Abstract
OBJECTIVE
To review the use of radiotherapy in cancer care, especially the role of radiation in palliative care.
QUALITY OF EVIDENCE
MEDLINE was searched from January 1966 to January 2004. Relevant articles evaluating indications for radiotherapy were reviewed. This paper describes use of radiotherapy based on well established current radiotherapy practices and level I and II evidence.
MAIN MESSAGE
A substantial number of patients seeing family physicians develop cancer or die of it. Despite its effectiveness, radiotherapy remains underused in management of cancer patients. Broad uses of radiotherapy in cancer care include curative treatment, palliative symptom control, and management of oncologic emergencies. Radiotherapy can be especially effective for treating common complications of cancer, including painful bone and soft tissue metastases, hemoptysis, dyspnea, dysphagia, brain metastases, and spinal cord compression.
CONCLUSION
Radiotherapy is a vital aspect of both curative and palliative cancer treatment. Understanding the basics of radiotherapy can assist family physicians in providing complete care for their cancer patients.
Abstract
OBJECTIF
Faire le point sur l’utilisation de la radiothérapie dans le traitement du cancer, notamment sur le rôle des radiations dans les soins palliatifs.
QUALITÉ DES PREUVES
On a consulté MEDLINE entre janvier 1966 et janvier 2004 et les articles traitant spécifiquement des indications de la radiothérapie ont fait l’objet d’une recension. Cet article décrit les indications de la radiothérapie en se fondant sur les pratiques actuellement reconnues pour ce type de traitement et sur des preuves de niveau I et II.
PRINCIPAL MESSAGE
Un nombre appréciable des clients des médecins de famille développent un cancer ou en meurent. Malgré son efficacité, la radiothérapie demeure sous-utilisée dans le traitement des cancéreux. Le rôle de la radiothérapie chez les cancéreux va du traitement curatif au contrôle palliatif des symptômes et au traitement des urgences oncologiques. La radiothérapie est souvent efficace pour traiter des complications usuelles du cancer, comme les douleurs osseuses, les métastases des tissus mous, les hémoptysies, la dyspnée, la dysphagie, les métastases cérébrales et la compression de la moelle épinière.
CONCLUSION
La radiothérapie est une partie intégrante du traitement du cancer, tant au point de vue curatif que palliatif. Le médecin de famille qui possède des notions élémentaires de radiothérapie devrait fournir aux cancéreux un traitement plus complet.
EDITOR’S KEY POINTS.
Radiotherapy is an important, but sometimes underused, treatment for curative, palliative, and emergency cancer care.
Family physicians should consider radiotherapy for symptom relief for patients receiving palliative care. It can help relieve pain, for example, from bone or soft tissue metastases or from brain tumours and can treat hemoptysis, dysphagia, dyspnea, or spinal cord compression.
Benefits are usually noticeable within 1 to 3 weeks and side effects are mild to moderate, with fatigue, nausea and skin or mucous membrane irritation the most common.
POINTS DE REPÈRE DU RÉDACTEUR.
La radiothérapie est un traitement important, mais parfois sous-utilisé, dans les soins curatifs, palliatifs et d’urgence du cancer.
Le médecin de famille devrait penser à la radiothérapie pour soulager les symptômes des patients qui reçoivent des soins palliatifs. Elle peut aider à soulager la douleur associée, par exemple, aux métastases des os ou des tissus mous, ou aux tumeurs cérébrales, en plus de traiter les hémoptysies, les dysphagies, la dyspnée ou les compressions de la moelle épinière.
Les effets bénéfiques sont généralement observables en 1 à 3 semaines et les effets indésirables sont légers à modérés, les plus fréquents étant la fatigue, les nausées et l’irritation de la peau ou des muqueuses.
In Canada today, approximately 40% of men and women can expect to develop cancer during their lives, and 25% of them will die of it.1 Radiotherapy is an integral part of a multidisciplinary approach to cancer care; an estimated 50% to 60% of all cancer patients could benefit from such treatment. Radiation therapy has an especially important role in palliative care.2,3
Unfortunately, many health care professionals have had little education on the value of radiotherapy and often do not consider it for treating their patients with cancer.4 A better understanding of the role of radiotherapy in cancer treatment can assist family physicians in caring for their cancer patients.5 This article briefly describes the role of radiotherapy in cancer treatment, particularly emphasizing its effectiveness for palliative care, so that family physicians will be better aware of the appropriateness of referring patients for such treatment.6
Quality of evidence
MEDLINE was searched from January 1966 to January 2004 by cross-matching the MeSH headings “radiotherapy,” “education,” and “physicians, family.” Articles reviewing the role of radiotherapy in cancer treatment were appraised. Several articles commented on the potential benefits of improving education on radiotherapy for family physicians so that they would be in a position to provide better care for their cancer patients (level II evidence). The discussion of radiotherapy in this paper is based on well established, current, published radiotherapy practices and on level I and II evidence for response rates to radiotherapy in a variety of common clinical settings.
Rationale for treatment
Radiotherapy, also called radiation therapy, uses high-energy radiation to kill tumour cells by damaging their DNA and preventing them from dividing properly. The rationale for fractionation, or dividing the total dose of radiation over time, is to allow normal tissues to repair damage and still destroy cancer cells. This is not a big issue for palliative radiotherapy, but is critical for curative treatment.
Radiotherapy focuses on treating cancer in situ without removing organs and tissues, as with surgery, and without causing the systemic side effects of chemotherapy. Selection of patients is, therefore, less restricted by existing medical conditions. Radiotherapy can be used alone or in conjunction with surgery and systemic therapies (eg, chemotherapy, hormones). The intent is either to cure with radical radiotherapy or to control symptoms with palliative radiotherapy.
Radiotherapy treatment
Three-step approach.
The first step in radiotherapy is to meet with a radiation oncologist so that an informed decision can be made regarding the overall prognosis and goals of treatment and so that patients and physicians can proceed with planning treatment. The next step is to determine the area to be treated, a process called simulation. The simulation for treatment is often done with fluoroscopy, x-ray films, or computed tomography scans.
The third step is treatment. Radiation treatments are usually given 5 days a week (Monday to Friday with no treatments on weekends) over several weeks. Radiation treatments last only minutes each day. Palliative radiotherapy usually has a much shorter course of treatment (as few as one to five treatments) and aims to provide rapid relief of symptoms. In some cancer centres, especially those with dedicated palliative radiotherapy clinics, consultation, simulation, and treatment can all be done on the same day.
Myths about radiotherapy.
The many myths regarding radiotherapy need to be dispelled. Specifically, treatment is not painful; patients do not become radioactive after treatment; and patients do not pose a danger to those around them. Radiotherapy is usually given over several minutes and is similar to having an x-ray examination. Patients need to be cooperative and able to lie still for 10 to 15 minutes. As it is a localized treatment, benefits and side effects are generally limited to the areas being treated.
Limitations of therapy.
Radiotherapy has limitations. First, there is no immediate relief of symptoms after radiation; it often takes 1 to 3 weeks for patients to notice maximum improvement. Therefore, patients with a life expectancy of less than 1 month are usually not candidates for radiotherapy. Also, except for brain metastases, radiotherapy usually does not work well if there is diffuse or extensive critical organ involvement, such as liver or lung metastases. In these situations, acute radiation toxicity can be severe and outweigh any potential benefits.
The etiology of cancer symptoms should be clearly understood before radiation therapy is given; otherwise it might be ineffective at improving symptoms. For example, a patient with lung cancer and dyspnea might not notice any improvement and could even feel worse following radiotherapy if the underlying problem is related to chronic obstructive lung disease.
Radical and adjuvant radiotherapy
Radiotherapy plays an important role in curative treatment of many cancers.3,7 It can be used alone or in conjunction with surgery, chemotherapy, or both, with the intent of completely eradicating the cancer. Radiation therapy allows for local control of the cancer with generally good cosmesis and organ preservation. The most common malignancies treated with radiotherapy include those involving the breasts, prostate, lungs, gastrointestinal tract, and skin. Radiation oncologists must balance the toxicity of radiotherapy, including its long-term complications, with the probability of cure. Many cancers can be treated successfully with radiation, and these are the ones most often subject to this type of treatment. Radiation therapy can also be used for some benign conditions, including keloids, pituitary adenomas, Graves ophthalmopathy, and arteriovenous malformations.7
Palliative radiotherapy
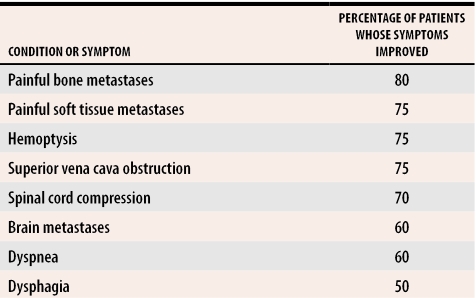
Radiotherapy can be effective at controlling symptoms and improving the quality of life of patients with advanced cancer2,8,9; 60% to 80% of all patients undergoing palliative radiotherapy experience clinically significant improvement in symptoms following treatment although it might take several weeks after treatment for full benefits to be evident. Table 18-18 gives typical rates of symptom improvement after palliative radiotherapy for some of the most common conditions for which radiotherapy is effective. Compared with radical radiotherapy, palliative radiotherapy usually occurs over a relatively short period, such as five treatments over 1 week or even a single treatment in 1 day. This is more convenient for patients and increases their compliance with treatment.10,19
Table 1.
Percentage of patients who experience improvement in symptoms following palliative radiotherapy
Palliative radiotherapy is usually straightforward to administer and requires fewer resources than radical treatment. It also has far fewer side effects, and most of those are mild and easily managed. Unfortunately, radiotherapy is still underused by health care professionals caring for patients with advanced cancer,4 despite its effectiveness in relieving pain and other symptoms and its importance in managing oncologic emergencies.8,9 Family physicians can often have an important role in identifying potentially treatable problems, but some investigations are difficult to obtain on an urgent basis and are best arranged by an oncology specialist.
Treatments for certain conditions
Spinal cord compression.
Spinal cord compression resulting from tumour growth is an oncologic emergency that should be treated within 24 hours of diagnosis. The aim of treatment is to maintain patients’ ability to walk, continence, and comfort. Most patients (95%) with spinal cord compression present with back pain and neurologic signs and symptoms including weakness, paresthesia, incontinence, spasticity, and hyperreflexia. Patients’ neurologic deficits sometimes progress rapidly, and early detection is of utmost importance. Magnetic resonance imaging is the modality of choice for this.
A radiation oncologist should be consulted on an emergency basis for spinal cord compression. Radiotherapy remains the mainstay of treatment, but some patients might require neurosurgery.8,11 The course of radiation therapy usually lasts 1 to 2 weeks. Prognosis is largely dependent on a patient’s overall condition, pretreatment ability to walk, rate of symptom progression, and the extent of the block. Most patients ambulatory at diagnosis of spinal cord compression remain ambulatory if treated promptly; only half of those who can move their legs but are not walking become ambulatory after treatment. Unfortunately, few completely paraplegic patients recover neurologic function, which highlights the importance of early diagnosis and immediate treatment.
Superior vena cava obstruction.
Superior vena cava obstruction caused by cancer also requires urgent, though not emergency, treatment. Patients usually present with neck and facial swelling, dilated neck veins, orthopnea, and shortness of breath, and sometimes progress to headaches and cerebral edema. Radiotherapy to the neck and mediastinum should be given on an urgent basis, usually within 1 to 2 weeks, depending on severity of presenting symptoms. More than 70% of patients notice improvement in symptoms.8,12 Some chemotherapy-responsive malignancies, such as lymphomas and small cell lung cancers, can also cause superior vena cava obstruction and are primarily treated with chemotherapy. It is important, therefore, to do an adequate tumour biopsy so that tumour histology can be documented.10
Bone metastasis.
Bone metastases are the most common indication for palliative radiotherapy. About 80% of patients who receive radiation therapy for bone pain experience fewer symptoms; maximum effect is noticed on average 1 to 3 weeks after treatment.2,9,13,14 Breast, prostate, and lung are common primary cancer sites for bone metastases.15 Diagnosis is usually made using bone scans and plain x-ray films, but occasionally magnetic resonance imaging or computed tomography scans are needed. Spinal cord compression needs to be ruled out if back pain is associated with neurologic signs or symptoms. For many patients, even a single treatment leads to substantially reduced pain; prolonged courses of treatment are rarely required.10,14 As there is usually a delay between radiotherapy and noticeable improvement in pain, it is important to maximize medical management of patients’ pain even before treatment starts.
Brain metastasis.
Brain metastases occur in approximately 10% to 30% of all cancer patients. Radiotherapy, in addition to steroids and occasionally surgery, can improve symptoms and prolong survival.8,9 Patients often present with symptoms such as headache, cognitive dysfunction, neurologic deficits, and seizures. Contrast-enhanced computed tomography or magnetic resonance imaging scans are used to diagnose brain metastases. A brain biopsy might be required if diagnosis is uncertain.20 High doses of steroids are often given to patients once a diagnosis is made while they wait for radiotherapy to start.
Radiotherapy, commonly given over 1 to 2 weeks to the whole brain, can improve symptoms and even prolong survival. Patients with solitary brain metastases are often considered for either surgical resection or stereotactic radiosurgery (highly focused radiotherapy) in addition to whole-brain radiation.9,10
Other symptoms.
Tumour growth can partially or completely block hollow organs, such as the esophagus, trachea, or bronchi, and radiotherapy can be helpful in reducing the obstruction.15,16 Hemoptysis and bleeding from other areas including the bladder, vagina, and rectum can also be successfully treated with palliative radiotherapy.9 Radiotherapy can help relieve many other symptoms resulting from cancer, including painful soft tissue or nodal masses and enlarging cutaneous or subcutaneous metastases.9,17,18
Side effects
Radiotherapy is generally well tolerated, and side effects are usually limited to the area being treated.6 Fatigue, however, is a common systemic side effect, but it tends to be mild and self-limiting.7 Most common side effects can be managed quite easily with simple measures: rest, adequate fluid intake, good nutrition, and proper hygiene can help minimize the acute side effects of radiation. Early local effects are felt during or shortly after radiation treatment and are usually easily treated. They resolve within 3 to 6 weeks of radiotherapy. Late local effects can occur months to years after therapy and might be permanent.
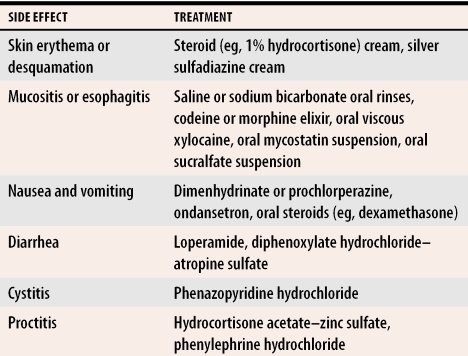
Hair loss occurs only in areas treated and is usually temporary. Skin reactions, such as erythema and desquamation, are common and often treated similarly to sunburns with topical steroids. Mucositis and esophagitis occur after radiotherapy to the head, neck, and mediastinal areas and are treated with dietary modifications, oral rinses, analgesics, antifungals, and cytoprotective agents.
Nausea and vomiting can occur several hours after radiotherapy to the brain or abdomen; antiemetics are indicated. Sometimes antiemetics are used prophylactically just before radiation to minimize the severity of symptoms. Diarrhea sometimes results from treatment to the abdomen or pelvic areas and is best managed with lots of oral fluids, dietary modifications, and common antidiarrheal medication. Proctitis from radiotherapy can be treated with sitz baths and standard anorectal therapy. Radiation cystitis often responds to increased fluid intake (including acidic drinks, such as cranberry juice) and occasionally, urinary analgesics. Medications used to treat common side effects are shown in Table 2. Serious late side effects are uncommon, but should be managed by treating radiation oncologists. These late side effects are usually not a major issue for patients receiving palliative radiotherapy.
Table 2. Treatment of common side effects of radiation.
Treatments are based on typical approaches used at the Ottawa Hospital Regional Cancer Centre in Ontario.
Conclusion
Radiotherapy has an essential role in radical and palliative management of cancer patients. Family physicians participating in care of cancer patients can help facilitate referral for radiotherapy when they encounter patients with oncologic problems or complications amenable to radiotherapy treatment.
Acknowledgments
The authors thank Ms Betty McAndrew for her secretarial expertise in completing this manuscript.
Biographies
Dr Samant is a Radiation Oncologist at the Ottawa Hospital Regional Cancer Centre and an Assistant Professor in the Faculty of Medicine at the University of Ottawa in Ontario.
Dr Gooi is a resident in radiation oncology at the University of Manitoba in Winnipeg.
Footnotes
Competing interests: None declared
References
- 1.National Cancer Institute of Canada. Canadian cancer statistics 2003. Toronto, Ont: National Cancer Institute of Canada; 2003. [Google Scholar]
- 2.Ciezki JP, Komurcu S, Macklis RM. Palliative radiotherapy. Semin Oncol. pp. 90–93. [PubMed]
- 3.Rice AM. An introduction to radiotherapy. Nurs Standard. pp. 49–56. [DOI] [PubMed]
- 4.Samant R, Malette M, Tucker T, Lightfoot N. Radiotherapy education among family physicians and residents. J Cancer Educ. pp. 134–138. [DOI] [PubMed]
- 5.Piga A, Graziano F, Zahra G, Cellerino R. Attitudes of non-oncology physicians dealing with cancer patients. A survey based on clinical scenarios in Ancona province, central Italy. Tumori. 1996;82(5):423–429. doi: 10.1177/030089169608200502. [DOI] [PubMed] [Google Scholar]
- 6.Chan SL, Kagan R, Streeter OE, Jr, Ryoo MC. Outcome of care. Complications from radiation therapy treatment. Am J Clin Oncol. 1993;16(1):81–85. [PubMed] [Google Scholar]
- 7.Tisdale BA. When to consider radiation therapy for your patient. Am Fam Physician. 1999;59(5):1177–1184. [PubMed] [Google Scholar]
- 8.Donato V, Bonfili P, Bulzonetti N, Santarelli M, Osti MF, Tombolini V, et al. Radiation therapy for oncological emergencies. Anticancer Res. 2001;21(3C):2219–2224. [PubMed] [Google Scholar]
- 9.Hoegler D. Radiotherapy for palliation of symptoms in incurable cancer. Curr Probl Cancer. 1997;21(3):129–183. doi: 10.1016/s0147-0272(97)80004-9. [DOI] [PubMed] [Google Scholar]
- 10.Ashby M. The role of radiotherapy in palliative care. J Pain Symptom Manage. 1991;6(6):380–388. doi: 10.1016/0885-3924(91)90030-8. [DOI] [PubMed] [Google Scholar]
- 11.Cavaliere R, Schiff D. Epidural spinal cord compression. Curr Treat Options Neurol. 2004;6(4):285–295. doi: 10.1007/s11940-004-0028-1. [DOI] [PubMed] [Google Scholar]
- 12.Egelmeers A, Goor C, van Meerbeeck J, van den Weyngaert D, Scalliet P. Palliative effectiveness of radiation therapy in the treatment of superior vena cava syndrome. Bull Cancer Radiother. 1996;83(3):153–157. doi: 10.1016/0924-4212(96)81747-6. [DOI] [PubMed] [Google Scholar]
- 13.Falkmer U, Jarhult J, Wersall P, Cavallin-Stahl E. A systematic overview of radiation therapy effects in skeletal metastases. Acta Oncol. 2003;42(5-6):620–633. doi: 10.1080/02841860310014895. [DOI] [PubMed] [Google Scholar]
- 14.Gaze MN, Kelly CG, Kerr GR, Cull A, Cowie VJ, Gregor A, et al. Pain relief and quality of life following radiotherapy for bone metastases: a randomized trial of two fractionation schedules. Radiother Oncol. 1997;45(2):109–116. doi: 10.1016/s0167-8140(97)00101-1. [DOI] [PubMed] [Google Scholar]
- 15.Cross CK, Berman S, Buswell L, Johnson B, Baldini EH. Prospective study of palliative hypofractionated radiotherapy (8. 5 Gy x2) for patients with symptomatic non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2004;58(4):1098–1105. doi: 10.1016/j.ijrobp.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Langendijk JA, ten Velde GP, Aaronson NK, de Jong JM, Muller MJ, Wouters EF. Quality of life after palliative radiotherapy in non-small cell lung cancer: a prospective study. Int J Radiat Oncol Biol Phys. pp. 149–155. [DOI] [PubMed]
- 17.Kranzbuhler H. Radiotherapy for tumour pain. Ther Umsch. 1998;55(7):423–425. [PubMed] [Google Scholar]
- 18.Awan AM, Weichselbaum RR. Palliative radiotherapy. Hematol Oncol Clin North Am. 1990;4(6):1169–1181. [PubMed] [Google Scholar]
- 19.Coia LR, Hanks GE, Martz K, Steinfeld A, Diamond JJ, Kramer S. Practice patterns of palliative care for the United States 1984-1985. Int J Radiat Oncol Biol Phys. pp. 1261–1269. [DOI] [PubMed]
- 20.Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322(8):494–500. doi: 10.1056/NEJM199002223220802. [DOI] [PubMed] [Google Scholar]