Abstract
Candida glabrata, which can become resistant to fluconazole, is a common cause of bloodstream infection. This study was performed to determine the significance of cross-resistance to new azole drugs among C. glabrata isolates recovered as a cause of infection in azole-treated hematopoietic stem cell transplant (HSCT) recipients. Seven cases of invasive candidiasis caused by C. glabrata occurred in HSCT recipients who were receiving azole therapy between January 2000 and December 2004 in our institution. Case characteristics were ascertained. Sequential colonizing and invasive isolates were examined to determine susceptibilities to fluconazole, itraconazole, and voriconazole, and molecular relatedness by restriction fragment length polymorphism (RFLP) analysis. Twenty-three C. glabrata isolates were recovered from 4 patients who developed candidemia while receiving fluconazole and three patients who developed candidemia while receiving voriconazole. The mode MICs of fluconazole, itraconazole, and voriconazole for these isolates were ≥64 μg/ml (range, 4 to ≥64 μg/ml), 2 μg/ml (range, 0.25 to ≥16 μg/ml), and 1 μg/ml (range, 0.03 to ≥16 μg/ml), respectively. Kendall tau b correlation coefficients demonstrated significant associations between the MICs of voriconazole with fluconazole (P = 0.005) and itraconazole (P = 0.008). Colonizing and invasive isolates exhibiting variable susceptibilities had similar RFLP patterns. These observations suggest that C. glabrata exhibits considerable clinically significant cross-resistance between older azole drugs (fluconazole and itraconazole) and voriconazole. Caution is advised when considering voriconazole therapy for C. glabrata candidemia that occurs in patients with extensive prior azole drug exposure.
Candida glabrata is currently the second most common cause of candidemia in the United States, and infection is associated with considerable mortality (6, 12). Microbial resistance to fluconazole readily develops; according to the 1993 to 2002 data from the ARTEMIS Global Antifungal Surveillance Program, 8.2% of C. glabrata isolates (n = 949) had a fluconazole MIC of ≥64 μg/ml and only 60% were truly susceptible by criteria outlined by previously published interpretive breakpoints (18, 19). Fluconazole use is thought to be one factor influencing the incidence of C. glabrata infections in certain geographic locations (16).
Voriconazole is an expanded-spectrum triazole derivative of fluconazole. The drug structurally resembles fluconazole except for the replacement of one of the triazole rings with a fluorinated pyrimidine and an additional α-methyl group. It is approved for the primary treatment of acute invasive aspergillosis, salvage therapy for rare but serious fungal infections such as those caused by Scedosporium apiospermum and Fusarium spp., esophageal candidiasis, and invasive candidiasis (8). Evaluation of the susceptibilities of a large number of C. glabrata isolates suggests that voriconazole activity may be better than that of fluconazole (17, 18); however, the potential of clinically significant resistance has become evident with recent reports noting the development of C. glabrata candidemia in patients receiving fluconazole (11) and voriconazole (7) therapy and the observation of cross-resistance developing in isolates recovered from the oral cavity and bloodstream (5). We performed this study to evaluate the clinical significance of azole cross-resistance in C. glabrata isolates recovered from colonizing and invasive sites of patients receiving azole therapy after hematopoietic stem cell transplantation (HSCT).
MATERIALS AND METHODS
Cases and definitions.
This study was approved by the Fred Hutchinson Cancer Research Center Institutional Review Board. To identify cases of fungal infections, HSCT recipients were monitored prospectively. A subset of patients had routine weekly screening for Candida isolates in mouthwash and stool samples. In addition, microbiology records were examined retrospectively for cases of bloodstream Candida glabrata infection in HSCT recipients between 1 January 2000 through 31 December 2004. During this period of time, patients received fluconazole (400 mg once daily) or itraconazole (2.5 mg/kg of body weight three times daily) as prophylaxis after HSCT (13) and voriconazole (3 to 4 mg/kg intravenously or 200 mg orally twice daily) for primary therapy of invasive aspergillosis. Voriconazole was also administered for prophylaxis in selected patients considered to have particularly high risks for invasive mold infection.
Candidemia was defined according to MSG/EORTC criteria (2). A C. glabrata invasive infection was considered to be an “azole breakthrough infection” if it developed after ≥7 days of azole therapy. Pharmacy records were reviewed for the use of antifungals prior to or during candidemia. Charts were reviewed for patient demographic information, underlying disease, HSCT type, comorbidity, immunosuppressive therapies, and outcome.
Microbial testing: susceptibilities and typing.
Candida glabrata isolates were stored frozen at −70°C until recovery by subculture. Fluconazole, itraconazole, and voriconazole susceptibilities were determined by the Clinical and Laboratory Standards Institute (CLSI, formerly NCCLS) M27-A microbroth dilution assay for yeast (14).
Molecular typing of sequential C. glabrata isolates obtained from patients was performed using a previously described restriction fragment length polymorphism method (10). Briefly, C. glabrata genomic DNA was isolated using the MasterPure yeast DNA purification kit (Epicenter, Madison, WI) according to the manufacturer's instructions. DNA was digested to completion with EcoRI, and Southern blots were hybridized with 32P-labeled Cg12, a moderately repetitive DNA probe (provided by D. Soll, University of Iowa) using standard methods (21).
Statistical analysis.
The strength of association between the MICs of fluconazole with itraconazole and voriconazole was assessed using the Kendall tau b rank correlation coefficient (τ). Bootstrapping and permutation methodologies were implemented to calculate 95% confidence intervals and P values, respectively, while appropriately accounting for correlated observations of isolates obtained within individuals.
RESULTS
During a 4-year period, 7 patients receiving azole therapy developed invasive C. glabrata infections. Case characteristics are listed in Table 1. The median time between the start of azole therapy and diagnosis of candidemia was 36 days (range, 13 to 173 days).
TABLE 1.
Cases of C. glabrata candidemiaa
| Case no. | Age (yr) | Underlying disease | Donor type | Day of candidemiab | Antifungal drugc |
|---|---|---|---|---|---|
| 1 | 54 | CML | MRD | 41 | Itraconazole (P) |
| 2 | 12 | MDS | MUD | 82 | Voriconazole (P) |
| 3 | 21 | AML | MUD | 92 | Voriconazole (P) |
| 4 | 41 | MM | MUD | 64 | Voriconazole (T) |
| 5 | 44 | HL | Autologous | 13 | Fluconazole (P) |
| 6 | 31 | MDS | MUD | 16 | Fluconazole (P) |
| 7 | 53 | NHL | MM-UD | 173 | Fluconazole (T) |
CML, chronic myelogenous leukemia; MDS, myelodysplastic syndrome; AML, acute myelogenous leukemia; MM, multiple myeloma; HL, Hodgkin's lymphoma; NHL, non-Hodgkin's lymphoma; MRD, human leukocyte antigen (HLA)-matched related donor; MUD, HLA-matched unrelated donor; MM-UD, HLA-mismatched unrelated donor.
Relative to day of receipt of stem cells (day 0).
Antifungal drugs received prior to or during candidemia. P, administered as part of a preventative algorithm; T, administered for treatment of a prior infection.
Colonizing and invasive isolates obtained from patients and corresponding susceptibilities are listed in Table 2. Three patients (cases 1 to 3) who had colonizing isolates available for analysis had developed colonization with isolates that had high MICs of multiple azoles prior to development of bloodstream infection. Colonizing isolates were not available for analysis from patients 4 to 7.
TABLE 2.
Antifungal susceptibility of C. glabrata isolates
| Case no. | Date collected (day/mo/yr)a | MIC (μg/ml) of:
|
||
|---|---|---|---|---|
| Fluconazole | Itraconazole | Voriconazole | ||
| 1 | 1/11/2000 | >64 | 0.25 | <0.03 |
| 1/25/2000 | 4 | 2 | 0.06 | |
| 1/30/2000 | 4 | 1 | 0.5 | |
| 2/8/2000 | 4 | 0.5 | 0.06 | |
| 2/14/2000 | >64 | 2 | 1 | |
| 3/14/2000 | >64 | 2 | 1 | |
| 3/21/2000 | >64 | 2 | 1 | |
| 4/7/2000 | >64 | 2 | 1 | |
| 4/11/2000 | >64 | 2 | 2 | |
| 4/25/2000 | >64 | 2 | 2 | |
| 5/2/2000 | >64 | 0.5 | 1 | |
| 5/9/2000 | >64 | 2 | 1 | |
| 2 | 8/5/2003 | >64 | 2 | 1 |
| 9/11/2004 | >64 | 2 | 1 | |
| 10/1/2004 | >64 | 4 | >16 | |
| 12/2/2004 | >64 | 2 | 2 | |
| 3 | 3/22/2004 | 8 | 1 | 0.25 |
| 7/10/2004 | >64 | >16 | 2 | |
| 7/17/2004 | >64 | >16 | 2 | |
| 4 | 7/19/2000 | >64 | >16 | 4 |
| 5 | 11/28/2002 | 8 | 1 | 0.25 |
| 6 | 7/27/2003 | >64 | >16 | >16 |
| 7 | 1/29/2003 | >64 | >16 | 4 |
Bloodstream isolates are shown in bold.
Isolates that had high fluconazole MICs (≥64 μg/ml) appeared to also have relatively high MICs of itraconazole (≥2 μg/ml) and voriconazole (1 to 2 μg/ml). Correlation coefficients suggest significant associations between the MICs of voriconazole and fluconazole (τ, 0.58; 95% confidence interval, 0.43 to 0.85; P, 0.005) and itraconazole (τ, 0.74; 95% confidence interval, 0.43 to 0.83; P, 0.008).
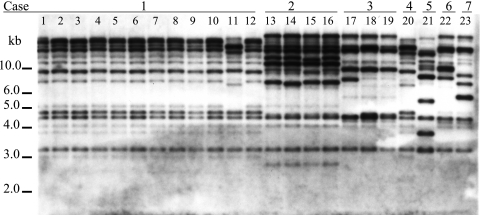
Molecular typing by restriction fragment length polymorphism demonstrated similar banding patterns among isolates recovered from the same patients but different patterns of isolates between patients (Fig. 1). Isolates recovered from case 1 were similar, except for colonizing isolate 11, which appeared to have a genotype similar to that of the isolate recovered from case 4. All other isolates were genetically dissimilar.
FIG. 1.
Restriction fragment length polymorphism analysis of Candida glabrata isolates included in this study. Cases from which isolates were obtained are indicated.
DISCUSSION
We report a series of 7 cases of invasive Candida glabrata infections that developed during azole therapy, with several isolates exhibiting relatively high MICs of both the “old” (fluconazole) and “new” (voriconazole) drugs approved for treatment of candidemia. This observation has important therapeutic implications, as it suggests that Candida glabrata can exhibit clinically meaningful resistance across different azole drugs.
The spectrum of activity of voriconazole is increased compared to fluconazole, with several studies reporting that both Candida albicans and non-C. albicans Candida species exhibit low MICs of voriconazole (17, 18). The finding that MIC50s and MIC90s of voriconazole for C. glabrata are low, approximately 0.25 and 1 μg/ml in large surveys of nonselected isolates (19), suggests that this drug retains good clinical activity. It is with this justification that investigators of a recent randomized trial evaluating voriconazole therapy for candidemia suggest that voriconazole (and caspofungin) should be considered better alternatives than fluconazole for primary therapy of candidemia (9). However, results of this and other recent case series (1, 11) suggest that these organisms may develop clinically meaningful cross-resistance among azole drugs, raising questions regarding the utility of voriconazole in individuals heavily pretreated with azole drugs.
Candida glabrata isolates for which MICs of both fluconazole and voriconazole are high have been observed. For instance, among the 46 C. glabrata isolates in the ARTEMIS study that were resistant to fluconazole (MIC, ≥64 μg/ml) and itraconazole (MIC, ≥1 μg/ml), 40 (87%) had a voriconazole MIC of ≥2 μg/ml (18, 19). In a study evaluating voriconazole administered for “salvage” therapy, 90 C. glabrata isolates that exhibited high fluconazole MICs (mean, 128 μg/ml) also exhibited relatively high mean voriconazole MICs (4 μg/ml) (15). In that study, the proportion of patients with C. glabrata infection who were treated successfully was approximately 25%; as clinical response is also dictated by host factors, success of “salvage” therapy may not be an optimal measure of the clinical impact of microbial resistance. Case series of what appear to be clinically significant microbial resistance are being reported (1, 11). Importantly, the characteristics and outcomes in these patients appear similar, as most of the patients have had a high amount of azole drug exposure in the setting of immunosuppressive conditions, such as after hematopoietic stem cell transplantation (1, 11).
Two recent studies have investigated the in vitro development of azole cross-resistance in detail. In one study, C. glabrata isolates recovered from clinical specimens during a 3-year hospital survey in Italy were evaluated (22). In this study, which included isolates that demonstrated both susceptible dose-dependent and -resistant fluconazole phenotypes, cross-resistance to voriconazole was noted. In another study, investigators observed rapid and stable acquisition of azole cross-resistance in C. glabrata isolates that were exposed to fluconazole upon serial culture in the laboratory (4). Our case series adds to our understanding of this phenomenon by demonstrating that colonizing C. glabrata isolates can develop increasingly high MICs to all three azoles during patient exposure to fluconazole, itraconazole, or voriconazole; these cases suggest clinical significance of cross-resistance in a heavily azole-pretreated population.
The mechanisms of resistance of C. glabrata to azoles are being elucidated. We have previously demonstrated that resistance to fluconazole in C. glabrata is associated with increased relative mRNA levels for ATP binding cassette transporters, CgCDR1, CgCDR2, and PDH1, which appeared to occur during patient exposure to fluconazole (3). More recently, evaluation of molecular mechanisms in matched and unmatched isolates recovered from hospitals in Italy provided evidence that increased mRNA of genes encoding CgCDR1, CgCDR2, and CgSNQ2 was associated with high MICs of both fluconazole and voriconazole (22).
Statistical analysis demonstrated a significant association between the MIC of voriconazole and those of fluconazole and itraconazole, respectively. However, there were isolates in this series that demonstrated variable MICs of the azole drugs; for instance, the first isolate from case 1 had a very high fluconazole MIC with low MICs of both itraconazole and voriconazole. Subsequent isolates demonstrated progressively increased MICs of both itraconazole and voriconazole. Evaluating the mechanism of azole resistance in each of these isolates will be of interest to determine whether efflux pumps, alterations in the azole target, or novel mechanism(s) are involved in sequential acquisition of increasing resistance in the series.
Results of molecular typing suggest that patients became infected with their colonizing strain, as was previously reported (20). Isolates infecting different people appeared to be different strains, having dissimilar patterns, with the exception of one isolate recovered from patients 1 and 4. Although both of those cases occurred in the year 2000, there was no epidemiological link noted, with consideration of overlapping space and time (data not shown). Also, the isolates recovered exhibited different susceptibility profiles. We cannot definitively state whether these isolates represent the same or similar strains.
Results of this study may have important implications when considering the definition of voriconazole “resistance.” Interpretive MIC breakpoints recently approved by CLSI to define voriconazole resistance are as follows: MIC of ≤1 μg/ml, susceptible; MIC of 2 μg/ml, susceptible dose dependent; MIC of ≥4 μg/ml, resistant. In the three patients who developed C. glabrata candidemia during receipt of voriconazole, the isolate MICs were 1 μg/ml (case 2), 2 μg/ml (case 3), and 4 μg/ml (case 4). Other reports noted C. glabrata isolates with MICs of >2 μg/ml “breaking through” voriconazole therapy (1, 7).
This study demonstrates that colonizing C. glabrata isolates can acquire decreased susceptibility to multiple azole drugs, including voriconazole, during exposure to both voriconazole and “older” compounds, fluconazole and itraconazole. Future research should be performed to determine the molecular mechanisms by which isolates become sequentially resistant to numerous azoles. Caution is advised when considering voriconazole therapy for C. glabrata candidemia in settings that predict fluconazole resistance.
Acknowledgments
A.A.P. received grant support from the 2004 John P. Utz Postdoctoral Fellowship in Medical Mycology. This work was in part supported by NIH grant AI05592.
A.A.P., J.L.G., J.F.S., and K.K. have no reported potential conflicts of interest. K.A.M. and M.R. have served as consultants for Pfizer.
REFERENCES
- 1.Alexander, B. D., W. A. Schell, J. L. Miller, G. D. Long, and J. R. Perfect. 2005. Candida glabrata fungemia in transplant patients receiving voriconazole after fluconazole. Transplantation 80:868-871. [DOI] [PubMed] [Google Scholar]
- 2.Ascioglu, A., J. Rex, B. DePauw, J. Bennett, J. Bille, F. Crokaert, D. Denning, J. Donnelly, J. Edwards, Z. Erjavec, D. Fiere, O. Lortholary, J. Maertens, J. Meis, T. Patterson, J. Ritter, D. Selleslag, P. Shah, D. Stevens, T. Walsh, and J. Ritter. 2002. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin. Infect. Dis. 34:7-14. [DOI] [PubMed] [Google Scholar]
- 3.Bennett, J. E., K. Izumikawa, and K. A. Marr. 2004. Mechanism of increased fluconazole resistance in Candida glabrata during prophylaxis. Antimicrob. Agents Chemother. 48:1773-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borst, A., M. T. Raimer, D. W. Warnock, C. J. Morrison, and B. A. Arthington-Skaggs. 2005. Rapid acquisition of stable azole resistance by Candida glabrata isolates obtained before the clinical introduction of fluconazole. Antimicrob. Agents Chemother. 49:783-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burn, A. K., A. W. Fothergill, W. R. Kirkpatrick, B. J. Coco, T. F. Patterson, D. I. McCarthy, M. G. Rinaldi, and S. W. Redding. 2004. Comparison of antifungal susceptibilities to fluconazole and voriconazole of oral Candida glabrata isolates from head and neck radiation patients. J. Clin. Microbiol. 42:5846-5848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fidel, P. L., Jr., J. A. Vazquez, and J. D. Sobel. 1999. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin. Microbiol. Rev. 12:80-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imhof, A., S. A. Balajee, D. N. Fredricks, J. A. Englund, and K. A. Marr. 2004. Breakthrough fungal infections in stem cell transplant recipients receiving voriconazole. Clin. Infect. Dis. 39:743-746. [DOI] [PubMed] [Google Scholar]
- 8.Johnson, L. B., and C. A. Kauffman. 2003. Voriconazole: a new triazole antifungal agent. Clin. Infect. Dis. 36:630-637. [DOI] [PubMed] [Google Scholar]
- 9.Kullberg, B. J., J. D. Sobel, M. Ruhnke, P. G. Pappas, C. Viscoli, J. H. Rex, J. D. Cleary, E. Rubinstein, L. W. Church, J. M. Brown, H. T. Schlamm, I. T. Oborska, F. Hilton, and M. R. Hodges. 2005. Voriconazole versus a regimen of amphotericin B followed by fluconazole for candidaemia in non-neutropenic patients: a randomised non-inferiority trial. Lancet 366:1435-1442. [DOI] [PubMed] [Google Scholar]
- 10.Lockhart, S. R., S. Joly, C. Pujol, J. D. Sobel, M. A. Pfaller, and D. R. Soll. 1997. Development and verification of fingerprinting probes for Candida glabrata. Microbiology 143(Pt 12):3733-3746. [DOI] [PubMed] [Google Scholar]
- 11.Magill, S., C. Shields, C. Sears, M. Choti, and W. Merz. 2006. Triazole cross-resistance among Candida spp.: case report, occurrence among bloodstream isolates, and implications for antifungal therapy. J. Clin. Microbiol. 44:529-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malani, A., J. Hmoud, L. Chiu, P. L. Carver, A. Bielaczyc, and C. A. Kauffman. 2005. Candida glabrata fungemia: experience in a tertiary care center. Clin. Infect. Dis. 41:975-981. [DOI] [PubMed] [Google Scholar]
- 13.Marr, K. A., F. Crippa, W. Leisenring, M. Hoyle, M. Boeckh, S. A. Balajee, W. G. Nichols, B. Musher, and L. Corey. 2004. Itraconazole versus fluconazole for prevention of fungal infections in patients receiving allogeneic stem cell transplants. Blood 103:1527-1533. [DOI] [PubMed] [Google Scholar]
- 14.National Committee for Clinical Laboratory Standards. 1997. Reference method for broth dilution antifungal susceptibility testing of yeasts, approved standard. NCCLS document M27-A. National Committee for Clinical Laboratory Standards., Wayne, PA.
- 15.Perfect, J. R., K. A. Marr, T. J. Walsh, R. N. Greenberg, B. DuPont, J. de la Torre-Cisneros, G. Just-Nubling, H. T. Schlamm, I. Lutsar, A. Espinel-Ingroff, and E. Johnson. 2003. Voriconazole treatment for less-common, emerging, or refractory fungal infections. Clin. Infect. Dis. 36:1122-1131. [DOI] [PubMed] [Google Scholar]
- 16.Pfaller, M. A., and D. J. Diekema. 2004. Twelve years of fluconazole in clinical practice: global trends in species distribution and fluconazole susceptibility of bloodstream isolates of Candida. Clin. Microbiol. Infect. 10(Suppl. 1):11-23. [DOI] [PubMed] [Google Scholar]
- 17.Pfaller, M. A., D. J. Diekema, S. A. Messer, L. Boyken, and R. J. Hollis. 2003. Activities of fluconazole and voriconazole against 1,586 recent clinical isolates of Candida species determined by broth microdilution, disk diffusion, and Etest methods: report from the ARTEMIS Global Antifungal Susceptibility Program, 2001. J. Clin. Microbiol. 41:1440-1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pfaller, M. A., S. A. Messer, L. Boyken, R. J. Hollis, C. Rice, S. Tendolkar, and D. J. Diekema. 2004. In vitro activities of voriconazole, posaconazole, and fluconazole against 4,169 clinical isolates of Candida spp. and Cryptococcus neoformans collected during 2001 and 2002 in the ARTEMIS global antifungal surveillance program. Diagn. Microbiol. Infect. Dis. 48:201-205. [DOI] [PubMed] [Google Scholar]
- 19.Pfaller, M. A., S. A. Messer, L. Boyken, S. Tendolkar, R. J. Hollis, and D. J. Diekema. 2004. Geographic variation in the susceptibilities of invasive isolates of Candida glabrata to seven systemically active antifungal agents: a global assessment from the ARTEMIS Antifungal Surveillance Program conducted in 2001 and 2002. J. Clin. Microbiol. 42:3142-3146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Redding, S. W., K. A. Marr, W. R. Kirkpatrick, B. J. Coco, and T. F. Patterson. 2004. Candida glabrata sepsis secondary to oral colonization in bone marrow transplantation. Med. Mycol. 42:479-481. [DOI] [PubMed] [Google Scholar]
- 21.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, 2nd ed. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 22.Sanguinetti, M., B. Posteraro, B. Fiori, S. Ranno, R. Torelli, and G. Fadda. 2005. Mechanisms of azole resistance in clinical isolates of Candida glabrata collected during a hospital survey of antifungal resistance. Antimicrob. Agents Chemother. 49:668-679. [DOI] [PMC free article] [PubMed] [Google Scholar]