hypothesis is also reinforced by the previous findings of Leber et al. (12), who identified four point mutations in the same domain of S. cerevisiae SE which could confer resistance to terbinafine, F402L, F420L, P430S, and F433S, corresponding to F397, F415, P423, and L426, respectively, in T. rubrum SE (Fig. 1).
So far our analyses have revealed that terbinafine resistance in T. rubrum is only connected to amino acid substitutions in SE. However, this does not preclude other resistance mechanisms. The occurrence of multiple antifungal resistance mechanisms within the same organism is well established (3, 13, 19, 20). Nevertheless, resistance to terbinafine in NFI5166 might be pleiotropic, since this strain is more resistant than NFI5182-06, which carries the same SE mutation.
In conclusion, alteration of the target of terbinafine in T. rubrum seems to be the predominant resistance mechanism in this organism. However, since the frequency of resistance of T. rubrum to terbinafine is very low, it appears unlikely that resistance to terbinafine therapy will become a significant clinical problem.
Nucleotide sequence accession number.
The complete sequence data for NFI5166 SE have been assigned GenBank accession number DQ060522.
REFERENCES
- 1.Bradley, M. C., S. Leidich, N. Isham, B. E. Elewski, and M. A. Ghannoum. 1999. Antifungal susceptibilities and genetic relatedness of serial Trichophyton rubrum isolates from patients with onychomycosis of the toenail. Mycoses 42:105-110. [PubMed] [Google Scholar]
- 2.Chenna, R., H. Sugawara, T. Koike, R. Lopez, T. J. Gibson, D. G. Higgins, and J. D. Thompson. 2003. Multiple sequence alignment with the Clustal series of programs. Nucleic Acids Res. 31:3497-5300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.da Silva Ferreira, M. E., J. L. Capellaro, E. dos Reis Marques, I. Malavazi, D. Perlin, S. Park, J. B. Anderson, A. L. Colombo, B. A. Arthington-Skaggs, M. H. Goldman, and G. H. Goldman. 2004. In vitro evolution of itraconazole resistance in Aspergillus fumigatus involves multiple mechanisms of resistance. Antimicrob. Agents Chemother. 48:4405-4413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Favre, B., and N. S. Ryder. 1996. Characterization of squalene epoxidase activity from the dermatophyte Trichophyton rubrum and its inhibition by terbinafine and other antimycotic agents. Antimicrob. Agents Chemother. 40:443-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Favre, B., and N. S. Ryder. 1997. Differential inhibition of fungal and mammalian squalene epoxidases by the benzylamine SDZ SBA 586 in comparison with the allylamine terbinafine. Arch. Biochem. Biophys. 340:265-269. [DOI] [PubMed] [Google Scholar]
- 6.Favre, B., and N. S. Ryder. 1997. Cloning and expression of squalene epoxidase from the pathogenic yeast Candida albicans. Gene 189:119-126. [DOI] [PubMed] [Google Scholar]
- 7.Favre, B., M. A. Ghannoum, and N. S. Ryder. 2004. Biochemical characterization of terbinafine-resistant Trichophyton rubrum isolates. Med. Mycol. 42:525-529. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez-Torres, B., H. Vazquez-Veiga, X. Llovo, M. Pereiro, Jr., and J. Guarro. 2000. In vitro susceptibility to itraconazole, clotrimazole, ketoconazole and terbinafine of 100 isolates of Trichophyton rubrum. Chemotherapy 46:390-394. [DOI] [PubMed] [Google Scholar]
- 9.Gupta, A. K., and Y. Kohli. 2003. Evaluation of in vitro resistance in patients with onychomycosis who fail antifungal therapy. Dermatology 207:375-380. [DOI] [PubMed] [Google Scholar]
- 10.Gupta, A. K., and Y. Kohli. 2003. In vitro susceptibility testing of ciclopirox, terbinafine, ketoconazole and itraconazole against dermatophytes and nondermatophytes, and in vitro evaluation of combination antifungal activity. Br. J. Dermatol. 149:296-305. [DOI] [PubMed] [Google Scholar]
- 11.Hofbauer, B., I. Leitner, and N. S. Ryder. 2002. In vitro susceptibility of Microsporum canis and other dermatophyte isolates from veterinary infections during therapy with terbinafine or griseofulvin. Med. Mycol. 40:179-183. [DOI] [PubMed] [Google Scholar]
- 12.Leber, R., S. Fuchsbichler, V. Klobucnikova, N. Schweighofer, E. Pitters, K. Wohlfarter, M. Lederer, K. Landl, C. Ruckenstuhl, I. Hapala, and F. Turnowsky. 2003. Molecular mechanism of terbinafine resistance in Saccharomyces cerevisiae. Antimicrob. Agents Chemother. 47:3890-3900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loeffler, J., and D. A. Stevens. 2003. Antifungal drug resistance. Clin. Infect. Dis. 6:S313-S341. [DOI] [PubMed] [Google Scholar]
- 14.Mukherjee, P. K., S. D. Leidich, N. Isham, I. Leitner, N. S. Ryder, and M. A. Ghannoum. 2003. Clinical Trichophyton rubrum strain exhibiting primary resistance to terbinafine. Antimicrob. Agents Chemother. 47:82-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Committee for Clinical Laboratory Standards. 2000. Reference method for broth dilution antifungal susceptibility testing of conidium-forming filamentous fungi. Approved standard M38-A. NCCLS, Wayne, PA.
- 16.Osborne, C. S., B. Hofbauer, B. Favre, and N. S. Ryder. 2003. In vitro analysis of the ability of Trichophyton rubrum to become resistant to terbinafine. Antimicrob. Agents Chemother. 47:3634-3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osborne, C. S., I. Leitner, B. Favre, and N. S. Ryder. 2005. Amino acid substitution in Trichophyton rubrum squalene epoxidase associated with resistance to terbinafine. Antimicrob. Agents Chemother. 49:2840-2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perea, S., A. W. Fothergill, D. A. Sutton, and M. G. Rinaldi. 2001. Comparison of in vitro activities of voriconazole and five established antifungal agents against different species of dermatophytes using a broth macrodilution method. J. Clin. Microbiol. 39:385-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanglard, D. 2002. Resistance of human fungal pathogens to antifungal drugs. Curr. Opin. Microbiol. 5:379-385. [DOI] [PubMed] [Google Scholar]
- 20.Sanglard, D. 2002. Clinical relevance of mechanisms of antifungal drug resistance in yeasts. Enferm. Infecc. Microbiol. Clin. 20:462-469. [DOI] [PubMed] [Google Scholar]