EDITOR’S KEY POINTS.
This case report describes an immigrant woman who presented for a general checkup with only mild symptoms of fatigue and was found to have a profound iron deficiency anemia of 45 g/L.
The standard immigration screening for admission to Canada is oriented to detect conditions of public health risk and is not a general assessment.
This case illustrates the wisdom of comprehensive medical screening for immigrant patients who might not volunteer symptoms and who might have adapted to chronic conditions.
POINTS DE REPÈRE DU RÉDACTEUR.
Cet article décrit le cas d’une immigrante qui se plaignait seulement d’une fatigue légère mais chez qui l’examen médical complet a révélé une profonde anémie ferriprive de 45 g/L.
Le dépistage standard exigé par l’Immigration pour l’admission au Canada vise surtout a détecter des conditions présentant un risque de santé publique; ce n’est pas un examen de santé général.
Ce cas illustre la pertinence d’un dépistage médical complet pour les immigrants qui pourraient être tentés de taire certains symptômes et qui pourraient s’être adaptés à des états chroniques.
Anemia, a reduction below normal in concentration of blood hemoglobin or total red blood cell volume,1 is often seen by family physicians and has a variety of underlying causes. Common causes among immigrant and refugee populations include micronutrient deficiency, hemoglobinopathy, alpha and beta thalassemia, and glucose-6-phosphate dehydrogenase deficiency.2
Anemia is particularly prevalent among refugee women. The diagnosis, however, is easily overlooked, as these women are often asymptomatic. This case report demonstrates the importance of comprehensive health screening for postimmigration refugees to detect chronic illnesses, such as anemia, and highlights disparities in access to health services that persist worldwide.
Case description
Mrs A., a 44-year-old Syrian refugee who had recently arrived in Canada, came to the clinic for immunizations for her children. Once her children were looked after, she consented to a general checkup for herself. She identified no major health concerns but did note some fatigue before menstruation.
Mrs A.’s medical history was generally unremarkable. She had 3 healthy pregnancies with uncomplicated term deliveries, and an intrauterine device had been inserted 2 years ago for contraception. She had no history of chest pain or claudication. Menses were regular with no reported history of abnormal bleeding or menorrhagia caused by the intrauterine device. There was no recent weight loss, chills, epistaxis, or bleeding gums, and she denied bruising easily. In addition, she had no history of hematochezia, melena, hematuria, liver failure, jaundice, pale stools, dark urine, or itchiness. She had no drug allergies, and did not smoke or drink alcohol. She had not taken any medications recently.
Mrs A. appeared well nourished but pale. She was afebrile, her blood pressure was 157/87 mm Hg, her resting heart rate was 105 beats a minute, her respiratory rate was 12 breaths a minute, and she had capillary oxygen saturation of 100% on room air. There were no orthostatic changes in her vital signs. Her chest was clear and her heart sounds were normal.
Mrs A.’s initial screening tests showed grossly abnormal hemoglobin (45 g/L), with microcytic red cells (54.9 fL) and an increased red cell distribution width (27.3%). Her ferritin was also low (2 mcg/L). She had a normal thyroid-stimulating hormone level and a normal white blood cell count.
Follow-up testing revealed an abnormal reticulocyte count (105.6 x 109/L), iron saturation of 3%, and total iron-binding capacity of 77%. She also had slightly abnormal serum B12 levels (116 pmol/L). Her hemoglobin electrophoresis ruled out thalassemia major, and the results of her glucose-6-phosphate dehydrogenase test were negative. Serum folate, transferrin, haptoglobin, and bilirubin levels were all normal. She had group A positive blood with no antibodies present. Pelvic ultrasound showed a normally placed intrauterine device.
Mrs A. was referred to hospital where she received a transfusion of 3 units of whole blood. Due to the severity of the anemia, a gastroenterology consultation, including endoscopy and colonoscopy, was conducted to rule out any gastrointestinal bleeding or problems with malabsorption; the results were all normal. On discharge from hospital her hemoglobin had increased to 75 g/L. Her discharge medications were 300 mg of ferrous gluconate, 3 times daily; folic acid, 5 mg daily; and vitamin B12, 1000 mcg daily, all taken orally.
Mrs A. reported to the clinic 1 week later feeling much better. Over the following months her hemoglobin returned to normal (125 g/L) on iron therapy, as did her pulse rate and blood pressure.
Discussion
This case of iron deficiency anemia serves as a reminder of the high prevalence of undiagnosed micronutrient deficiencies in the developing world and thus the importance of comprehensive screening in postimmigration refugee care. Health inequities persist, and the gap is widening between the world’s poorest people and those better placed to benefit from economic development and public health strategies.3
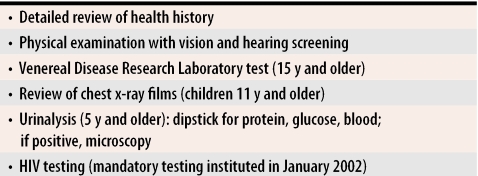
Many physicians and patients mistakenly assume that the Canadian preimmigration medical examination provides comprehensive preventive health screening for immigrants. This medical examination (Table 1) is designed to screen for patients who might pose a public health risk or place undue burden on the Canadian health care system.4 This examination is not designed as a preventive health screening tool to meet the ongoing health needs of immigrants. Indeed, comprehensive health screening after an immigrant arrives should be delivered with a focus on individual health needs,5 within a confidential professional relationship, and with adherence to public health recommendations.
Table 1.
Citizenship and Immigration Canada medical examination
Anemia in immigrants and refugees is frequently multifactorial. While iron deficiency is the most common cause of anemia worldwide, genetic traits, such as thalassemia and hemoglobinopathy (eg, sickle cell disease, glucose-6-phosphate dehydrogenase deficiency, hemoglobin E disorder) should be considered in immigrants of Southeast Asian, African, and Mediterranean descent.5 Hemoglobin electrophoresis should be performed, ideally once iron stores have been replenished, in cases of microcytic anemia among immigrants.
Mrs A. presented to the clinic with low expectations for health care. She was surprised when advised of the screening tests and immunizations available to her and might have assumed, like many adult refugees, that vaccines and general checkups were only for children. Many refugees fail to obtain preventive procedures because they are unfamiliar with health services, because of language and cultural barriers, and because they have limited appreciation for the value of preventive health care.6
Many illnesses among refugees from low-income countries, are undiagnosed as a result of health care inequities.7 Physicians should be aware of substantial inequities in health care services. Shortages of qualified staff, medications, technology, and equipment8 are everyday realities. These shortages can lead to underdetection of chronic disease, resulting in poorer health outcomes.
This case of chronic anemia exemplifies how the body adapts to low iron levels, resulting in few signs of disease. Given that Mrs A. did not report feeling ill at the initial visit, her improved sense of well-being after receiving treatment is interesting. Mrs A.’s anemia might have remained undetected or become life threatening had health screening not been suggested.
Conclusion
Providing comprehensive and culturally appropriate health care to refugee populations can be as rewarding as it is challenging; it often has a great effect on the life of a new immigrant.2 The case of Mrs A. exemplifies the need for a comprehensive screening program for all refugees and newcomers to Canada. Once illnesses such as anemia are identified, therapy can be provided, in conjunction with health promotion, to improve patient health outcomes.
Biographies
Dr Pottie is a Principal Scientist at the Institute of Population Health and is an Assistant Professor in the Department of Family Medicine and co-Director of the Immigrant Health and Visiting Friends and Relatives Program at the University of Ottawa in Ontario.
Ms Topp is a nurse practitioner in the Immigrant Health and Visiting Friends and Relatives Program.
Dr Kilbertus is an Assistant Professor in the Department of Family Medicine and co-Director for the Immigrant Health and Visiting Friends and Relatives Program.
Footnotes
Competing interests: None declared
References
- 1.Little DR. Ambulatory management of common forms of anemia. Am Fam Physician. 1999;59:1598–1604. [PubMed] [Google Scholar]
- 2.Adams KM, Gardiner LD, Assefi N. Healthcare challenges from the developing world: post-immigration refugee medicine. BMJ. 2004;328:1548–1552. doi: 10.1136/bmj.328.7455.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palinkas L, Pickwell SM, Brandstein K, Clark TJ, Hill LL, Moser RJ, et al. The journey to wellness: stages of refugee health promotion and disease prevention. J Immigr Health. 2003;5(1):19–28. doi: 10.1023/a:1021048112073. [DOI] [PubMed] [Google Scholar]
- 4.Gushulak BD, Williams LS. National immigration health policy: existing policy, changing needs, and future directions. Can J Public Health. 2004;95(3):27–29. doi: 10.1007/BF03403662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stauffer WM, Kamat D, Walker PF. Screening of international immigrants, refugees, and adoptees. Prim Care. 2002;29(4):879–905. doi: 10.1016/s0095-4543(02)00035-0. [DOI] [PubMed] [Google Scholar]
- 6.Bacaner N, Stauffer B, Boulware DR, Walker PF, Keystone JS. Travel medicine considerations for North American immigrants visiting friends and relatives. JAMA. pp. 2856–2864. [DOI] [PubMed]
- 7.Gavagan T, Brodyaga L. Medical care for immigrants and refugees. Am Fam Physician. 1998;57:1061–1068. [PubMed] [Google Scholar]
- 8.Jong-wook L. Global health improvement and WHO: shaping the future. Lancet. 2003;362:2083–2088. doi: 10.1016/S0140-6736(03)15107-0. [DOI] [PMC free article] [PubMed] [Google Scholar]