Abstract
OBJECTIVE
To examine where rural physicians grew up, when during their training they became interested in rural medicine, factors influencing their decision to practise rural medicine, and differences in these measures according to rural or urban upbringing.
DESIGN
Mailed survey.
SETTING
Rural Canada.
PARTICIPANTS
Rural family physicians who graduated between 1991 and 2000 from a Canadian medical school.
MAIN OUTCOME MEASURES
Backgrounds of recently graduated rural physicians, when physicians first became interested in rural practice during training, and most influential factors in decisions to practise rural medicine.
RESULTS
Response rate was 59% (382/651). About 33% of rural physicians grew up in communities of less than 10 000 people, 44% in cities of 10 000 to 499 999 people, and 23% in cities of more than 500 000 people. Physicians raised in rural areas were more likely than those raised in urban areas to have some interest in rural family practice at the start and end of medical school (90% vs 67% at the start, 98% vs 91% at the end, respectively, P < .0001). Physicians raised in urban areas were more likely to state that rural medical training was the most influential factor in their choice of rural practice (19% vs 9%, P = .015). Other factors cited as influential were the challenge of rural practice (24% for both urban and rural upbringing), rural lifestyle (14% for urban and 18% for rural upbringing) and, for physicians raised in rural areas, having grown up or spent time in a rural area (27% for rural and 4.1% for urban upbringing, P < .001). Financial incentives were least frequently cited as the most influential factor (7.5% for urban and 4.9% for rural upbringing, P = .35).
CONCLUSION
Although other studies have suggested that physicians with a rural upbringing are more likely to practise rural medicine and policy makers might still wish to target students raised in rural areas as candidates for rural medicine, this study shows that physicians raised in urban areas remain the main source of human resources for rural communities. They account for two thirds of new physicians in rural areas. Education in rural medicine during medical training has a stronger influence on physicians raised in urban areas than on physicians raised in rural areas. Undergraduate and postgraduate training periods, therefore, offer an important opportunity for recruiting physicians raised in urban areas to rural practice.
Abstract
OBJECTIF
Déterminer le milieu dans lequel les médecins ruraux ont grandi, le moment de leur formation où ils ont commencé à s’intéresser à la médecine rurale et les facteurs qui ont influencé leur décision de pratiquer la médecine rurale; établir si les résultats obtenus diffèrent entre ceux qui ont été élevés en ville ou à la campagne.
TYPE D’ÉTUDE
Enquête postale.
CONTEXTE
Le Canada rural.
PARTICIPANTS
Médecins de famille ruraux diplômés d’une faculté de médecine canadienne entre 1991 et 2000.
PRINCIPAUX POINTS À L’ÉTUDE
Le passé des médecins ruraux récemment diplômés, le moment de leur formation où ils ont commencé à s’intéresser à la médecine rurale et les facteurs qui ont le plus influé sur leur décision de pratiquer à la campagne.
RÉSULTATS
Le taux de réponse se situait à 59% (382/651). Quelque 33% des médecins ruraux avaient grandi dans des collectivités de moins de 10 000 habitants, 44% dans des villes de 10 000 à 499 999 habitants et 23% dans des villes de plus de 500 000 habitants. Les médecins d’origine rurale étaient plus enclins que ceux provenant de centres urbains à s’intéresser à la pratique familiale rurale au début et à la fin de leurs études en médecine (respectivement 90% par rapport à 67% au début, et 98% contre 91% à la fin, P < ,0001). Les médecins issus de milieux urbains étaient plus portés à dire que la formation en médecine rurale était le facteur qui avait le plus influencé leur choix de la pratique rurale (19% par rapport à 9%, P = .015). Au nombre des autres facteurs mentionnés figuraient les défis de la pratique rurale (24% tant chez ceux d’origine urbaine que rurale), le mode de vie en milieu rural (14% pour les citadins et 18% pour ceux de provenance rurale) et, pour les médecins élevés dans des milieux ruraux, ayant grandi ou passé du temps en milieu rural (27% chez les médecins d’origine rurale et 4,1% chez les citadins, P < .001). Les mesures d’incitation financière étaient le moins souvent mentionnées comme le facteur le plus influent (7,5% chez les citadins et 4,9% chez ceux d’origine rurale, P= ,35).
CONCLUSION
Contrairement aux études qui suggèrent que les médecins élevés en milieu rural ont plus de chance d’aller en pratique rurale et aux politiques des décideurs qui voudraient encore favoriser les candidatures des étudiants élevés en milieu rural pour cette raison, cette étude démontre que les médecins élevés en milieu urbain demeurent le principal réservoir de ressources humaines pour les collectivitiés rurales. Ils représentent les deux-tiers des nouveaux médecins dans les régions rurales. Le fait d’avoir eu une formation sur la médecine rurale durant les études médicales a plus d’influence chez les médecins élevés en milieu urbain que chez ceux élevés en milieu rural. Les périodes de formation au premier et au deuxième cycle représentent donc une occasion idéale pour amener les médecins élevés en milieu urbain à pratiquer à la campagne.
EDITOR’S KEY POINTS.
This study found that physicians who grew up in rural areas were more likely to return to rural areas to practise. Most rural physicians, however, actually come from cities and were greatly influenced by their rural training experiences.
For students from both urban and rural backgrounds, the challenges of rural practice and its lifestyle had the greatest positive influence on choice of practice location.
Are encouraging rural applicants to apply for medicine, making exposure to rural practice available during training, and promoting the challenges and lifestyle of rural practice to physicians from both urban and rural backgrounds the best strategies for recruitment to rural practice?
POINTS DE REPÈRE DU RÉDACTEUR.
Cette étude a montré que les médecins élevés en milieu rural ont plus de chances de retourner pratiquer en région rurale. Toutefois, la plupart des médecins ruraux proviennent des villes et ont été fortement influencés par leur expérience de formation rurale.
Pour les étudiants d’origine urbaine comme rurale, le défi de la pratique rurale et de son mode de vie est le facteur le plus important dans le choix du lieu de pratique.
Pour améliorer le recrutement en médecine rurale, devrait-on inciter les étudiants ruraux à se porter candidats en médecine, offrir plus de stages en médecine rurale durant la formation, et vanter les défis et le mode de vie de la pratique rurale auprès des médecins des milieux urbains comme ruraux?
Inequitable geographic distribution of physicians in countries with vast areas, such as Canada, the United States, and Australia, has been a continuing challenge for policy makers. Attempts have been made to encourage more doctors to practise in rural areas for the past 40 years. These attempts have included financial incentives; recruitment drives; offers of free tuition, access to educational resources, teaching opportunities, and locum tenens1; and medical education specifically targeted at preparing doctors for rural practice.2
One factor identified as predicting rural practice has been where a physician grew up. Studies from Canada,3,4 the United States,5-9 and Australia10,11 demonstrate that people raised in rural communities are two to four times more likely to ultimately work in rural areas. This prompted suggestions that more young people with rural backgrounds be admitted to medical schools.12
One of the Australian studies,11 however, noted that, although rural background predicts rural practice, most rural practitioners actually did not spend any of their formative years in rural areas. This finding suggests a great potential for bringing physicians raised in urban areas into rural practice. We could not find any studies that explored this phenomenon in Canada.
Another predictor of rural practice cited in the literature is exposure to rural training. Graduates of both undergraduate medical programs with a rural focus13 and postgraduate rural residency training programs14,15 in the United States had relatively high rates of participation in rural practice. Choosing rural electives has also been associated with recruitment to rural areas; this appears to have a greater effect on people raised in urban areas.16 What is less clear is exactly when physicians solidify a decision to engage in rural practice and whether these key decision points vary by whether physicians were raised in rural or urban areas.
Studies have also examined other factors influencing the decision to choose rural practice. Spouses’ preferences and proximity to family also strongly influence practice location.17 Financial incentives influence choice of rural practice, but have a greater effect on short-term recruitment than on long-term retention.18 Again, however, the difference in degree of influence of these factors on physicians raised in rural and urban areas remains to be clarified.
This study has three objectives. First, it explores whether recently graduated Canadian rural physicians tend to have urban or rural backgrounds, and whether, as in Australia, most of Canada’s rural practitioners were raised in urban areas. Second, it examines whether the time during a physician’s training at which he or she became interested in rural medicine differs by whether the physician has a rural or urban background. Third, it identifies the most influential factors in physicians’ decisions to practise rural medicine and how these factors differ depending on where physicians were raised.
METHOD
For our survey, we developed broad questions examining the influence of rural medical education on the decision to engage in rural practice. The survey was pilot-tested by 10 rural family physicians who provided feedback on questions, wording, and layout. Questions that relate to this study are listed below.
How large was the community in which you lived when you were of high school age?
Please rate your level of interest in rural family practice at different stages of your training and career. (Stages of training were start of medical school, end of medical school, and end of postgraduate training. Levels of interest were “little or no interest in rural medicine”; “some interest in rural medicine, but I was uncertain”; and “was certain I wanted to practise rural medicine.”)
How much of a positive influence did the following factors have on your decision to work in a rural area? (Factors included rural training, financial incentives, past exposure to rural areas, and other issues listed as “other” factors. Respondents were asked to identify first, second, and third most influential factors.)
Other questions examined length of exposure to rural practice during postgraduate training and breadth of rural experiences (eg, opportunities to work in very remote settings with no local specialist backup) and the effect of these training-program factors on choice of rural practice.
Sample size calculations indicated that all recently graduated rural family physicians needed to be sampled in order to detect a difference in proportion of 0.10, assuming an alpha of .05, a power of .80, and a response rate of 50%. Accordingly, we surveyed all family physicians and general practitioners in Canada who had graduated recently (between 1991 and 2000) from Canadian medical schools and were practising at the time of the study (2002) in rural communities (less than 10 000 people and situated outside Census Agglomeration or Census Metropolitan areas). Potential respondents meeting these criteria were identified from the Southam Medical Database, a commercial database widely used in Canada. A French version of the questionnaire was sent to Francophone physicians in Quebec and New Brunswick. Physicians received a first mailing in October 2002, then a reminder card and a second mailing. A third mailing was done in regions where response rates were still below 50% after the first two mailings.
We tested for differences in characteristics between those with urban upbringing and those with rural upbringing. Because outcomes of interest were categorical variables, we used chi-square tests. In testing for differences in “other” factors, we limited formal statistical testing to four broad categories of factors rather than individual factors to avoid reduction in statistical power due to multiple comparisons. Analyses were performed using SAS version 8.
Ethics approval was obtained from Sunnybrook and Women’s College Health Sciences Centre in Toronto, Ont.
RESULTS
We surveyed 784 physicians; 133 returned questionnaires were removed due to ineligibility. Reasons for ineligibility included not in family practice, not in rural practice, did not graduate between 1991 and 2000, and no longer located at the address listed in the database. This left an eligible sample of 651 physicians. The 382 completed eligible questionnaires represent an effective response rate of 59% (382/651). The response rate was higher among Anglophones (63%) than among Francophones (51%). Mean age of respondents was 35 years. There was no significant difference between respondents and nonrespondents in average age or number of years since graduation. Female physicians were more likely to return the survey than male physicians were (65% vs 51%, P = .0004).
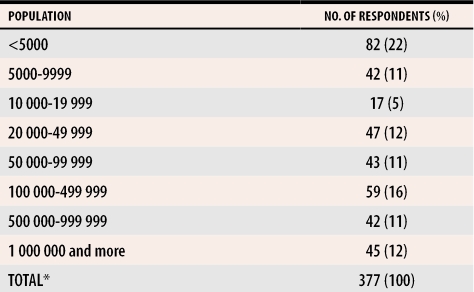
Among respondents, one third grew up in communities of less than 10 000 people; the remainder grew up in urban communities of widely different sizes. Almost one quarter of rural physicians grew up in cities with more than half a million population (Table 1).
Table 1.
Size of community where physicians practising in rural areas were raised
*Data missing for five participants.
As rural physicians progressed through training, their interest in rural medicine increased. The proportion of respondents who were certain they wanted to practise rural medicine rose from only 28% at the start of medical school to 77% by the end of postgraduate training. Respondents with a rural upbringing were more likely than those with an urban upbringing to have at least some interest in rural family practice at the start of medical school (90% vs 67%, P <.0001). At the end of medical school, this difference, while substantially reduced, remained significant (98% vs 91%, P <.0001). By the end of postgraduate training, the difference in proportion of physicians reporting little interest in rural medicine disappears, although physicians raised in rural areas were still more likely to report they were certain they wanted to practise rural medicine (92% versus 71%, P < .0001).
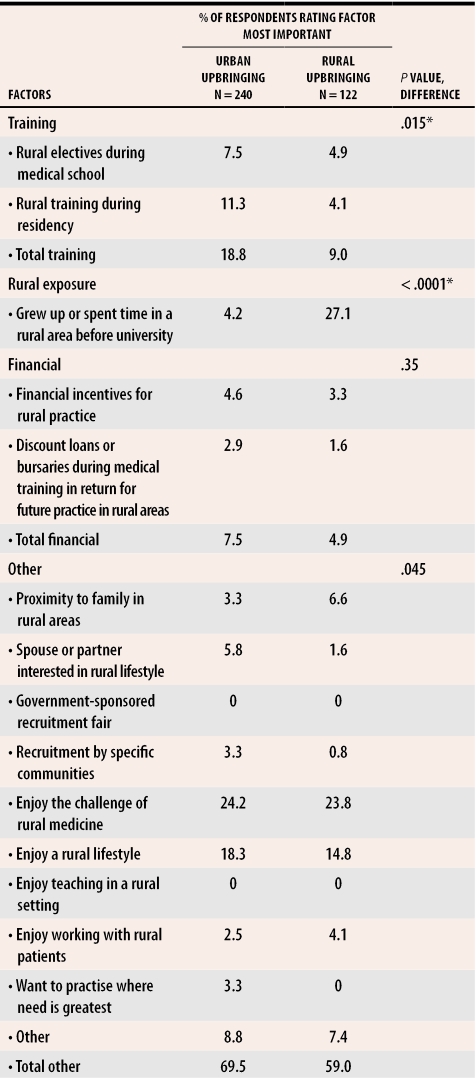
The challenge of rural medicine and enjoyment of a rural lifestyle were two of the most important factors for physicians from both urban and rural backgrounds in the decision to practise rural medicine (Table 2). Physicians raised in urban areas were more likely to indicate that exposure to rural practice during medical school or residency was the most important factor in their decision to practise rural medicine. Physicians raised in rural areas were more likely to report that having spent time in rural areas before university was the most important factor; among these physicians, this was most commonly cited as the most important factor. There were no statistically significant differences between the two types of physicians with respect to other factors.
Table 2.
Most important factors in deciding to practise rural medicine
*Significant to P < .05 using modified Bonferroni adjustment for multiple comparisons. P value for overall chi-square comparison was < .0001.
DISCUSSION
This study suggests that it is indeed possible to entice individuals who grew up in urban areas into rural practice. Two thirds of rural physicians who responded did not come from rural backgrounds. This finding has been noted previously in Australia,11 and our study now confirms that a similar pattern exists in Canada. Those with an urban upbringing appear to be attracted to rural medicine for a variety of reasons, including community recruitment, challenge, a desire to serve society, and exposure during residency training.
This study also sheds new light on the timing of decisions about rural practice. Physicians raised in rural areas have greater interest in rural medicine before medical school than physicians raised in urban areas. Interest in rural practice gradually increases as training progresses, especially among physicians from urban backgrounds. One third of these physicians had little or no interest in rural medicine before medical school. Only 9% had little or no interest by the end of medical school, and only 2.5% by the end of postgraduate training. This finding underscores the fact that medical school and postgraduate training offer important opportunities for enticing physicians raised in urban areas into rural practice.
Those raised in urban areas appear to be more sensitive to rural training than those raised in rural areas. They rate exposure to rural medicine through electives and rotations as having greater influence on their decision to choose rural practice. Among these physicians, rural training might offer more than just the clinical skills needed to survive in a rural environment. It might also offer exposure to other positive aspects of the rural experience, such as the challenge of rural practice and a rural lifestyle. These factors were rated highly influential by physicians raised in urban areas. Without exposure to rural settings, physicians raised in urban areas would have difficulty appreciating these aspects of rural practice.
Our findings do not contradict previous studies that report that those who grew up in rural areas are more likely to enter rural practice. The reality, however, is that the number of rural students applying to and getting into medical school remains small. According to one study, while rural residents account for more than 20% of the Canadian population, only slightly more than 10% of medical students are of rural origin.19 Although policies that give rural students preferential access to medical training have merit, training programs should also consider the fact that students from urban backgrounds will be an important source of rural physicians.
Limitations
First, there is the potential for respondent bias. Baseline characteristics for respondents and nonrespondents were, however, reasonably similar. Second, there is a possibility of recall bias in responses to questions about the timing of interest in rural medicine and the effect of various factors on choice of rural medicine. This, however, is mitigated to some extent by restricting the sample to more recent graduates. Third, we examined only one aspect of rural upbringing: the high school years. This narrow definition was used because of space limitations on the survey. One Australian study confirms, however, that location of primary and secondary schooling both predict rural practice.11
Conclusion
Other studies suggest that physicians with a rural upbringing are more likely to practise rural medicine, and policy makers might still wish to target students raised in rural areas as candidates for rural medicine. Physicians with an urban upbringing, however, remain the main source of human resources for rural communities, where they account for two thirds of new physicians. Rural education during medical training has a significantly stronger influence on physicians raised in urban areas than on physicians raised in rural areas. Undergraduate and postgraduate training periods, therefore, provide an important opportunity for recruiting physicians raised in urban areas to rural practice.
Acknowledgments
We gratefully acknowledge funding for this study from the Canadian Institutes of Health Research, grant no. RLH-54126.
Biographies
Dr Chan is a Senior Scientist at the Institute for Clinical Evaluative Sciences in Toronto, Ont; was an Assistant Professor in the Faculty of Medicine at the University of Toronto at the time of the study; is Chief Executive Officer of the Health Quality Council in Saskatoon, Sask; and is an Adjunct Professor in the College of Medicine at the University of Saskatchewan in Saskatoon.
Ms Degani was a research coordinator at the Institute for Clinical Evaluative Sciences at the time of the study.
Dr Crichton is Program Director of the Northeastern Ontario Family Medicine program in Sudbury and is an Assistant Professor at the University of Ottawa in Ontario.
Dr Pong is Research Director of the Centre for Rural and Northern Health Research and is an Adjunct Professor at Laurentian University in Sudbury.
Dr Rourke was Director of the Southwestern Ontario Rural Medicine Unit in the Faculty of Medicine and Dentistry at the University of Western Ontario in London at the time of this study and is now Dean of the Faculty of Medicine at Memorial University of Newfoundland in St John’s.
Dr Goertzen was Program Director for the Family Medicine North program in the Northwest Ontario Medical Programme in Thunder Bay, Ont, at the time of the study and is now an Associate Clinical Professor in the Faculty of Health Sciences at McMaster University in Hamilton, Ont.
Dr McCready is Chair of the Northwestern Ontario Medical Programme and is now an Associate Professor at McMaster University.
References
- 1.Ontario Ministry of Health and Long-Term Care. Underserviced area program. Toronto, Ont: Ontario Ministry of Health and Long-Term Care; 2002. [cited 2004 October 1]. Available from: http://www.health.gov.on.ca/english/providers/program/uap/uap_mn.html. [DOI] [PubMed] [Google Scholar]
- 2.Krupa LK, Chan BTB. [cited 2005 August 5];Canadian rural family medicine training programs. Growth and variation in recruitment. 2005 51:852–853. Available from: http://www.cfpc.ca/cfp/2005/jun/_pdf/vol51-jun-research-3.pdf. [PMC free article] [PubMed]
- 3.Easterbrook M, Godwin M, Wilson R, Hodgetts G, Brown G, Pong R, et al. Rural background and clinical rural rotations during medical training: effect on practice location. CMAJ. 1999;160:1159–1163. [PMC free article] [PubMed] [Google Scholar]
- 4.Carter RG. The relation between personal characteristics of physicians and practice location in Manitoba. CMAJ. 1987;136:559–563. [PMC free article] [PubMed] [Google Scholar]
- 5.Becker P, Hartz A, Cutler J. Time trends in the association of a rural or urban background with physician location. J Med Educ. 1979;54(7):544–550. doi: 10.1097/00001888-197907000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Rabinowitz HK, Diamond JJ, Markham FW, Paynter NP. Critical factors for designing programs to increase the supply and retention of rural primary care physicians. JAMA. 2001;286(9):1041–1048. doi: 10.1001/jama.286.9.1041. [DOI] [PubMed] [Google Scholar]
- 7.Fryer GE, Stine C, Vojir C, Miller M. Predictors and profiles of rural versus urban family practice. Fam Med. 1997;29(2):115–118. [PubMed] [Google Scholar]
- 8.Kassebaum DG, Szenas MA. Rural sources of medical students, and graduates’ choice of rural practice. Acad Med. 1993;68:232–236. doi: 10.1097/00001888-199303000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Brooks RG, Mardon R, Clawson A. The rural physician workforce in Florida: a survey of US- and foreign-born primary care physicians. J Rural Health. 2003;19(4):484–491. doi: 10.1111/j.1748-0361.2003.tb00586.x. [DOI] [PubMed] [Google Scholar]
- 10.Wilkinson D, Beilby JJ, Thompson DJ, Laven GA, Chamberlain NL, Laurence CO. Associations between rural background and where South Australian general practitioners work. Med J Aust. 2000;173(3):137–140. doi: 10.5694/j.1326-5377.2000.tb125568.x. [DOI] [PubMed] [Google Scholar]
- 11.Laven GA, Beilby JJ, Wilkinson D, McElroy HJ. Factors associated with rural practice among Australian-trained general practitioners. Med J Aust. 2003;179(2):75–79. doi: 10.5694/j.1326-5377.2003.tb05439.x. [DOI] [PubMed] [Google Scholar]
- 12.Strasser R. Training for rural practice: lessons from Australia. Can Fam Physician. 2001;47:2196. 2196-8 (Eng), 2203-5 (Fr) [PMC free article] [PubMed] [Google Scholar]
- 13.Rabinowitz HK, Diamond JJ, Markham FW, Hazelwood CE. A program to increase the number of family physicians in rural and underserved areas: impact after 22 years. JAMA. 1999;281(3):255–260. doi: 10.1001/jama.281.3.255. [DOI] [PubMed] [Google Scholar]
- 14.Acosta DA. Impact of rural training on physician work force: the role of postresidency education. J Rural Health. 2000;16:254–261. doi: 10.1111/j.1748-0361.2000.tb00469.x. [DOI] [PubMed] [Google Scholar]
- 15.Rosenthal TC, McGuigan MH, Anderson G. Rural residency tracks in family practice: graduate outcomes. Fam Med. 2000;32(3):174–177. [PubMed] [Google Scholar]
- 16.Steinwald B, Steinwald C. The effect of preceptorship and rural training programs on physicians’ practice location decisions. Med Care. 1975;13(3):219–229. doi: 10.1097/00005650-197503000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Szafran O, Crutcher RA, Chaytors RG. Location of family medicine graduates’ practices. What factors influence Albertans’ choices? Can Fam Physician. 2001;47:2279–2285. [PMC free article] [PubMed] [Google Scholar]
- 18.Sempowski IP. Effectiveness of financial incentives in exchange for rural and underserviced area return-of-service commitments: systematic review of the literature. Can J Rural Med. 2004;9(2):82–88. [PubMed] [Google Scholar]
- 19.Dhalla IA, Kwong JC, Streiner DL, Baddour RE, Waddell AE, Johnson IL. Characteristics of first-year students in Canadian medical schools. CMAJ. 2002;166:1029–1035. [PMC free article] [PubMed] [Google Scholar]