Abstract
PROBLEM BEING ADDRESSED
Colorectal cancer (CRC) is a substantial cause of death and morbidity in Canada. Endoscopy screening by colonoscopy has been recommended, but widespread implementation is impossible because it is difficult to obtain, especially in rural areas.
OBJECTIVE OF PROGRAM
To screen for CRC safely and effectively using colonoscopy performed by non-specialist endoscopists in rural areas.
PROGRAM DESCRIPTION
Health providers and community organizations were informed about the screening program. Patients between the ages of 50 and 75 and those at high risk of CRC based on family history were screened. Measures of safety and effectiveness were monitored. In 2 years of screening, one of 152 patients was found to have CRC, and 23.7% had adenomatous polyps. There were no complications. Rates of CRC and adenoma detection and cecal intubation were similar to rates found in other screening studies.
CONCLUSION
It was not difficult to design and implement a CRC screening program in our small rural community. Colonoscopies performed by family physicians have been effective, and there have been no serious complications.
Abstract
QUESTION À L’ÉTUDE
Le cancer colorectal (CCR) est une importante cause de décès et de morbidité au Canada. La colonoscopie recommandée comme dépistage n’est toutefois pas réalisable sur une grande échelle à cause du peu de disponibilité de cet examen, notamment en régions rurales.
OBJECTIF DU PROGRAMME
Faire le dépistage du CCR de façon sûre et efficace en faisant faire les colonoscopies par des omnipraticiens dans les régions rurales.
DESCRIPTION DU PROGRAMME
Le personnel soignant et les organismes communautaires ont été informés du programme de dépistage. Le dépistage visait les patients de 50 à 75 ans et ceux jugés à risque élevé de CCR d’après l’histoire familiale. Les aspects de sécurité et d’efficacité ont fait l’objet de surveillance. Sur les 152 patients examinés en deux années de dépistage, on a trouvé un cas de CCR et des polypes adénomateux dans une proportion de 23,7%. Aucune complication n’est survenue. Les proportions de CCR et d’adénomes détectés et d’intubations intra-cæcales étaient semblables a celles observées dans d’autres études de dépistage.
CONCLUSION
La conception et la mise en place d’un programme de dépistage du CCR dans notre petite collectivité rurale se sont avérées plutôt faciles. Les colonoscopies ont été effectuées par des médecins de famille de façon efficace et sans complication importante.
EDITOR’S KEY POINTS.
Although screening for colorectal cancer is recommended, widespread access to it is poor, especially in rural communities because there are few endoscopists.
The rural community of Wawa, Ont, addressed the problem by designing a program to screen all eligible adults over 10 years. The program was widely advertised in the media and by health practitioners.
Two family doctors trained to do colonoscopies, which were carried out in hospital. Small increases in staff and operating room time were required.
Over 2 years, 152 screening colonoscopies were carried out. Polyps were detected in 24% of cases and cancer found in one case. There were no complications. These figures are consistent with those at specialist facilities.
POINTS DE REPÈRE DU RÉDACTEUR.
Le dépistage du cancer colorectal est recommandé, mais il n’est pas facilement accessible, notamment en milieu rural, à cause de la pénurie d’endoscopistes.
Dans la communauté rurale de Wawa (Ont.) on a résolu le problème en instaurant un programme de dépistage visant tous les adultes éligibles sur une période de 10 ans. Ce programme a été largement publicisé grâce aux médias et au personnel soignant.
Deux médecins de famille ont appris à faire des colonoscopies, lesquelles ont été faites à l’hôpital. Le programme n’a exigé qu’une légère augmentation en personnel et en temps de salle d’opération.
En deux ans, 152 colonoscopies de dépistage ont été effectuées. Des polypes ont été détectés dans 24% des cas et il y a eu un cas de cancer. Il n’y a pas eu de complications. Ces chiffres concordent avec ceux obtenus dans les milieux spécialisés.
Colorectal cancer (CRC) is the second leading cause of death from cancer in Canada.1 Our community carries a high burden of illness among patients who are diagnosed with CRC but survive to require lifelong treatment for the disease and its complications. Screening for CRC has been shown to result in decreased mortality,2-5 and colonoscopic screening offers the additional advantage of preventing CRC by removing polyps with malignant potential.6,7
In 1999, the Ontario Expert Panel on Colorectal Cancer recommended that, among other things, a screening program for CRC be introduced in the province and that the program expand to use colonoscopy as the primary screening method when resources are available.8 Screening using the fecal occult blood test had been available in our community for many years, but we believed that screening with colonoscopy was superior.4,9,10 We considered developing a colonoscopy screening program in which colonoscopies would be performed by non-specialists in our community.
The main question for us was risk to patients. Risk of perforation has been quoted as being as high as one in 1000 procedures, although Rex et al in 2000 suggested, “the rate of perforation in diagnostic colonoscopy is uncertain but is of the order of one in several thousand colonoscopies.”9 The annual incidence of CRC in Ontario increases with increasing age from about 50 per 100 000 at age 50 to about 300 per 100 000 at age 75.8. Based on a review of colonoscopy studies, we calculated that if we screened 1000 patients over 10 years, we would uncover approximately seven asymptomatic cases of CRC and would cause less than one perforation.12
We decided to initiate a program with a goal of safely screening the eligible local population within 10 years. A 10-year interval between screening colonoscopies is currently recommended for average-risk patients.8,10 Priorities in design of the program included the following.
We had to be able to demonstrate the effectiveness of the procedure.
We needed a simple, effective way to recruit patients.
We had to avoid straining hospital resources.
Because the probability of finding a cancer in a population of average-risk patients is about 1%, the risk of serious complications should also be very low for the program to be beneficial overall; therefore, monitoring the effectiveness and safety of the program was essential.
Program description
Setting.
Patients residing in Wawa, Ont, or surrounding communities (total population about 6000) between the ages of 50 and 75 years, or with a family history of colon cancer and younger than 50 years, were eligible to participate in the screening program. Those whose life expectancy physicians estimated to be less than 10 years were excluded. Patients with a clinical indication for colonoscopy, or who had had colonoscopy within the last 10 years, were also excluded. Screening colonoscopy was done in the operating room, with the usual operating staff, on days that were already available for colonoscopy or other surgical procedures.
Patient selection.
To avoid a large backlog of patients awaiting colonoscopy, we decided on a stepwise approach to recruitment. The screening program was publicized in a series of articles in the Wawa newspaper during the first month of the program. To broaden access to the program, patients were allowed to book the procedure directly, without referral from a health care provider. During the initial year, providers (five family physicians and one nurse practitioner) offered screening colonoscopy to some eligible patients during office visits when it occurred to them to do so after our initial educational presentation. No additional measures were implemented to encourage them to recommend screening. In the second year, clerical staff placed reminders to offer CRC screening in the charts of patients older than 50 who presented for appointments booked for any reason at the medical centre. If enrolment is inadequate in the future, a final step will be to search the medical centre’s electronic medical records for all remaining eligible patients and to contact them directly to offer screening.
Procedure.
Colonoscopies are done in the hospital operating room, 2 days weekly. A single nurse assists during the procedure and cleans the colonoscope afterward. Informed consent is obtained. Patients give themselves the bowel preparation, Golytely, at home.
Patients have an intravenous line of normal saline running, and supplemental oxygen is administered. Cardiac rhythm and pulse oximetry are monitored continuously, and blood pressure is measured regularly. Sedative medications (usually a combination of fentanyl, midazolam, and propofol) are administered by the endoscopist or a registered nurse in the presence of the endoscopist. No anesthetist is present. Cecal intubation is confirmed by viewing the ileal papilla and seeing the colonoscope light in the right lower quadrant. If the cecum is not reached, patients are informed of other screening options. Polyps are destroyed using “hot” biopsy forceps in direct fulguration, or are removed by a wire snare and sent for histologic examination.
The endoscopist discusses the findings with patients in whom disease is found and plans for treatment or repeat colonoscopy, as required. We defined an adenomatous polyp as any polyp, of any size, with an adenomatous component but no carcinoma. Endoscopists track their colonoscopy data with database software on hand-held computers.
Evaluation.
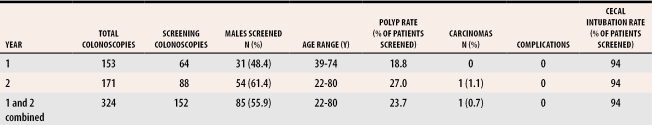
Outcomes were defined as detection of adenomatous polyps, detection of carcinoma, technical success in reaching the cecum, and complications. We defined complications as intestinal perforation, hemorrhage requiring hospital admission or transfusion, or problems related to sedation that required admission to hospital. Table 1 shows results for each year individually and combined.
Table 1.
Results of first 2 years of screening
Discussion
In this study, 23.7% (95% confidence interval [CI] 15.2% to 29.0%) of screened patients were found to have adenomas. A 1995 review of colonoscopy studies found that an average of 29% of patients considered at average risk of CRC were found to have adenomas.11 We detected one carcinoma in 152 patients (0.7%, 95% CI 0 to 2.1%). Rex reported an average rate of 0.7%, in both patients who underwent colonoscopy because of a positive family history and patients who were at average risk.11*
Before initiating the program, we had assured ourselves that the colonoscopies we were doing were meeting standards suggested in the literature. We reviewed the work of one of the authors (E.K.) who had been performing colonoscopies in our hospital for 9 years before the study. We found that, in the final years of the study, he had achieved acceptable benchmarks in safety and effectiveness.12 A second family physician (M.C.) began doing colonoscopies in Wawa in 2001 after training during residency and while in practice. Review of the results in our program indicates that measures of effectiveness have met benchmark values so far.
There were no procedural complications in the first 2 years of the program. Because reported complication rates are very low, we will not be able to conclude that our rates are as low as those reported in the literature until we have done at least 1000 colonoscopies. We are reassured, however, by the fact that if we add the colonoscopies E.K. performed before our screening program to these results, we have performed almost 1000 colonoscopies here without a perforation.
Our stepwise approach to recruiting patients served to even out the demand for screening colonoscopy, although at times the waiting list grew long. It has not been difficult to recruit patients so far, although this could change as we get further down the list of eligible patients.
The local hospital board was involved, as they provided ethical approval for a study describing the screening program. They were reassured that our goal of 100 screening colonoscopies yearly would add only two colonoscopies weekly to the load at the hospital, yet would allow screening of nearly all eligible patients over 10 years. This was not expected to strain hospital resources unduly. Oddly enough, the number of colonoscopies performed for traditional indications remained about the same as it had been in previous years. There was no indication that the program strained hospital resources or delayed other procedures. The time a physician spent performing colonoscopies, however, meant reduced time for other responsibilities.
Those designing the study agreed to review the progress of the screening program every 6 months and to complete the study in 2 years. The group plans to report on the health effects of the program after 5 years.
Our review of the literature suggests that the need for CRC screening in Canada is currently unmet. Although colonoscopy has been recommended as a screening tool, one barrier to its implementation is the inadequate number of specialist endoscopists available to screen the population at risk, especially in rural isolated communities. Although there are reports of non-specialists performing colonoscopies, an October 2004 MEDLINE search of colonoscopy screening programs for CRC found no programs in which non-specialists performed the test.
Whether we need a study to confirm that screening colonoscopy reduces morbidity and mortality from CRC better than fecal occult blood screening is debatable. But it would be interesting to see whether, on a large scale, non-specialists can safely screen for CRC using colonoscopy. We have found that training programs for non-specialists are few and far between.
Conclusion
We were able to design and implement this CRC screening program in a small centre with no great effort. Despite the limited number of patients screened, the rate of cancers and polyps detected was similar to that reported in the literature. As yet, there have been no complications as we have defined them. Non-specialists considering implementing similar programs will find they can readily monitor the effectiveness and safety of their colonoscopies.
Acknowledgments
This research was supported by a grant from the Ontario Medical Association’s CME Fund. We thank the late Dr Hui Lee for his guidance.
Biography
Drs Cotterill, Gasparelli, and Kirby are general practitioners at Lady Dunn Hospital in Wawa, Ont. Drs Gasparelli and Kirby are Associate Professors at McMaster University in Hamilton, Ont.
Footnotes
Competing interests: None declared
*Almost 4 years after starting the program, no carcinomas missed on initial screening examinations have been diagnosed.
References
- 1.National Cancer Institute of Canada. Canadian cancer statistics 2004. April 2004. Toronto, Ont: National Cancer Institute of Canada; [cited 2004 Nov 1]. Available from: http://www.ncic.cancer.ca/vgn/images/portal/cit_86751114/14/35/195991821ncic_stats2004_en.pdf. [Google Scholar]
- 2.Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–1477. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 3.Selby JV, Friedman GD, Quesenberry CP, Jr, Weiss NS. A case-control study of sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326:653–657. doi: 10.1056/NEJM199203053261001. [DOI] [PubMed] [Google Scholar]
- 4.Newcomb PA, Norfleet RG, Storer BE, Surawicz TS, Marcus PM. Screening sigmoidoscopy and colorectal cancer mortality. J Natl Cancer Inst. 1992;84:1572–1575. doi: 10.1093/jnci/84.20.1572. [DOI] [PubMed] [Google Scholar]
- 5.Towler BP, Irwig L, Glasziou P, Weller D, Kewenter J. Screening for colorectal cancer using the faecal occult blood test, Hemoccult (Cochrane Review). In: The Cochrane Library [database on disk and CD-ROM]. The Cochrane Collaboration. 2004 Issue 1. Chichester, UK: John Wiley & Sons, Ltd; [DOI] [PubMed] [Google Scholar]
- 6.Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 7.The Italian Multicentre Study Group. Citarda F, Tomaselli G, Capocaccia R, Barcherini S, Crespi M. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut. 2001;48:812–815. doi: 10.1136/gut.48.6.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ontario Expert Panel on Colorectal Cancer. Colorectal cancer screening. The final report of the Ontario Expert Panel. Toronto, Ont: Cancer Care Ontario; 1999. [Google Scholar]
- 9.Rex DK, Johnson DA, Lieberman DA, Burt RW, Sonnenberg A. Colorectal Cancer Prevention 2000: screening recommendations of the American College of Gastroenterology. Am J Gastroenterol. 2000;95:868–877. doi: 10.1111/j.1572-0241.2000.02059.x. [DOI] [PubMed] [Google Scholar]
- 10.Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale—update based on new evidence. Gastroenterology. 2003;124:544–560. doi: 10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- 11.Rex DK. Colonoscopy: a review of its yield for cancer and adenomas by indication. Am J Gastroenterol. 1995;90:353–363. [PubMed] [Google Scholar]
- 12.Kirby E. Colonoscopy procedures at a small rural hospital. Can J Rural Med. 2004;9(2):89–93. [PubMed] [Google Scholar]