Excision of sebaceous (epidermoid) cysts is a common surgical procedure performed by family physicians. In 2003, I started a referral clinic in Kingston, Ont, called the Minor Office Procedures Clinic. My objectives were to provide a clinic for referrals from family doctors who did not do minor surgery and to use this as an opportunity to teach first-year family medicine residents. Many family doctors in our area have stopped doing surgery in their offices, perhaps because of overloaded practices, compensation issues, or concerns about equipment.
MEDLINE was searched using the key word sebaceous cyst OR the MeSH heading epidermoid cyst. There is debate regarding the proper histologic classification of these cysts.1 The tips below are formulated primarily from attempts to describe my methods to first-year residents.
Common indications for sebaceous cyst excision include recurrent inflammation, annoyance, and cosmetic concerns. Provincial fee schedules and regulations determine which procedures are insured services. Relative contraindications include severe inflammation and recent incision and drainage.
Equipment required
You will need a sterile surgical tray, chlorhexidine, sterile drapes, local anesthesia (usually lidocaine 1% with epinephrine), suture material, sterile gloves, 4-cm by 4-cm gauze pads, and adequate lighting. Essential are a scalpel, two curved hemostats, a needle driver, scissors, toothed forceps, and suture material.
Method
The method includes sterile preparation, draping, local anesthesia, excision by a combination of sharp and blunt dissection, and closure of the wound. The key is to remove the cyst sac intact with minimal or no leakage of sebum. An alternate method involves a smaller incision into the sac, manual expression of the sebum, and removal of the empty sac using forceps and scissors.2,3 Although the scar is smaller, the wound will have a higher rate of inflammation and drainage. Some physicians using the microincision technique have treated the empty sac with the chemical phenol.4
Tip 1.
Avoid excision when the cyst is inflamed. A minimum of 4 weeks should be allowed after a drainage procedure. Most inflamed sebaceous cysts (inflamed due to sebum) are not infected and will settle spontaneously over 4 weeks. Antibiotics, such as cephalexin or cloxacillin, are commonly used but in fact probably provide little benefit.
Tip 2.
Try to avoid incision and drainage, as it will be inconvenient for the patient (eg, packing, home care) and will make the eventual excision more difficult. Incise and drain only if there is copious fluid build-up.
Tip 3.
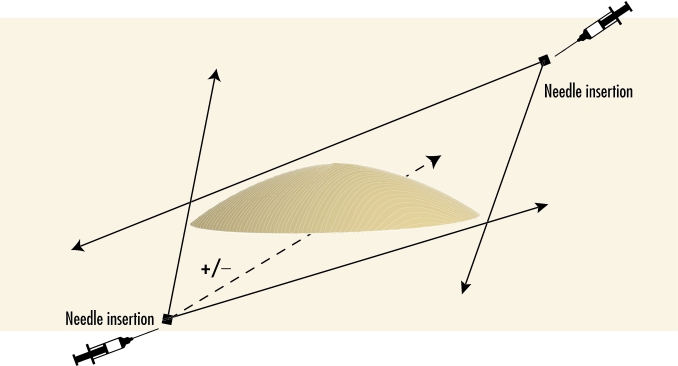
Use lidocaine with epinephrine unless contraindicated (eg, distal extremity) to lessen bleeding. Make a diamond-shaped field block, as illustrated in Figure 1. Additional anesthetic can be injected below large cysts. Avoid injection into the cyst itself, as this will increase the pressure inside and increase risk of rupture. You can monitor pressure by palpating the cyst while injecting the lidocaine. If lidocaine is inadvertently injected into the sac, consider trying to decompress by aspirating cyst material.
Figure 1. Infiltration of local anesthetic.
Additional anesthetic can be injected below large cysts.
Tip 4.
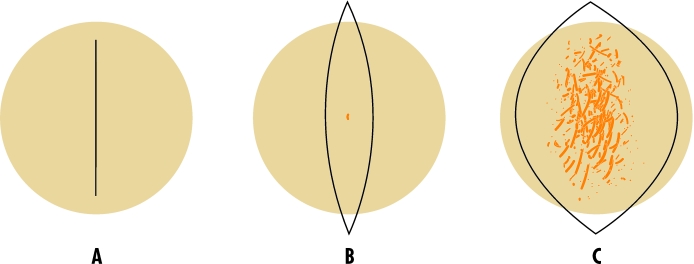
Choose the appropriate skin incision as outlined in Figure 2. If the cyst is not inflamed or scarred and does not have a residual punctum on the skin, do a linear incision over the middle. If a punctum or scar is present, a small elliptical incision is advisable. If the cyst has had recurrent inflammation or scar tissue formation, more radical excision is indicated.
Tip 5.
The initial incision with the scalpel should have a light touch so as not to go completely through the dermis and into the cyst. Maintain an even depth mid-dermis along the length. When in doubt, stay superficial and alternate between Tips 5 and 6 until you see the cyst.
Tip 6.
Use the curved hemostat to “test” the depth of the incision by gently spreading perpendicular to the incision. When the incision is deep enough, the tissues will spread, and the cyst will be evident. If the incision is not deep enough, repeat Tip 5.
Tip 7.
Whenever possible, use blunt dissection rather than a scalpel to dissect around the cyst. Place the closed curved hemostat around the cyst and spread. Initially point the tip away from the centre to avoid inadvertent injury to the cyst wall. Firm areas of connective tissue can be divided with a scalpel. As experience increases, more sharp and less blunt dissection can be employed.
Tip 8.
If the cyst ruptures, try to clamp the hole with hemostats. Try to avoid sebum contact with the wound, as it is intrinsically inflammatory. In many cases, it will be necessary to abandon blunt dissection, lift the cyst with a hemostat, and use the scalpel to expedite removal. Aim to have to do this less than 20% of the time.
Tip 9.
Avoid two-layer closure for small and moderate-sized cysts (up to 2-cm diameter). The small space can usually be closed quite well with a vertical mattress technique. For small excisions, simple interrupted closure can be done. Using a deep layer of absorbable suture material considerably increases the duration and complexity of the procedure and could lead to more inflammation and potential for a stitch abscess. In cases where there is a larger cavity, a few deep absorbable (Vicryl or Monocryl) stitches can be placed with the knot along the deep side of the stitch and the ends cut short.
Tip 10.
Clean wounds thoroughly and send patients home with dressings that will not allow blood to leak through. Patients’ spouses or friends will judge your work by the external appearance when patients get home.
Conclusion
I have applied these practice tips in teaching sebaceous cyst excision to relatively inexperienced first-year family medicine residents. I have found that they have been able to become independent more quickly and rupture cysts less frequently. Family physicians can use these tips to increase their comfort with cyst excision and provide a beneficial treatment to their patients.
Figure 2. Three possible incision techniques.
A) No inflammation, B) Central puncta or inflammation, C) Extensive inflammation or scar tissue
Biography
Dr Sempowski is an Assistant Professor in the Department of Family Medicine at Queen’s University in Kingston, Ont.
References
- 1.Kwittken J. Sebaceous cyst: fact, not fiction. Int J Dermatol. 1994;33(3):218–219. doi: 10.1111/j.1365-4362.1994.tb04990.x. [DOI] [PubMed] [Google Scholar]
- 2.Nakamura M. Treating a sebaceous cyst: an incisional technique. Aesthet Plast Surg. 2001;25(1):52–56. doi: 10.1007/s002660010095. [DOI] [PubMed] [Google Scholar]
- 3.Klin B, Ashkenazi H. Sebaceous cyst excison with minimal surgery. Am Fam Physician. 1990;41(6):1746–1748. [PubMed] [Google Scholar]
- 4.Moore C, Greer DM. Sebaceous cyst extraction through mini-incisions. Br J Plast Surg. 1975;28(4):307–309. doi: 10.1016/0007-1226(75)90040-5. [DOI] [PubMed] [Google Scholar]