Abstract
OBJECTIVE
To examine whether Palm Prevention, a free software tool for Palm OS personal digital assistants (PDAs) that provides quick access to preventive guidelines in a patient-specific manner at the point of care, improved adherence to five preventive measures in primary care.
DESIGN
Prospective intervention pilot study.
SETTING
Vancouver, BC, and surrounding area.
PARTICIPANTS
Eight general practitioners.
INTERVENTIONS
Each physician used Palm Prevention for five preventive measures during routine preventive health visits with 10 patients (n = 80). Charts of consenting patients were reviewed for documentation of recommended maneuvers.
MAIN OUTCOME MEASURES
Rates of adherence to five evidence-based guidelines selected from the Canadian and American task forces on preventive care and incorporated into Palm Prevention.
RESULTS
Intervention and control physicians were similar in their familiarity with and use of PDAs, and they recruited similar patients for the study. Intervention and control groups had similar rates of screening for hypertension. Intervention improved adherence to the remaining four guidelines: cervical cancer screening increased 22% (only absolute increases are reported); hyperlipidemia screening increased 30%; colorectal cancer screening increased 27%; and prophylaxis with acetylsalicylic acid in high-risk patients increased 38%. Participants were surveyed after the study; all reported that they found the software helpful and would continue using Palm Prevention. Usage statistics showed that study participants used the tool outside the trial: users entered between 28 and 68 unique patients into the program during the 2-month intervention.
CONCLUSION
This pilot study suggests PDAs are useful in improving preventive care and facilitating translation of knowledge into practice. This was particularly apparent with newer guidelines.
Abstract
OBJECTIF
Déterminer si, dans un contexte de soins primaires, l’adhésion à cinq mesures préventives peut être améliorée par l’utilisation de Palm Prevention, un logiciel gratuit conçu pour les assistants numériques personnels (ANP) de poche qui procure un accès rapide à des directives de nature préventive adaptées aux besoins spécifiques des patients.
TYPE D’ÉTUDE
Étude d’intervention pilote prospective.
CONTEXTE
Vancouver (C.-B.) et ses environs.
PARTICIPANTS
Huit omnipraticiens.
INTERVENTIONS
Chaque médecin a utilisé le logiciel Palm Prevention pour cinq mesures préventives lors des visites périodiques de 10 patients (n = 80) pour des soins de santé préventifs. Les dossiers des patients consentants ont été consultés pour documenter les mesures recommandées.
PRINCIPAUX PARAMÈTRES MESURÉS
Taux d’adhésion à cinq directives reposant sur des données probantes provenant des groupes d’étude canadien et américain sur les soins de santé préventifs et incorporées au logiciel Palm Prevention.
RÉSULTATS
Les médecins des groupes expérimental et témoin avaient une connaissance et une utilisation des ANP similaires et ont recruté des patients semblables. Les deux groupes avaient le même taux de dépistage de l’hypertension. L’intervention a amélioré l’adhésion aux quatre autres directives: augmentation de 22% du dépistage du cancer du col (seules les augmentations absolues sont indiquées); de 30% du dépistage de l’hyperlipidémie; de 27% du dépistage du cancer colorectal; et de 38% de l’utilisation d’acide acétylsalicylique prophylactique chez les patients à risque élevé. Lors d’une enquête post-étude, les participants ont tous déclaré qu’ils avaient trouvé le logiciel utile et qu’ils continueraient de l’utiliser. Les statistiques sur l’utilisation ont montré que les participants ont employé Palm Prevention en-dehors de l’étude: ils ont entré entre 28 et 68 patients différents dans le programme pendant les deux mois de l’étude.
CONCLUSION
Cette étude pilote suggère que les ANP sont utiles pour améliorer les soins de santé préventifs et faciliter la mise en pratique des connaissances. Cela est particulièrement évident pour les nouvelles directives.
EDITOR’S KEY POINTS.
Family doctors are inundated with guidelines, especially in preventive care, and they struggle to keep abreast of them and to incorporate the latest evidence-based recommendations into practice.
This pilot study showed how a Palm-based preventive program, tailored to individual patient characteristics, could increase uptake of five specific guidelines.
Although similar guidelines can be incorporated into electronic medical records, physicians have been slow to adopt them. Palm-type technology is more accessible and could offer an efficient way to encourage use of guidelines.
POINTS DE REPÈRE DU RÉDACTEUR.
Les médecins de famille sont inondés de directives, notamment sur les soins de santé préventifs, et ils s’efforcent de rester à jour et d’incorporer à leur pratique les plus récentes recommandations fondées sur des données probantes.
Cette étude pilote a montré comment un programme préventif utilisant un ordinateur de poche et adapté aux caractéristiques individuelles des patients pouvait accroître la compréhension de cinq directives spécifiques.
Même si de telles directives peuvent être incorporées aux dossiers médicaux électroniques, les médecins ont été lents à les adopter. La technologie du type ordinateur de poche est plus accessible et devrait représenter une façon efficace de promouvoir l’utilisation des directives.
Considerable time and money have been used to develop and distribute clinical practice guidelines (CPGs). Many expert groups have been established to synthesize research to produce these guidelines.
While CPGs were often drawn from expert opinion in the past, today more guidelines are based on a rigorous examination of published evidence. The United States National Guideline Clearinghouse had more than 950 evidence-based guidelines in its collection as of May 2002.1 In North America, two key organizations have to date developed evidence-based preventive guidelines: the Canadian Task Force on Preventive Health Care (CTFPC) and the United States Preventive Services Task Force (USPSTF). These organizations have been developing, publishing, and updating guidelines for many years.2,3 They used rigorous and transparent approaches to guideline development.
When evaluating the effect of CPGs, one thing has become apparent: development and distribution of guidelines does not always produce changes in practice.4,5 A recent American study suggests that less than 55% of appropriate screening maneuvers are performed.6 When surveyed, physicians have described a variety of barriers to implementing guidelines in their practices, including awareness, familiarity, disagreement, self-efficacy, outcome expectancy, inertia of previous practice, doctor-patient relationships, and logistical problems.7,8
One method to improve CPG implementation is to provide patient-specific reminders at point of care.9 Tailoring guidelines—showing only recommendations appropriate for the patient being treated—reduces the amount of evidence presented and reduces information overload. This can be automated—an electronic medical record with an active clinical decision support system can present guidelines—or manual—a nurse can review charts and produce paper reminders before a physician sees each patient.10 While effective, these examples are often too costly or labour intensive to be implemented by family doctors in their offices. Personal digital assistants (PDAs) can be inexpensive tools for providing patient-specific reminders at point of care.
Increasingly, PDAs are finding their way into doctors’ hands.11 They are being used for clinical reference. A recent survey in the United States suggests that the number of doctors using PDAs as medical resources nearly doubled from 1999 to 2001 (from 10% to 18%).12 Most commonly, physicians use PDAs as a drug reference11 and report an improvement in care when they use PDAs.13 Personal digital assistants have several advantages over desktop computers: they are simpler, cheaper, and “pocketable,” so they are available wherever physicians practise; they fit more easily into the flow of a physician’s work.
Before this study, no implementation of preventive guidelines on a PDA provided the guidelines in a patient-specific manner. Palm Prevention uses patient characteristics to filter a collection of preventive guidelines and to show only the guidelines that are relevant to that patient. This pilot study was designed to examine whether using Palm Prevention improved adherence to five preventive measures in primary care.
METHODS
Software development and design
Palm Prevention was developed for this trial. It was written by the author for Palm OS PDAs using Satellite Forms 4.1 from PumaTech Inc.
Guideline content was used, with permission, from both the CTFPC and the USPSTF. Evidence levels were based on the CTFPC’s standard A through E rating system.2 The USPSTF uses a similar five-point scale. Guidelines were selected that were applicable to point-of-care management of adult patients. By default, Canadian guidelines were used. American guidelines were selected if they were more recently updated.
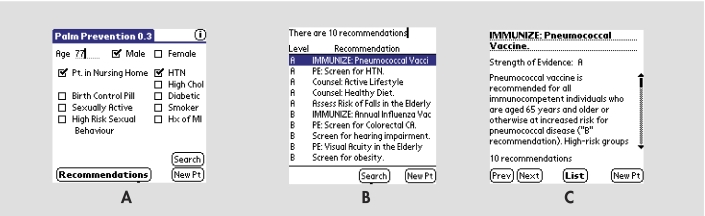
Figure 1 shows the Palm Prevention interface. A physician selects a patient’s age, sex, and appropriate risk factors. Tapping recommendations shows a list of applicable reminders from the software’s database. A research version of Palm Prevention automated data collection for this study.
Figure 1. Palm Prevention interface.
A) Main input screen for Palm Prevention where users enter the patient’s age and tap on various demographic options. Pressing “Recommendations” jumps users to a list of guidelines specific to patient data entered, ranked by level of evidence. B) Within each level, guidelines are clustered according to intervention type (counseling, physical examination, laboratory tests, and treatment). Tapping on any guideline title shows a detailed summary from the original guideline source. C) List and text can be scrolled through using scroll arrows or hardware buttons.
Study design
General practitioners were recruited from the Vancouver, BC, area through two educational presentations in 2001 focusing on PDA use in family medicine. Of the volunteers, eight GPs who owned Palm OS–based PDAs and who had integrated some level of preventive health care into their routine practice were selected. Physicians were randomized into two groups using a random number generator.
All physicians received the same information and survey at the start of the trial. They were asked to enrol 10 patients requesting routine preventive health visits. Patients enrolled were not pregnant, were 18 or older, and were able to provide informed consent. The intervention period was February 2002 to April 2002. Physicians were asked to obtain patient consent and document all preventive measures performed or discussed during the visit. The intervention group received Palm Prevention. The control group did not receive the software until after the study. The intervention group was surveyed after using Palm Prevention. For this pilot study and resident research project, eight physicians and 80 patients were recruited. This study was approved by the University of British Columbia’s Clinical Research Ethics Board.
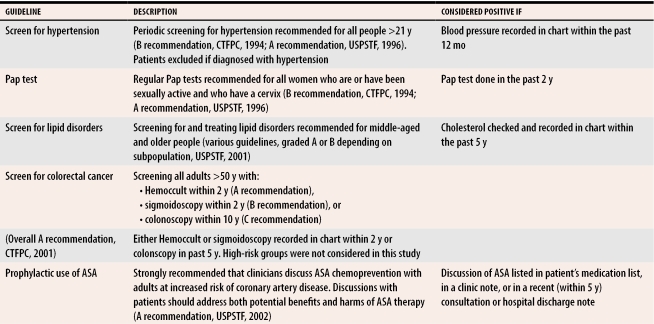
Chart reviews
All charts were reviewed by the author (not blinded). Five maneuvers (Table 1) were chosen for this study because they are clearly defined with explicit timing (eg, Pap smear every 2 years) and because the guidelines ranged from old to new. If a maneuver was not performed, patients’ charts were searched for contraindications. If a contraindication existed, that recommendation was withdrawn for that patient. The last 5 years of charts were reviewed for this study.
Table 1.
Guidelines studied in Palm Prevention
CTFPC—Canadian Task Force on Preventive Health Care; USPSTF—United States Preventive Services Task Force.
RESULTS
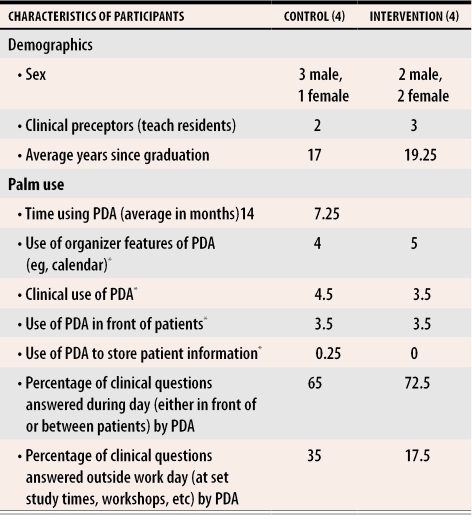
Physician participants
Table 2 compares characteristics of participants. Most physicians were fee-for-service physicians involved in teaching (evenly split between the two groups). All physicians graduated from Canadian medical schools, most from the University of British Columbia. All but one physician (in the intervention group) used the PDA daily to answer clinical questions.
Table 2. Participants’ demographic characteristics, familiarity with PDAs, and general usage patterns of PDAs.
All numbers are shown as averages of participants’ responses.
PDA—personal digital assistant.
*A 5-point scale was used to assess frequency (0–never; 1–less than once a month; 2–one to three times per month; 3–one to seven times a week; 4–once a day; 5–two or more times a day).
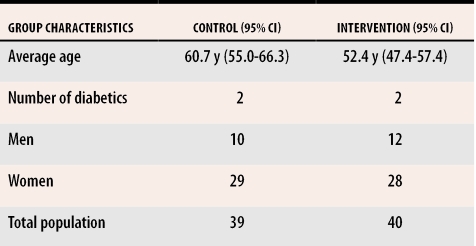
Patient enrolment
All GPs collected the required number of patients during the 2 months. One patient who did not fit the age requirements of the study was excluded in the control group. Patient groups were similar (Table 3).
Table 3.
Demographics of study and control groups
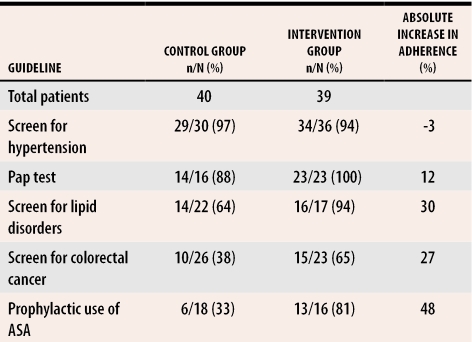
Adherence to guidelines
Table 4 compares how the two groups adhered to the five guidelines selected for the study. Not all patients qualified for all guidelines; thus, the total number of patients varies for each guideline. Adherence rates increased more for newer guidelines than older ones (hypertension screening and cervical cancer screening).
Table 4. Adherence to the five studied guidelines.
Denominator indicates number of patients eligible for a specific intervention (as determined by guideline criteria); numerator indicates number of patients who received the intervention.
Using Palm Prevention
After using Palm Prevention, all users stated that they would continue to use the software. Reasons for continuing included “quick, evidence-based [and] easy to use at the point of care” and “level of evidence helped with deciding how much time to devote to each topic.” One user commented that Palm Prevention “makes me more thorough, and patients appreciate the completeness.” All physicians used Palm Prevention more than requested; they entered between 18 and 58 extra patients into Palm Prevention during the study.
DISCUSSION
This very small study does not warrant statistical analysis. The results, although interesting, should be interpreted with caution. Use of a reminder system at point of care improves adherence to guidelines. Palm Prevention is such a reminder system for preventive care. This pilot study suggests that reminding physicians of guidelines in this manner improves the quality of care delivered, particularly with newer guidelines.
Guideline adherence
Blood pressure measurements have been taken by physicians for many years; patients almost seem to expect measurements as part of any checkup. The CTFPC has been recommending screening for more than 18 years.14 Unsurprisingly, this was the most-performed screening maneuver (more than 90% of eligible patients). There was no increase with the reminder, likely due to a ceiling effect.
Pap smears have long been described as an important screening activity.15 Next to hypertension screening, Pap smears were the most routinely performed in the population studied. Even with the provincial registry in British Columbia, however, compliance was still not 100% among patients who participated in the study. The intervention group showed a modest increase in screening for cervical cancer.
Evidence for screening cholesterol in patients who are at near-term risk of coronary artery disease is growing. Several groups have recommended screening these patients.16 There was a greater screening rate (30% greater) in the group using Palm Prevention.
Colorectal screening guidelines were published by the CTFPC in 2001.17 Despite a considerable increase in adherence (27%), this guideline had the lowest adherence rate (65%) in the intervention group. This could be due to available resources, or because screening for colorectal cancer is an embarrassing topic for patients and physicians. Either way, this study indicates that other interventions are needed to improve adherence to this guideline in British Columbia.
A new guideline on prophylaxis with ASA for patients at high risk of coronary artery disease was a based on a recent review of the evidence, and was published by the USPSTF just before the start of this study.18 As the newest guideline, and perhaps one that physicians would be the least familiar with, it had the largest increase in adherence of the five guidelines in this study.
Physicians in this study incorporated Palm Prevention into their practice, using it more than requested. Perhaps this is because a PDA is simple to use, is inexpensive, and can be integrated into GPs’ practice styles.19 These features could be why PDAs have been so quickly adopted, despite the lack of large studies supporting their usefulness.20
Limitations
Although participants were randomly assigned to groups, there were only eight of them. Differences in practice style could account for some of the differences seen between the two groups.
The physicians recruited for this study are “early adopters.” While clinical PDA use is increasing, and some expect that accessing useful clinical resources at point of care will be the next “major advance for physicians,”21 PDAs are not as common as stethoscopes. This project might have appealed to participants because they are already champions of, and are comfortable with, technology. These findings might not generalize to other physicians. It is important to know whether similar tools would appeal to other physicians.
This study looked only at initial use of the software. Further study is needed to see if tools like Palm Prevention can change physicians’ behaviour over a longer period.
The Hawthorne effect, often cited, likely affects these study results. Being involved in a study likely stimulated both groups to be more comprehensive in their preventive health care and documentation than usual. This could be more apparent in the control group. A longer-term study might reduce this effect.
This study looks only at preventive care for patients who go to physicians. Patients who do not go to physicians could not be enrolled in the study, and, therefore, there could be considerable bias in the reported adherence rates.
Conclusion
This pilot study, despite small numbers, showed improvements in the quality of preventive care delivered by physicians using Palm Prevention, particularly with newer recommendations that had not already become part of routine practice. The results of this pilot study suggest a need for larger studies on the effect of PDAs on health care delivery. Simple, PDA-based tools, such as Palm Prevention, could aid physicians in using clinical decision–support tools and aid in the delivery of evidence-based care.
Acknowledgments
I thank Drs Colleen Kirkham, Jonathan Berkowitz and Francis Lau for supporting the project and reviewing the manuscript. I also thank the St Paul’s Hospital Department of Family Practice and the St Paul’s Family Practice residency program, the British Columbia Medical Association, and the Canadian and American task forces on preventive health care for their support and interest in the research.
Biography
Dr Price is a Clinical Assistant Professor in the Department of Family Practice at the University of British Columbia in Vancouver.
Footnotes
Competing interests: The author has been involved in development of several PDA-based medical tools for education, practice, and research. Palm Prevention was developed for this study as part of his resident research project at the University of British Columbia. He has no financial interest in the sale of Palm Prevention. It is available free of charge from http://www.pdaguidelines.com.
References
- 1.National Guideline Clearinghouse. Guideline index. Rockville, Md: Agency for Healthcare Research and Quality; 2002. [cited 2002 May 14]. Available from: http://www.guideline.gov/browse/guideline_index.aspx. [Google Scholar]
- 2.Canadian Task Force on the Periodic Health Examination. The Canadian guide to clinical preventive health care. 2nd ed. Ottawa, Ont: Health Canada; 1994. [Google Scholar]
- 3.US Preventive Services Task Force. Guide to Clinical Preventive Services. 2nd ed. Washington, DC: US Department of Health and Human Services; 1996. [cited 2005 Aug 25]. Available at: http://www.ahrq.gov/clinic/cpsix.htm. [Google Scholar]
- 4.Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ. Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med. pp. 1306–1311. [DOI] [PubMed]
- 5.Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342(8883):1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- 6.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 7.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. pp. 1458–1465. [DOI] [PubMed]
- 8.Freeman AC, Sweeney K. Why general practitioners do not implement evidence: qualitative study. BMJ. 2001;323(7321):1100–1102. doi: 10.1136/bmj.323.7321.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weingarten S. Translating practice guidelines into patient care: guidelines at the bedside. Chest. 2000;118(2 Suppl):4–7. doi: 10.1378/chest.118.2_suppl.4s. [DOI] [PubMed] [Google Scholar]
- 10.Johnston ME, Langton KB, Haynes RB, Mathieu A. Effects of computer-based clinical decision support systems on clinician performance and patient outcome. A critical appraisal of research. Ann Intern Med. 1994;120(2):135–142. doi: 10.7326/0003-4819-120-2-199401150-00007. [DOI] [PubMed] [Google Scholar]
- 11.McLeod TG, Ebbert JO, Lymp JF. Survey assessment of personal digital assistant use among trainees and attending physicians. J Am Med Inform Assoc. 2003;10(6):605–607. doi: 10.1197/jamia.M1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor H, Leitman R. Physicians’ use of handheld personal computing devices increases from 15% in 1999 to 26% in 2001. Health Care News. 2001;1(25):1–4. [Google Scholar]
- 13.Rothschild JM, Lee TH, Bae T, Bates DW. Clinican use of palmtop drug reference guide. J Am Med Inform Assoc. 2002;9(3):223–229. doi: 10.1197/jamia.M1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canadian Task Force on the Periodic Health Examination. The periodic health examination: 2. 1984 update. CMAJ. 1984;130(10):1278–1285. [PMC free article] [PubMed] [Google Scholar]
- 15.Morrison BJ. Screening for cervical cancer. In: Canadian Task Force on the Periodic Health Examination. The Canadian guide to clinical preventive health care. 2nd ed. Ottawa, Ont: Health Canada; 1994. pp. 870–881. [Google Scholar]
- 16.US Preventive Services Task Force. Screening adults for lipid disorders: recommendations and rationale. Am J Prev Med. 2001;20(3 Suppl):73–76. [PubMed] [Google Scholar]
- 17.Canadian Task Force on Preventive Health Care. Colorectal cancer screening. Recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2001;165(2):206–208. [PMC free article] [PubMed] [Google Scholar]
- 18.Hayden M, Pignone M, Phillips C, Mulrow C. Aspirin for the primary prevention of cardiovascular events: a summary of the evidence for the US Preventive Services Task Force. Ann Int Med. 2002;136(2):161–172. doi: 10.7326/0003-4819-136-2-200201150-00016. [DOI] [PubMed] [Google Scholar]
- 19.Criswell DF, Parchman ML. Handheld computer use in US family practice residency programs. J Am Med Inform Assoc. 2002;9(2):80–86. doi: 10.1136/jamia.2002.0090080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fischer S, Stewart TE, Mehta S, Wax R, Lapinsky SE. Handheld computing in medicine. J Am Med Inform Assoc. 2003;10(2):139–149. doi: 10.1197/jamia.M1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilcox RA, Whitham EM. Reduction of medical error at the point-of-care using electronic clinical information delivery. Intern Med J. 2003;33(11):537–540. doi: 10.1046/j.1445-5994.2003.00465.x. [DOI] [PubMed] [Google Scholar]