Abstract
OBJECTIVE
Being of rural origin is one of the few predictors of whether medical students choose either family or rural practice as a career. This study investigates what proportion of applicants are of rural origin, what their grades are, and whether they are accepted.
DESIGN
Mailed survey using the postal codes of Ontario medical school applicants’ residences when they attended secondary school to link them to communities. Applicants of rural origin were defined as having attended secondary school while residing in communities with core populations of fewer than 10 000 people.
SETTING
Province of Ontario, its six medical schools, and its 1 500 000 rural citizens (13% of the total population).
PARTICIPANTS
All 4948 applicants to Ontario medical schools in 2002 and 2003 who had gone to high school in Ontario.
MAIN OUTCOME MEASURES
Proportion of rural applicants among all applicants in the given years. Mean grade point averages (GPA) and Medical College Admission Test (MCAT) scores attained by applicants of both urban and rural origin. Proportion of rural students among all students admitted to medical schools.
RESULTS
While 13% of the Ontario population is rural, only 7.3% of Ontario applicants to medical school were of rural origin (P < .001). On average, the GPAs of applicants of rural and urban origin were identical at 3.42 (P = .995 not significant [NS]). The MCAT scores averaged 8.9 for applicants of rural origin and 9.0 for applicants of urban origin (P = .36 NS). Applicants of rural origin were admitted to medical school as frequently as applicants of urban origin (1:5.6 vs 1:4.7, P = .139 NS).
CONCLUSION
Although students of rural origin in Ontario apply to medical school less frequently than students of urban origin do, those that do apply have similar grades to those of urban applicants and are equally likely to be accepted.
Abstract
OBJECTIF
L’origine rurale d’un étudiant en médecine est un des rares éléments qui peuvent permettre de prévoir si un étudiant en médecine choisira de faire carrière en médecine familiale ou rurale. Cette étude voulait savoir quelle est la proportion des candidats qui viennent d’un milieu rural, quelle est leur cote R, et dans quelle proportion ils sont admis.
TYPE D’ÉTUDE
Enquête postale à l’aide des codes postaux des lieux où résidaient les candidats aux études médicales en Ontario durant leur études secondaires, afin d’établir leurs communautés d’origine. Par candidats d’origine rurale, on entendait ceux qui vivaient dans une collectivité de moins de 10 000 âmes durant leurs études secondaires.
CONTEXTE
L’Ontario, ses six facultés de médecine et ses 1 500 000 citoyens ruraux (13% de la population totale)
PARTICIPANTS
Les 4948 candidats à l’admission aux facultés de médecine ontariennes en 2002 et 2003 ayant fait leurs études secondaires en Ontario.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Pourcentage des candidats d’une année donnée qui proviennent d’un milieu rural. La moyenne des notes pondérées et score au Medical College Admission Test (MCAT) pour les candidats ruraux et urbains. Proportion des candidats admis en médecine qui proviennent du milieu rural.
RÉSULTATS
Même si 13% de la population ontarienne est rurale, seulement 7,3% des Ontariens qui font une demande d’admission en médecine sont d’origine rurale (P < ,001). En moyenne, les candidats ruraux et urbains ont des moyennes des notes pondérées identiques de 3,42 (P = ,995, non significatif [NS]). Les candidats ruraux avaient en moyenne des scores de 8,9 au MCAT contre 9,0 pour les urbains (P = ,36, NS). Le taux d’admission en médecine était équivalent dans les deux groupes (1:5,6 pour les candidats urbains contre 1:4,7 pour les ruraux, P = ,139, NS).
CONCLUSION
Même s’ils se présentent moins souvent à l’admission en médecine que les étudiants urbains, les étudiants ontariens d’origine rurale qui posent leur candidature ont les mêmes notes que les candidats urbains et les mêmes chances d’être admis.
EDITOR’S KEY POINTS.
Ontario’s population is 13% rural, but only 7.3% of medical school applicants are from rural settings.
Rural applicants have similar grade point averages and Medical College Admission Test scores to those of their urban counterparts, although this finding is limited by incomplete reporting.
Rural applicants are accepted into medical schools in the same proportion as urban applicants.
POINTS DE REPÈRE DU RÉDACTEUR.
Même si 13% de la population ontarienne est rurale, seulement 7,3% de ceux qui demande leur admission en médecine sont d’origine rurale.
Les candidats ruraux et urbains ont des moyennes des notes pondérées et des scores au MCAT semblables, quoique cette conclusion soit limitée par des données incomplètes.
Les candidats ruraux sont admis en médecine dans la même proportion que les urbains.
Health care systems that rely on family physicians are efficient and yield better health outcomes than those that have a large proportion of specialists.1,2 Ready access to any health care for vulnerable rural populations often depends on the availability of family physicians. Maintaining or increasing interest in generalism and rural medicine in a culture of increasing specialization is thus a worthy challenge for policy makers. Choosing family practice and choosing a rural practice location are complex decisions of nature and nurture. One factor associated with both choices is whether a person comes from a rural background.
Canadian literature on choosing to practise in rural locations is limited. Easterbrook et al3 found that, among 159 family practice residents at Queen’s University in Kingston, Ont, those of rural origin (from areas with less than 10 000 population) were 2.3 times more likely than those from larger communities to choose to practise in rural communities immediately after graduation.
Wright et al4 found that, for 136 medical students graduating from McGill University, exposure to role models in a particular clinical field was strongly associated with medical students’ choice of clinical field for residency training. American studies indicated, however, that, while a rural family medicine preceptorship was important, medical students of rural origin were four times as likely to choose rural primary care, even in a standard urban curriculum. Rural origin and interest in primary care during the first year of training accounted for 78% of the probability that a graduating student would choose rural primary care.5
Wright and colleagues6 found that, among first-year medical students in Alberta and British Columbia, students who were older, were concerned about medical lifestyle, and grew up in smaller communities were more interested in family medicine as a career. In their multivariate analysis, interest in family practice increased progressively with smaller community of origin and was 2.3 times greater for students from communities of less than 50 000 population than for those from larger communities. A survey of 981 Canadian first-year medical students in 20017 found that students of rural origin were underrepresented in comparison with the proportion of Canadians living in rural areas (10.8% vs 22.4%).
Canadian medical schools require university-level courses as prerequisites. Finnie et al showed that, while 34% of men from urban areas and 41% of women from urban areas attended Canadian universities in 1995, only 21% of men from rural areas and 33% of women from rural areas did so.8 Frenette showed that having to travel more than 80 km to university reduced postsecondary education participation rates among Canadian rural students in all social and economic strata, but particularly among poorer families.9,10 No studies to date have looked at the proportion of students from rural areas among medical school applicants.
Applicants to the five Ontario medical schools use the Ontario Medical School Application Service (OMSAS) whether they apply to only one or to more of the schools. Several research questions can be answered from OMSAS data. Are students from rural Ontario less likely than those of urban origin to apply to Ontario medical schools? Do students from rural areas have lower marks than those from urban areas? Are applicants of rural origin less likely to be successful in getting into medical school?
METHODS
In fall 2000, the OMSAS agreed to ask for the postal codes of the residences where applicants lived when they attended secondary school. These postal codes, for 2002 and 2003 medical school applicants, were linked to community locations that could be categorized as either rural or urban, using Statistics Canada’s definition of rural areas and small towns.11 Applicants of rural origin were defined by having attended secondary school while residing in communities with core populations of less than 10 000.
Because the applicants of rural origin were few, the two intake years, 2002 and 2003, have been pooled for this analysis. Because 84.5% of the students admitted to Ontario’s medical schools were from Ontario, our analyses were limited to the 4948 applicants from Ontario. Proportions of applicants of rural and urban origins were determined by linking the postal codes on their application forms with Statistics Canada’s geographic data.
For applicants of both rural and urban origin, comparative descriptive statistics were derived for their grade point averages (GPAs) and Medical College Admission Test (MCAT) scores. The relative proportions of applicants of rural and urban origin accepted into Ontario medical schools were also computed. Statistical analysis was done using SPSS software. The study was approved by the Ethics Review Board at the University of Western Ontario in London.
RESULTS
In 2002, 2246 students from Ontario applied to the province’s medical schools; in 2003, 2702 applied. All provided postal codes, which allowed us to define them as having rural or urban backgrounds. There were 4588 applicants from urban areas and 360 from rural areas; only 7.3% of the applicants (360 of 4948) were of rural origin.
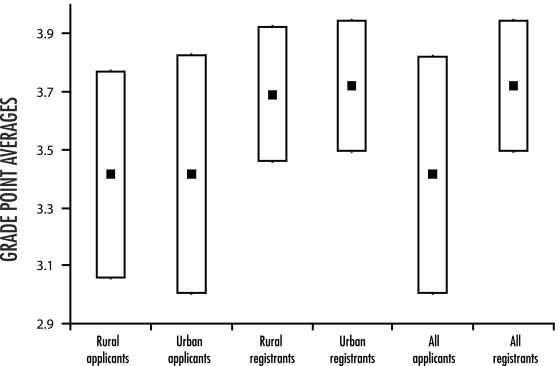
Grade point averages were available from the OMSAS database for 96% of applicants (n = 4749); the proportions of missing GPAs were equally distributed among rural and urban applicants. The MCAT scores required by three of the five Ontario medical schools were available for 43.0% of the rural students and 58.6% of the urban students. On average, the GPAs of applicants of rural and urban origins were identical at 3.42 (P = .995) (Figure 1). Average GPA for successful applicants (registrants) was 3.72.
Figure 1. Means and standard deviations of examination results of Ontario medical school applicants and registrants.
A) Grade point averages; B) Medical College Admission Test scores.
There were 505 successful applicants in 2002 and 529 in 2003. Overall, 6.2% of the successful applicants were of rural origin. One in 5.6 applicants of rural origin was admitted compared with one in 4.7 applicants of urban origin (P = .139).
DISCUSSION
The most important finding of this study is that students of rural origin are only 56% as likely to apply to medical school in Ontario as they would be if they represented the overall rural population of the province. While Ontario is 13% rural, only 7.3% of the Ontario applicants were of rural origin, and they made up only 6.2% of successful applicants. We speculate that this could be due to a lack of role models in rural areas or to financial barriers, or to both. There are, however, no studies to date dealing specifically with Ontario medical school applicants that would confirm these speculations.
There are half as many doctors in Canada’s rural regions as there are for comparable urban populations, and hence, very few physicians to model medicine as a career.12 Rural parents are on average less well educated than urban parents and are less likely to encourage their children to obtain post-secondary education.13 People in rural areas are poorer than their urban counterparts13 and are thus less likely to be able to support their sons and daughters through long and expensive training programs. This is particularly true when students do not live within commuting distance of a university where they can attain the prerequisites for medical school.9,10 Prospective students have to overcome the cultural and financial barriers to leaving home and moving to the city.14
While data on medical school applicants have not been studied elsewhere in a similar fashion, our findings are consistent with other findings in the literature on the underrepresentation of students of rural origin in medical schools. In 1989 in Australia, 10% of medical students were of rural origin in a country that is 25% rural.14
More detailed work needs to be done to characterize medical school applicants, both here and in other places, to gain a deeper appreciation of why medical schools receive proportionally fewer applications from students in rural areas than from students in urban areas. Reports from other places indicate encouragingly that it is possible to increase the number of students of rural origin in medical schools to a demographically equitable level. In Australia, for example, after some years of struggle, admission criteria were reformed to meet social accountability standards, and specially targeted national bursaries were offered to students of rural origin to reduce potential financial barriers. By 2000, the proportion of students of rural origin had increased to 25% of that country’s medical classes.14
One strategy adopted in Canada to make medical school more accessible to students of rural origin can be found in Quebec. In that province, the four medical schools have started to add 0.5 to the GPAs of applicants from rural and remote Quebec. This and other strategies might have to be explored to increase the proportion of both applicants and successful registrants of rural origin in Ontario’s medical schools.
Limitations
Our hypothesis that applicants of rural origin had poorer grades was unsubstantiated. One limitation of this result is the 4% of applicants for whom we have no GPAs. Data were missing primarily on postgraduate applicants and applicants who had taken a portion of their undergraduate training outside the country. Because applicants of rural and urban origins were equally likely to have missing GPA data, this small amount of missing data is unlikely to skew the analysis.
A more serious limitation is that more rural than urban applicants did not provide MCAT scores. This might simply reflect the fact that MCAT testing is not readily available to rural applicants who could be “home” for the summer when MCATs are usually written, but the reason might be more complex. Students who do not write the MCAT examinations, or who do but do not do well, might choose to apply only to schools that do not require MCAT scores (at the time of the study, in Ontario, these were McMaster University in Hamilton and the University of Ottawa). Thus, MCAT data should be treated with caution.
Conclusion
Students of rural origin are much less likely than their urban counterparts to apply to medical school. Once they do apply, their grades are comparable, and they appear to be accepted just as often as students from urban backgrounds.
Acknowledgments
Funding for this study was received from the Ontario Medical Association’s Continuing Medical Education Program for Rural and Isolated Physicians.
Biographies
Dr Hutten-Czapski practises rural family medicine in Haileybury, Ont.
Mr Pitblado teaches at Laurentian University in Sudbury, Ont.
Dr Rourke is Dean of Medicine at Memorial University of Newfoundland in St John’s.
Footnotes
Competing interests: None declared
References
- 1.Starfield B. Primary care: concepts, evaluation, and policy. New York, NY: Oxford University Press; 1992. [Google Scholar]
- 2.Starfield B, Shi L. Policy relevant determinants of health: an international perspective. Health Policy. 2002;60:201–218. doi: 10.1016/s0168-8510(01)00208-1. [DOI] [PubMed] [Google Scholar]
- 3.Easterbrook M, Godwin M, Wilson R, Hodgetts G, Brown G, Pong R, et al. Rural background and clinical rotations during medical training: effect on practice location. CMAJ. 1999;160:1159–1163. [PMC free article] [PubMed] [Google Scholar]
- 4.Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12(1):53–56. doi: 10.1046/j.1525-1497.1997.12109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabinowitz HK, Diamond JJ, Markham FW, Paynter NP. Critical factors for designing programs to increase the supply and retention of rural primary care physicians. JAMA. 2001;286:1041–1048. doi: 10.1001/jama.286.9.1041. [DOI] [PubMed] [Google Scholar]
- 6.Wright B, Scott I, Woloschuk W, Brenneis F. Career choice of new medical students at three Canadian universities: family medicine versus specialty medicine. CMAJ. 2004;170:1920–1924. doi: 10.1503/cmaj.1031111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dhalla IA, Kwong JC, Streiner DL, Baddour RE, Waddell AE, Johnson IL. Characteristics of first-year students in Canadian medical schools. CMAJ. 2002;166:1029–1035. [PMC free article] [PubMed] [Google Scholar]
- 8.Finnie R, Lascelles E, Sweetman A. Who goes? The direct and indirect effects of family background on access to post-secondary education. Catalogue no. 11F0019MIE2005237. Ottawa, Ont: Statistics Canada; 2005. [Google Scholar]
- 9.Frenette M. Too far to go on? Distance to school and university participation. Catalogue no. 11F0019MIE2002191. Ottawa, Ont: Statistics Canada; 2002. [Google Scholar]
- 10.Frenette M. Access to college and university: does distance matter? Catalogue no. 11F0019MIE2003201. Ottawa, Ont: Statistics Canada; 2003. [Google Scholar]
- 11.Du Plessis V, Beshiri R, Bollman RD, Clemenson H. [cited 2005 June 23];Definitions of rural. Statistics Canada catalogue no. 21-006-XIE. 2001 3(3):1–16. Available at: http://www.statcan.ca/english/freepub/21-006-XIE/21-006-XIE2001003.pdf.
- 12.Society of Rural Physicians of Canada. Comparative regional statistics. FP/GP numbers. Shawville, Que: Society of Rural Physicians of Canada; 2005. [cited 2005 June 23]. Available at: http://www.srpc.ca/numbers.html. [Google Scholar]
- 13.Statistics Canada. [cited 2005 June 23];Mapping the socio-economic diversity of rural Canada. Catalogue no. 21-006-XIE. 2004 5(2):1–33. Available at: http://www.statcan.ca/english/freepub/21-006-XIE/21-006-XIE2003002.pdf.
- 14.Dunbabin J, Levitt L. [cited 2005 June 23];Rural origin and rural medical exposure: their impact on the rural and remote medical workforce in Australia. 2003 3:212. Available at http://rrh.deakin.edu.au. [PubMed]