Abstract
OBJECTIVE
To determine whether having cesarean section capability in an isolated rural community makes a difference in adverse maternal or perinatal outcomes.
DESIGN
Retrospective study comparing population-based obstetric outcomes of two rural remote hospitals in northwestern British Columbia. One hospital had cesarean section capability; one did not.
SETTING
Bella Coola General Hospital (with cesarean section capability) in Bella Coola Valley (BCV) and Queen Charlotte Islands General Hospital (without cesarean section capability) in Queen Charlotte City (QCC).
PARTICIPANTS
Women who carried pregnancies beyond 20 weeks’ gestation and who gave birth between January 1, 1986, and December 31, 2000.
INTERVENTIONS
British Columbia Vital Statistics Agency data was used to compare obstetric outcomes in the two communities. A chart audit of local births at BCV and QCC was done to validate the vital statistics data.
MAIN OUTCOME MEASURES
Perinatal death, newborn transfer to a tertiary care facility, birth weight, gestational age at delivery, mode of delivery, and Apgar score.
RESULTS
The rate of preterm deliveries in QCC was higher (relative risk 1.41, 95% confidence interval 1.00 to 1.99; P = .047) than the rate in BCV. Otherwise, there were no differences in adverse maternal or perinatal outcomes in the two populations. In BCV, 69.8% of women delivered locally compared with 50.2% of women in the southern Queen Charlotte Islands (P < .001).
CONCLUSION
Having local cesarean section capability is associated with a greater proportion of local deliveries and a lower rate of preterm deliveries.
Abstract
OBJECTIF
Déterminer si la capacité de procéder à des césariennes dans une collectivité rurale isolée peut influencer les issues défavorables chez la mère ou le nouveau-né.
TYPE D’ÉTUDE
Une étude rétrospective comparant les résultats obstétricaux en fonction de la population dans deux hôpitaux ruraux éloignés, au nord-ouest de la Colombie-Britannique. On pratiquait des césariennes dans l’un des hôpitaux et dans l’autre, cette capacité n’existait pas.
CONTEXTE
L’Hôpital Général de Bella Coola (où s’effectuent des césariennes) dans la vallée de Bella Coola (BCV) et l’Hôpital Général de Queen Charlotte Islands (dépourvu de capacité de réaliser des césariennes) dans la ville de Queen Charlotte (QCC).
PARTICIPANTS
Des femmes qui ont vécu une grossesse de plus de 20 semaines de gestation et ont donné naissance entre le 1er janvier 1986 et le 31 décembre 2000.
INTERVENTIONS
On s’est servi des données du Bureau de l’état civil de la Colombie-Britannique pour comparer les résultats obstétricaux dans deux collectivités. On a procédé à une vérification des dossiers locaux des naissances au BCV et au QCC pour valider les données du Bureau de l’état civil.
PRINCIPAUX POINTS À L’ÉTUDE
Le décès périnatal, le transfert du nouveau-né dans un centre de soins tertiaires, le poids à la naissance, l’âge gestationnel à la naissance, le mode d’accouchement et le score Apgar.
RÉSULTATS
Le taux d’accouchements prématurés au QCC était plus élevé (risque relatif de 1,41, avec intervalle de confiance à 95% de 1,00 à 1,99; P = ,047) que le taux observé au BCV. Autrement, il n’y avait pas de différence dans les résultats défavorables chez la mère ou le nouveau-né dans les deux populations. Au BCV, 69,8% des femmes avaient un accouchement localement par rapport à 50,2% des femmes au sud des îles Queen Charlotte (P <,001).
CONCLUSION
La capacité d’effectuer des césariennes est associée à une plus forte proportion d’accouchements locaux et à un taux moins élevé d’accouchements prématurés.
EDITOR’S KEY POINTS.
This study compared the obstetric and perinatal outcomes of two rural hospitals in British Columbia, Bella Coola Valley (BCV), which had local cesarean section capability, and Queen Charlotte City (QCC), which did not.
The two communities were similar in population size and rural isolation, although BCV had a higher proportion of aboriginal people in its population.
As expected with its cesarean section capability, BCV delivered more women locally, about 70% compared with about 50% in QCC. There were no differences between the two sites in cesarean section rates, instrument deliveries, adverse perinatal outcomes, or perinatal mortality.
The only difference in outcomes was a higher preterm delivery rate in QCC of 8.8% compared with 6.2% in BCV. This held after adjustment for differences in aboriginal population.
POINTS DE REPÈRE DU RÉDACTEUR.
Cette étude comparait les résultats obstétricaux et périnataux dans deux hôpitaux ruraux de la Colombie-Britannique: dans la vallée de Bella Coola (BCV), où on procède localement à des césariennes, et dans la ville de Queen Charlotte (QCC), où cette capacité est absente.
Les deux communautés comptaient une population semblable au chapitre du nombre et de l’isolement rural, quoiqu’il y ait eu une plus forte proportion d’autochtones au BCV.
Comme on pouvait s’y attendre compte tenu de sa capacité d’effectuer des césariennes, le nombre d’accouchements locaux au BCV était plus élevé, soit environ 70% par rapport à environ 50% au QCC. Il n’y avait pas de différence entre les deux centres sur les plans du taux de césariennes, des accouchements avec instruments, des résultats périnataux indésirables ou de la mortalité périnatale.
Les seules distinctions dans les résultats se situaient dans le plus fort taux d’accouchements prématurés au QCC, soit 8,8% par rapport à 6,2% au BCV. Cette tendance se maintenait même après des ajustements en fonction des différences dans la population autochtone.
About 30% of Canada’s people live in communities of less than 10 000 people.1 There was a time, not that long ago, when Canadian women living in rural communities were confident that they would receive maternity care and deliver their babies within their own communities. Physicians working in these communities felt they had an obligation to provide obstetric services. A Joint Position Paper on Rural Maternity Care affirms that “every woman in Canada who resides in a rural community should be able to obtain high-quality maternity care as close to home as possible.”2 Across Canada, however, the practice of obstetrics in rural communities is undergoing profound change.3,4 Two surveys of rural community hospitals in northern Ontario revealed that the number of hospitals no longer offering obstetric care increased 500%, from three hospitals in 1981 to 15 hospitals in 1997, and that overall, anesthesia, epidural, and cesarean section services were less available.5,6
In 1984, 56.5% of Canada’s family physicians provided maternity services in their communities.7 This percentage declined to 37.1% by 1994 and to 20% by 1997.8,9 In British Columbia, the numbers are a little better as, in 1997, 36% of family physicians were still providing intrapartum care.9 Factors contributing to the dramatic decline in numbers of family physicians providing maternity care include cost of liability insurance, fear of litigation, poor remuneration, occupational stress, lifestyle choices, lack of confidence, and lack of professional support.7,10-12
In 1995, there were 576 hospitals in Canada providing maternity care; 126 of them did not perform cesarean sections. Among the hospitals that offered cesarean sections, 40% carried out fewer than 20 each year. With so few, it would be unrealistic to expect specialists to provide them.9,13 In British Columbia in 1996, 22 hospitals delivering fewer than 250 babies annually had no on-site cesarean section capability.14
There is evidence that small rural maternity services, when adequately supported, can safely provide care to rural women.15-18 Contradicting these findings is a recent study from Norway that examined neonatal mortality in geographic areas served by various sizes of maternity units from 1967 to 1996 and found statistically significant small increases in risk of neonatal death in the smaller maternity units.19
There is also some evidence to support the safety of rural maternity units without on-site access to cesarean sections. Population-based retrospective cohort studies in New Mexico and the Queen Charlotte Islands showed that perinatal outcomes were comparable to national outcomes, and chart review of adverse outcomes found no cases where local surgical access would have made an apparent difference.20,21 In these two studies, population-based rates of local birth were 65% and 67%, intrapartum transfer rates were 9.5% and 12%, and deliveries elsewhere were 25.6 and 21%, respectively.
Loss of local maternity services can lead to adverse outcomes for newborns. Larimore and Davis22 looked at the association between availability of maternity services and perinatal outcomes in rural Florida. Results of their study showed a noticeable increase in infant mortality in association with fewer rural maternity caregivers. A study by Nesbitt et al,23 in which access to obstetric care and birth outcomes were examined in rural areas of Washington State, found a direct association between increased rates of non-local delivery and adverse health outcomes among newborns. Communities were grouped based on rate of local hospital deliveries and were given the designations high outflow (more than one third of deliveries in local hospital) and low outflow (more than two thirds of deliveries in local hospital). Compared with low-outflow communities, high-outflow communities had 50% higher rates of prematurity, and women in them were 67% more likely to experience birth-associated complications. Also, average newborn health care costs were double those of low-outflow communities.
The objective of this study was to compare maternal and perinatal outcomes in two similar, isolated, rural coastal communities in British Columbia, one with and one without local cesarean section capability. Outcomes were compared over 15 years, from 1986 to 2000.
METHODS
Study sites
Bella Coola Valley (BCV) and Queen Charlotte City (QCC) are similar in terms of population size, Northern and Isolation Allowance program designation, type of hospital, and availability of local obstetric services (Figure 1).24,25 Bella Coola Valley differed from QCC in having a slightly greater aboriginal population (40% vs 29%) and in having cesarean section capability throughout most of the study period. The referral hospital closest to BCV is more than 450 km away by road to Williams Lake or a 2-hour flight away in Vancouver. Bella Coola Valley is served by three physicians at any given time.26 Queen Charlotte City is located 150 km off the northwest coast of British Columbia and serves a population of approximately 2700. Queen Charlotte Island General Hospital has 21 beds and is staffed by three family practitioners who offer obstetric services but not cesarean section deliveries. The referral centre with surgical capability closest to QCC is a 6-hour ferry ride or a 2-hour float plane trip away in Prince Rupert. The nearest centre with obstetricians and pediatricians is a 4-hour flight away in Vancouver. For both communities, inclement weather can prevent transport to a larger centre or at least make it very difficult.
Figure 1.
Location of Queen Charlotte City and Bella Coola Valley within British Columbia
Rural remoteness was identified by Northern and Isolation Allowance designation, a rural index score developed by the British Columbia Medical Services Plan.25
Study population
The populations of interest for both communities were women who carried pregnancies beyond 20 weeks’ gestation and who gave birth between January 1, 1986, and December 31, 2000. Maternal outcomes were recorded for mothers’ place of residence rather than place of delivery to ensure that all births, local and non-local, were included. Our study population included women who delivered in their communities, women who were transferred while in labour as a result of unforeseen emergencies, and women who chose to deliver in larger centres.
Data collection
Postal codes corresponding to each hospital’s local health area (defined as the hospital’s catchment area) were obtained from Canada Post and forwarded to the BC Vital Statistics Agency in Victoria.27 The agency then provided birth data for the two communities and identified mothers as aboriginal or nonaboriginal based on linkages with the Federal Indian Registry and the BC Medical Services Plan. Descriptive data related to maternal identity were removed to maintain anonymity. Information collected included maternal age, First Nation status, gravidity, parity, date of delivery, gestational age at delivery, mode of delivery, birth weight, Apgar score, labour outcomes, procedural interventions, and delivery outcomes.
Participants were then categorized according to location of delivery. Women were classified as having a local delivery if their residential postal codes were within the hospital catchment area and they delivered at the catchment hospital. Women were classified as non-local deliveries if they were admitted to their local hospitals in labour, but were transferred to a larger centre for delivery, or if they delivered outside their rural communities by choice or on the advice of their physicians.
Charts of women who had had local births were audited at the BCV and QCC hospitals to validate the statistics data. When deliveries occurred locally and we found discrepancies with the BC Agency’s data, we assumed that the local data were correct.
Data analysis
Data were tabulated and analyzed using the Statistical Package for the Social Sciences software.28 Descriptive statistics were used to compare the two communities with respect to sociodemographic factors and health services. Differences in outcomes between the two communities and differences between aboriginal and non-aboriginal groups were evaluated using the Pearson chi-square test. Statistically significant results were indicated with a significance level of P ≤ .05 for each outcome measure. A stratified analysis was used to explore potential differences between aboriginal and non-aboriginal birth outcomes.
Ethics approval for this project was granted before the start of data collection by the University of British Columbia’s Clinical Research Ethics Board.
RESULTS
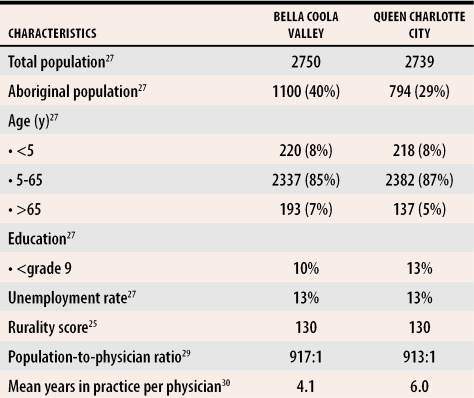
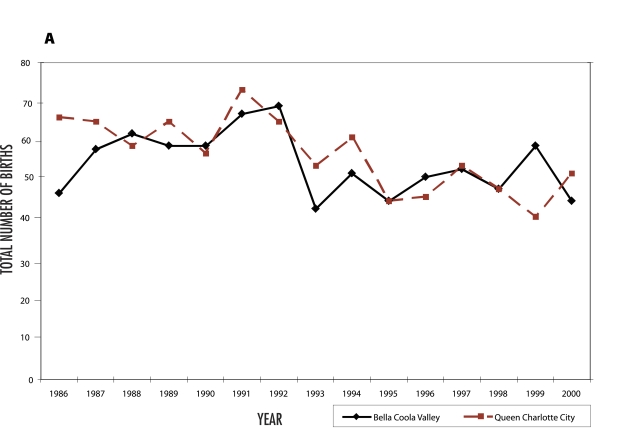
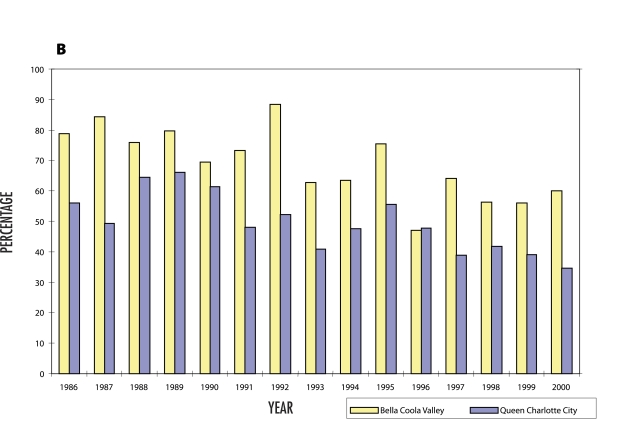
Table 125,27,29,30 demonstrates the remarkable similarity of these two rural populations. Annual number of births and proportion of local births for the two communities are shown in Figure 2. Similar trends toward decreasing numbers of births overall and decreasing proportion of local births are reported for both communities. Overall, significantly more women in BCV delivered locally throughout the 15-year period (69.8% vs 50.2%) (P < .001). No maternal deaths were reported in either population.
Table 1. Characteristics of Bella Coola Valley and Queen Charlotte City.
Differences between the two sites were non-significant for all characteristics.
Figure 2. Births in Queen Charlotte City and Bella Coola Valley, 1986-2000.
A) Total number of births; B) Percentage of births delivered locally.
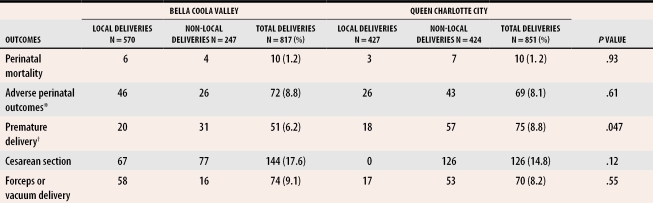
Table 231 summarizes the obstetric outcomes of women delivering in the two communities. More women at QCC had premature deliveries during the study period even though BCV had a higher proportion of aboriginal women. There were no other differences between BCV and QCC in terms of population-based rates of cesarean section, instrumental vaginal delivery, adverse perinatal outcomes, or perinatal mortality.
Table 2.
Obstetric outcomes of women in Bella Coola Valley and Queen Charlotte City, 1986-2000
*Perinatal death, birth weight <2500g, Apgar score <7 at 5 minutes, newborn transfer to secondary or tertiary care facility.31
†Rate of premature delivery in Queen Charlotte City was 41% higher during the study period (relative risk 1.41, 95% confidence interval 1.00 to 1.99).
Cesarean sections, epidural anesthesia, and vaginal births after cesarean section were done locally for certain women from BCV but not for women from QCC. Comparing local births only, there was no difference between the two hospitals in rates of episiotomy for vaginal delivery, premature delivery, perinatal mortality, or adverse perinatal outcomes.
Stratified analysis showed that ethnicity did not explain the difference in rates of premature delivery between the two communities. This secondary analysis was based on data collected only between January 1, 1991, and December 31, 2000.
DISCUSSION
This study compares two remarkably similar, small, isolated rural populations over 15 years. Each community had a small hospital maternity service. The BCV service had cesarean section capability; the QCC service did not. Perinatal mortality rates for both populations seem reasonable and are consistent with cumulative provincial rates over the same period (the BC perinatal mortality rate between 1986 and 2000 was 10.0%, 95% confidence interval 9.8 to 10.2).27 In British Columbia, the perinatal mortality rate is calculated by adding stillbirths of greater than 22 weeks’ gestation to neonatal deaths at less than 7 days old.
More women from the QCC population had preterm deliveries. This is consistent with the findings by Nesbitt and colleagues of increased prematurity associated with increased outflow from rural communities.23 Lack of local cesarean section capability means increased outflow. Overall, over the 15 years, almost 20% more women were able to remain in their home communities when local operative delivery was available. This summary statistic underreports the trend toward decreasing local access to rural maternity services reported by Rourke5 and Hutten-Czapski.12 In 1986, the BCV and QCC hospitals were able to deliver 78% and 55% of local women, respectively. By 2000, these proportions had dropped to 61% and 35%. Nesbitt and colleagues went on to suggest that high-outflow communities were likely to close their maternity services.23 This, in fact, occurred in 2000 when the QCC/Haida Gwaii community Health Council announced that local birth on the islands was no longer recommended due to the inability to meet standards for safe care. To date, this proclamation has not been rescinded, although births still occasionally take place on the islands as local resources allow. In BCV in recent years, it has become more difficult to maintain cesarean section capability year-round, and patients are being told that their community hospital might not have cesarean section capability when it is time to deliver.
Strengths of this study are the clear definition of population catchments enabled by the geography of coastal British Columbia and the merging of data from the provincial vital statistics database and the local hospitals’ medical records to provide a comprehensive perspective on the birthing population. In addition, the sociodemographic characteristics of both isolated, rural communities were comparable, and both communities had stable populations of salaried care providers during most of the study period. The hospitals were also similar with respect to services offered except for the striking difference that the BCV hospital provided local operative deliveries.
Limitations
The main limitation of this study is that the small populations make outcome measures, such as perinatal mortality rates, with consequently large confidence limits an approximation at best. Other limitations that challenge the generalizability of our findings are that the two communities are coastal and have large proportions of aboriginal people and salaried (rather than fee-for-service) physicians. The 15-year span encompasses several political reorganizations of health services in British Columbia and changing professional situations. We were unfortunately unable to link individual women’s outcomes with their socioeconomic status or educational background. It would follow logically, though, that the most disadvantaged women would be the least able to cope with the stress of not having local access to services.
There is an urgent need for a study that examines a large number of rural hospital population catchments over a shorter period to more clearly explore the association between hospital services and birth outcomes. Further research is also needed to understand why Canadian rural maternity services are eroding so dramatically in the face of what seems to be evidence justifying their existence. We need to understand more about the experience of rural women who no longer have access to local maternity services and the comparative health outcomes and dollar costs of maintaining or closing these services. This knowledge will inform our rural maternity health policy so we can plan appropriately.
Conclusion
Results of our study show that a rural maternity service with cesarean section capability in a small coastal BC community serves a larger proportion of the local population and is associated with significantly fewer premature deliveries. If these findings are replicated in larger studies, health service planners need to consider how to develop and maintain surgical services in rural and remote areas.
Acknowledgments
We thank the staff at the Bella Coola Medical Clinic, the Queen Charlotte Islands General Hospital, and the Queen Charlotte City Medical Clinic who assisted us in identifying and collecting prenatal lists, admission records, and medical records.
Biography
Ms Lynch is an instructor for the Nursing Program in Prince George, BC. Drs Thommasen and Anderson teach in the Department of Family Practice at the University of British Columbia in Vancouver. Dr Grzybowski is Director of Research in the Department of Family Practice at the University of British Columbia.
Footnotes
Competing interests: None declared
References
- 1.Statistics Canada. A national overview. Table 17. Ottawa, Ont: Statistics Canada; 1997. [Google Scholar]
- 2.Iglesias S, Grzybowski S, Klein MC, Gagne GP, Lalonde A. Rural obstetrics. Joint position paper on rural maternity care. Joint Working Group of the Society of Rural Physicians of Canada (SRPC), the Maternity Care Committee of the College of Family Physicians of Canada (CFPC), and the Society of Obstetricians and Gynaecologists of Canada (SOGC). Can Fam Physician. 1998;44:831–843. [PMC free article] [PubMed] [Google Scholar]
- 3.McIlwain R, Smith S. Obstetrics in a small isolated community: the cesarean section dilemma. Can J Rural Med. 2000;5(4):221–223. [Google Scholar]
- 4.Society of Obstetricians and Gynaecologists of Canada. SOGC policy statement. Obstetrical crisis in Canada. J SOGC. pp. 1161–1168.
- 5.Rourke JT. Trends in small hospital obstetric services in Ontario. Can Fam Physician. 1998;44:2117–2124. [PMC free article] [PubMed] [Google Scholar]
- 6.Hutten-Czapski PA. Decline of obstetrical services in northern Ontario. Can J Rural Med. 1999;4(2):72–76. [Google Scholar]
- 7.Klein M, Reynolds JL, Boucher F, Malus M, Rosenberg E. Obstetrical practice and training in Canadian family medicine: conserving an endangered species. Can Fam Physician. 1984;30:2093–2099. [PMC free article] [PubMed] [Google Scholar]
- 8.Buckle D. Obstetrical practice after a family medicine residency. Can Fam Physician. 1994;40:261–268. [PMC free article] [PubMed] [Google Scholar]
- 9.College of Family Physicians of Canada. The Janus Project. National Family Physician Survey—summary report. Mississauga, Ont: College of Family Physicians of Canada; 1998. [cited 2005 June 24]. Available at: http://www.cfpc.ca/English/cfpc/research/janus%20project/default.asp?.s=1. [Google Scholar]
- 10.Hutten-Czapski P, Iglesias S. Position paper on training for family practitioners in cesarean section and other advanced maternity care skills. Mississauga, Ont: College of Family Physicians of Canada; 1998. [cited 2005 June 24]. Available at: http://www.srpc.ca/librarydocs/cxtrainingdraft.html. [Google Scholar]
- 11.Levitt C, Kaczorowski J. Provision of intrapartum care by GP/FPs in Canada: an update. CMAJ. 1999;160:815–816. [PMC free article] [PubMed] [Google Scholar]
- 12.Shapiro JL. Satisfaction with obstetric care. Patient survey in a family practice shared-call group. Can Fam Physician. 1999;45:651–657. [PMC free article] [PubMed] [Google Scholar]
- 13.Levitt C, Hanvey L, Avard D, Chance G, Kaczorowski J. Survey of routine maternity care and practices in Canadian hospitals. Ottawa, Ont: Health Canada and Canadian Institute of Child Health; 1995. [Google Scholar]
- 14.British Columbia Reproductive Care Program. 1996 Report. Triannual hospital perinatal survey and nursing skills and competency survey. Vancouver, BC: British Columbia Reproductive Care Program; 1997. [Google Scholar]
- 15.Rosenblatt RA, Reinken J, Shoemack P. Is obstetrics safe in small hospitals? Evidence from New Zealand’s regionalized perinatal system. Lancet. 1985;2(8452):429–432. doi: 10.1016/s0140-6736(85)92747-3. [DOI] [PubMed] [Google Scholar]
- 16.Black DP, Fyfe IM. The safety of obstetric services in small communities in Northern Ontario. CMAJ. 1984;130:571–576. [PMC free article] [PubMed] [Google Scholar]
- 17.Viisainen K, Gissler M, Hemminki E. Birth outcomes by level of obstetric care in Finland: a catchment area based analysis. J Epidemiol Community Health. 1994;48(4):400–405. doi: 10.1136/jech.48.4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peddle LJ, Brown H, Buckley J, Dixon W, Kaye J, Muise M, et al. Voluntary regionalization and associated trends in perinatal care: the Nova Scotia Reproductive Care Program. Am J Obstet Gynecol. 1983;145(2):170–176. doi: 10.1016/0002-9378(83)90485-4. [DOI] [PubMed] [Google Scholar]
- 19.Moster D, Terje Lie R, Markestad T. Neonatal mortality rates in communities with small maternity units compared with those having larger maternity units. Br J Obstet Gynaecol. 2001;108:904–909. doi: 10.1111/j.1471-0528.2001.00207.x. [DOI] [PubMed] [Google Scholar]
- 20.Leeman L, Leeman R. Do all hospitals need cesarean delivery capability? An outcomes study of maternity care in a rural hospital without on-site cesarean capability. J Fam Pract. 2002;51(2):129–134. [PubMed] [Google Scholar]
- 21.Grzybowski S, Cadesky A, Hogg W. Rural obstetrics: a 5-year prospective study of the outcomes of all pregnancies in a remote northern community. CMAJ. 1991;144(8):987–994. [PMC free article] [PubMed] [Google Scholar]
- 22.Larimore WL, Davis A. Relation of infant mortality to the availability of maternity care in rural Florida. J Am Board Fam Pract. 1995;8:392–399. [PubMed] [Google Scholar]
- 23.Nesbitt TS, Connell FA, Hart LG, Rosenblatt RA. Access to obstetric care in rural areas: effect on birth outcomes. Am J Public Health. 1990;80(7):814–818. doi: 10.2105/ajph.80.7.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.British Columbia Vital Statistics Agency. 1996 British Columbia census. Victoria, BC: Government of British Columbia; 1996. [Google Scholar]
- 25.British Columbia Medical Association and BC Ministry of Health. Northern and Isolation Allowance (NIA) program. Program eligibility criteria. Victoria, BC: British Columbia Medical Association and BC Ministry of Health; 2000. [Google Scholar]
- 26.British Columbia Ministry of Health. Geographic units of analysis of British Columbia, local health area and health region map. Victoria BC: Government of British Columbia; 1997. [Google Scholar]
- 27.British Columbia Vital Statistics Agency. Selected vital statistics and health status indicators: 127th annual report 1998. Table 4. Trends of infant mortality British Columbia and Canada, 1965-1998. Victoria, BC: British Columbia Vital Statistics Agency; 1998. [cited 2005 June 24]. Available at: http://www.vs.gov.bc.ca/stats/annual/1998/tab04.html. [Google Scholar]
- 28.SPSS Inc. Statistical Package for the Social Sciences, version 10.0. Chicago, Ill: SPSS Inc; 1999. [Google Scholar]
- 29.Thommasen HV, Grzybowski S, Sun R. Physician population ratios in British Columbia. Can J Rural Med. 2001;4(3):139–145. [Google Scholar]
- 30.Thommasen HV, Thommasen AT, Grzybowski S. General practitioner to population ratios and long-term family physicians retention in British Columbia health regions. Can J Rural Med. 2001;6(2):115–122. [Google Scholar]
- 31.LeFevre M, Williamson HA, Hector M., Jr Obstetric risk assessment in rural practice. J Fam Pract. 1989;28(6):691–695. Discussion 1989;28(6):695-6. [PubMed] [Google Scholar]