Abstract
OBJECTIVE
To review the evidence on prevention and management of childhood obesity and to offer suggestions for family physicians.
QUALITY OF EVIDENCE
Articles were obtained from a PubMed search. Most studies on pediatric obesity provide level II evidence. There are some level I studies on management.
MAIN MESSAGE
Pediatric obesity is underdiagnosed and undertreated. Prevention should be initiated as early as pregnancy. Prevention and treatment approaches should include patient and family interventions focusing on nutrition, physical activity, reduced television viewing, and behaviour modification. The effectiveness of such interventions by primary care physicians has not been totally demonstrated, but incorporating them into clinical practice routines is likely to be beneficial.
CONCLUSION
Family physicians have a role in promoting preventive measures and identifying and treating obesity-related comorbidity. Pediatric obesity is not an individual child’s problem, but a problem that involves the whole family and the community. Recommending a healthy diet and increased physical activity and counseling families on behaviour change is the best approach to preventing and managing childhood obesity.
Abstract
OBJECTIF
Faire une revue des données sur la prévention et le traitement de l’obésité infantile et faire certaines suggestions aux médecins de famille.
QUALITÉ DES PREUVES
Les articles retenus proviennent d’une consultation de PubMed. La plupart des études sur l’obésité infantile fournissent des preuves de niveau II. Quelques études sur le traitement sont de niveau I.
PRINCIPAL MESSAGE
L’obésité infantile est sous-diagnostiquée et sous-traitée. La prévention devrait débuter dès la grossesse. La prévention et le traitement devraient comporter des interventions auprès du patient et de sa famille, en insistant sur l’alimentation, l’exercice, la réduction des heures de télévision et des changements comportementaux. L’efficacité de ces interventions par le médecin de première ligne n’a pas été clairement démontrée, mais leur ajout à la pratique quotidienne devrait s’avérer avantageuse.
CONCLUSION
Le médecin de famille a un rôle à jouer dans la promotion des mesures préventives et dans l’identification et le traitement de la comorbidité associée à l’obésité. L’obésité infantile ne touche pas uniquement l’enfant; c’est un problème qui relève de toute la famille et de la communauté. La meilleure façon de prévenir et de traiter l’obésité infantile consiste à recommander plus d’exercice et une alimentation saine, et à inciter la famille à certains changements comportementaux.
EDITOR’S KEY POINTS.
Pediatric obesity is underdiagnosed and is increasing at such an alarming rate in Canada that there will be serious consequences for the health care system as these obese children mature. Childhood obesity is a strong predictor of adult obesity.
The most important causes appear to be a decline in physical activity (due to increased time watching television and playing video games) and an increase in caloric intake (mostly carbohydrates in soft drinks and juices).
Obese children should be assessed with a full history, physical examination, and laboratory workup as befits patients with a serious problem. Physicians should ensure that treatment plans, such as increased activity, decreased television watching, and changes in diet, are supported by patients’ families.
Family doctors can play an important role in identifying pediatric obesity early, assessing it carefully, and planning interventions that are effective but also take into account the psychosocial aspects of the problem within the family.
POINTS DE REPÈRE DU RÉDACTEUR.
L’obésité infantile est un problème sous-diagnostiqué et son taux d’augmentation est si alarmant qu’on prévoit des conséquences graves pour le système de santé avec le vieillissement des enfants obèses. L’obésité infantile est un puissant facteur de prédiction pour l’obésité adulte.
Les causes majeures semblent être le manque d’exercice (par augmentation du temps passé à la télévision et aux jeux vidéo) et une prise calorique excessive (glucides surtout, sous forme de boissons gazeuses et de jus).
L’évaluation de l’enfant obèse devrait inclure l’histoire médicale complète, l’examen physique et certains examens de laboratoire, à l’instar des patients qui ont un problème sérieux. Le médecin devrait s’assurer que les éléments du traitement recommandé, tels que l’augmentation de l’exercice, la diminution des heures d’écoute de la télévision et les changements alimentaires, ont l’appui des parents.
Le médecin de famille peut jouer un rôle important pour identifier précocement l’obésité infantile, en faire une évaluation attentive et planifier des interventions efficaces, tout en tenant compte des aspects psychologiques du problème au sein de la famille.
Obesity is now well known as a medical problem among children. Outcomes associated with obesity in adults are now affecting children.1-3 The prevalence of overweight status has tripled worldwide in the last 2 to 3 decades, including in developing countries and regions that are increasingly urbanized.1 Among children aged 5 to 17 years, about 155 million are estimated to be overweight; 30 to 45 million of them are classified as obese.1
In Canada, recent data indicate that the prevalence of overweight status has more than doubled among school-aged children (7 to 13 years old) from 15% in 1981 to 33% and 26% in 1996 among boys and girls, respectively.4 In 1996, the prevalence of obesity was 10% for boys and 9% for girls.4 Provincial variation was observed with a trend toward increasing risk of being overweight from west to east. Socioeconomic status was inversely related to the prevalence of overweight status, regardless of geographic region.4
In the United States, the prevalence of obesity and overweight status varies greatly among ethnic groups. Overweight status is highest among Mexican people, intermediate among non-Hispanic black people, and lowest among non-Hispanic white people.1 Canada currently has no nationally representative obesity prevalence data for ethnic subgroups.
Pediatric obesity is not limited to industrialized countries; developing countries report an increasing prevalence also. In 38 countries where data were available, 16 showed a rising trend toward obesity, 14 were static, and only eight showed a falling rate.5 Psychosocial and economic problems are also associated with pediatric obesity. Obesity impairs physical function and quality of life, causes at least 300 000 premature deaths yearly, and costs $100 billion in health care services annually in the United States.1
Physicians sometimes fail to diagnose obesity in children.6 Providers identified obesity as a problem for only 50% of the obese children examined for health supervision. Even for children identified as obese by their providers, evaluation and treatment were often not consistent with current recommendations.6
Considering the magnitude of the epidemic, increased awareness and identification of obesity in primary care are essential.7 Family physicians have an important role in timely identification of overweight and obese children during periodic health examinations. They also have a role in promoting preventive measures and encouraging positive changes in behaviour, as well as identifying and treating obesity-related comorbidity. Family physicians should have the skills to identify pediatric obesity and its risk factors, and knowledge of treatment options. The goal of this article is to provide the best information available to help family physicians prevent and manage pediatric obesity.
Quality of evidence
Articles were sought through a PubMed search using the key words pediatric obesity and the MeSH words diet, exertion, behavioural modification, prevention, and management. Most studies provided level II evidence; a few intervention studies provided level I evidence.
Etiology
Genetics or environment?
Body mass index (BMI) is the standard criterion for measuring obesity in children and adults, and when used for children, provides a uniform measure across age groups. Body mass index is defined as weight in kilograms divided by height in metres squared (kg/m2). Obesity is defined as a BMI score at or above the 95th percentile for age and sex, respectively, and overweight status as a BMI between the 85th and 95th percentile for age and sex, respectively.2,3 These percentiles correspond to adult BMIs of 25 and 30, respectively, the accepted definitions of adult overweight status and obesity.8
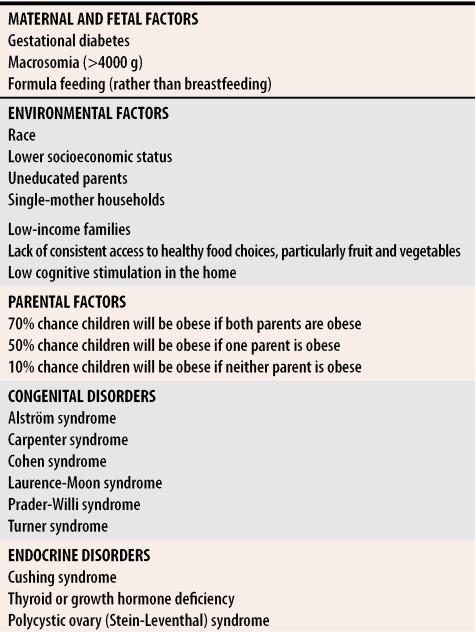
The epidemic of pediatric obesity cannot be explained by genetics alone or environment alone. Generally, obesity aggregates in families; high birth weight, maternal diabetes, and obesity in family members all are risk factors (Table 11-3,9,10). Obesity can be established through an interaction of more than 250 different genes, but the obese phenotype comes from gene-environment interactions.11,12 A longitudinal study (level II evidence) of 33 413 infants whose birth weight was >4000 g showed they were more than three times as likely to be obese at age 17 as infants with lower birth weights.13 This indicates a need for earlier surveillance, even as early as the prenatal period.
Table 1.
Risk factors associated with pediatric obesity
Genetic and endocrine causes.
Genetic and endocrine conditions known to be associated with a propensity for obesity (Table 11-3,9,10) are rare; diagnosing them requires collaboration with geneticists, endocrinologists, and other health specialists. They are generally associated with short stature, delayed growth and sexual maturation, or mental retardation and can be ruled out by history and physical examination. The task of primary care physicians is to diagnose these conditions early and to refer patients quickly to subspecialists. Discussion of these disorders is beyond the scope of this paper.
Lack of physical activity
The epidemic could be due to a decline in physical activity, a rise in fat intake, or a combination of both. Results of an epidemiologic study (level II evidence) of 7216 children aged 7 to 11 years support a link between physical inactivity and obesity in Canadian children.14 Television viewing plays a large part in this epidemic. A prospective study (level II evidence) of 700 children aged 10 to 15 years followed for 4 years showed that children watching television for more than 5 hours a day were five times as likely to be overweight as those watching less than 2 hours a day.15 Having a television in the bedroom is a strong predictor of being overweight (level II evidence), even among preschool-aged children.16 Results of a randomized controlled trial (level I evidence) showed that decreasing the amount of television school-aged children watched, even without specifically promoting more active behaviour, resulted in a significantly lower increase in their BMI score at 1-year follow up, compared with a control group.17
Changing diet
Some think that the increase in pediatric obesity is due to an increase in fat intake. The efficiency of nutrient use is higher for fat than for carbohydrates or protein, reflecting the small amount of energy required for synthesizing triglyceride. A 1-year longitudinal study (level II evidence) of more than 10 000 children aged 9 to 14 years, however, did not show any relationship between change in adiposity and fat intake.18 The main objection to dietary fat as being responsible for the current epidemic of obesity is that American children’s consumption of fat has decreased. In 1991, the National Cholesterol Education Program issued dietary guidelines for children 2 years and older that recommended reducing cholesterol intake to 300 mg/d, dietary fat to 30% of calories, and saturated fat to 10% of total energy intake.19 Fat, when eaten in excess, will eventually lead to obesity in predisposed patients. It seems unlikely, however, that increased fat consumption is responsible for the increase in pediatric obesity.
The amount of carbohydrate in children’s diets is a strong contender. Children began consuming more carbohydrates as a result of the recommendation to decrease dietary fat.18 Children increased their intake of simple sugars, mainly in the form of soft drinks, soda, and fruit drinks. Soft-drink consumption tripled between 1977-1978 and 1994 and now contributes to about 8% of adolescents’ total energy intake.20 In a prospective observational analysis (level II evidence), the authors demonstrated that increased consumption of simple sugars was associated with obesity in children.21 Also, increases in portion sizes of a variety of foods eaten at home and outside and eating fast food have been identified as risk factors for childhood obesity (level II evidence).22
Consequences of childhood obesity
Obesity is associated with health problems in children and is an important early risk factor for adult morbidity and mortality related to cardiovascular and other chronic diseases.1-3 Increased risk persists even if adolescents who were obese had lost the excess weight during adulthood, suggesting that obesity during adolescence sets triggers that are associated with risk of diseases in adulthood (level II evidence).23
A meta-analysis (level I evidence) by Goran24 showed that childhood obesity is a strong predictor of adulthood obesity. About 33% of obese preschool-aged children and 50% of obese school-aged children remained obese as adults. Risk of adult obesity was greater in both obese and nonobese children if at least one parent was overweight. This effect was most pronounced for children younger than 10 years; for children older than 10 years, their own overweight or obesity status was a better predictor than parental obesity (level II evidence).25
Overweight and obese children are at increased risk of a range of medical conditions affecting cardiovascular health (hypercholesterolemia, dyslipidemia, hypertension), the endocrine system (hyperinsulinism, insulin resistance, impaired glucose tolerance, type 2 diabetes mellitus, menstrual irregularity), the pulmonary system (asthma, obstructive sleep apnea syndrome, pickwickian syndrome), the musculoskeletal system (genu varum, slipped capital femoral epiphysis, Blount disease), and mental health (depression, low self-esteem, distorted body image, eating disorders).1-3 Risk factors for cardiovascular disease occur more frequently in overweight and obese children. Data from the Bogalusa Heart Study showed that 58% of overweight 5- to 17-year-old children had one cardiovascular risk factor or an elevated insulin level, and more than 25% had two or more risk factors (level II evidence).26 Newly diagnosed cases of type 2 diabetes mellitus increased from 4% in 1990 to 45% in 2001 in some populations of obese children aged 6 to 17 years.27 Impaired glucose tolerance, a prediabetic condition, is observed in 20% to 25% of obese children.28 Because these obesity-associated medical conditions can worsen if diagnosis is delayed, clinicians should be alert to these conditions in all obese pediatric patients.
Assessing pediatric obesity
Although the prevalence of childhood obesity has reached epidemic proportions, it is still underrecognized and undertreated. Medical evaluation of overweight and obese pediatric patients reportedly falls short of recommended practice.7
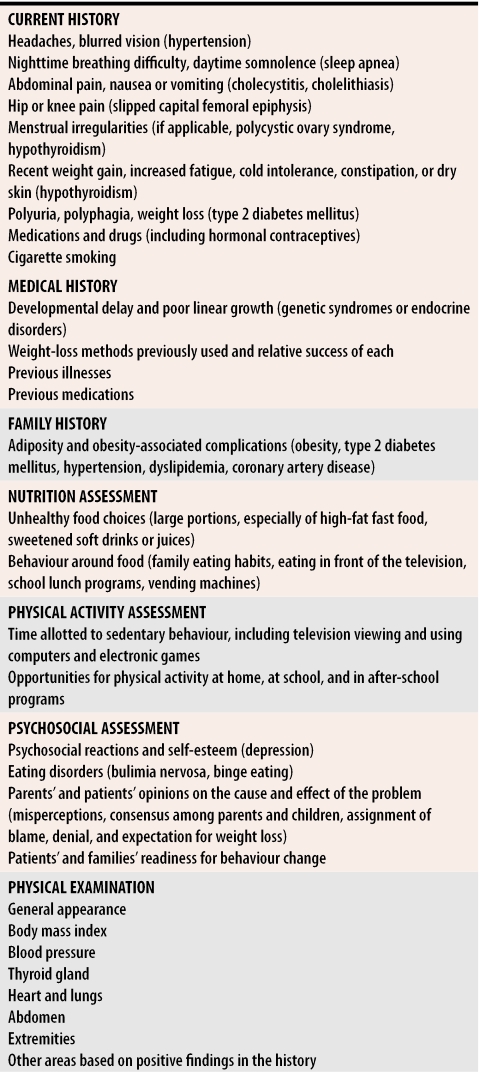
Initial assessment of an overweight child should include a history of gestational and linear growth as well as weight, age of onset of obesity, pubertal history (if applicable), and detailed histories of diet, physical activity, and psychosocial factors (level III evidence) (Table 22,3,29-32). A careful review should seek symptoms associated with congenital and endocrine causes and complications. Family history should focus on weight tendencies of family members and obesity-related complications in order to help predict greater risk for individual children.
Table 2. Recommendations for evaluating obese children.
Laboratory assessments (other than lipid profile, total cholesterol level, and a screening test for type 2 diabetes mellitus) are rarely useful except when findings from patient history or physical examination indicate specific tests.
Psychosocial factors are great predictors of whether weight management programs will be successful. If psychosocial assessment is not done before initiating a weight-loss program, the program is likely to fail due to poor compliance. Families not ready to make lifestyle changes are not in a position to support patients on weight-loss programs. Once children’s and families’ stage of readiness has been assessed, specific counseling techniques related to their stage of readiness for change can be integrated into weight-management programs (level III evidence).31
A full physical examination should focus on findings associated with symptoms of obesity identified by the history. Laboratory measurements should include lipid profile, total cholesterol level, and a screening test for type 2 diabetes mellitus. Other laboratory assessments are rarely useful unless they are specifically indicated by findings of history or examination (level III evidence).2 Initial follow-up, which should occur between 1 and 2 weeks after the first visit, should be used to review baseline laboratory findings with patients and families, to review the goals of the program, and to refer patients to other providers if indicated (level III evidence).2 Follow-up visits should be no more than 2 weeks apart until patients and families are comfortable with recommended changes. Intervals between visits can then be increased, and follow-up by telephone can be considered. Laboratory tests should be repeated in 6 months if results of initial tests are abnormal (level III evidence).2
Managing pediatric obesity
The goals of treatment are to find the energy balance that best promotes changes in body composition without interfering with normal growth and to teach children and their families about healthy eating and the benefits of physical activity.
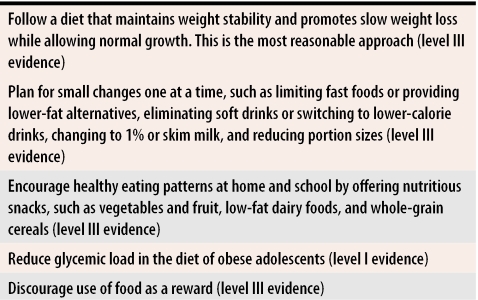
Diet.
Many pediatric patients’ diets do not meet recommended standards in terms of whole-grain cereals, fruit, vegetables, dairy products, and meat or meat alternatives and, therefore, do not provide sufficient key vitamins and minerals.33 Table 321,29,30,33,34 presents recommendations for helping patients acquire healthy eating habits.
Table 3.
Recommendations for physicians to use in nutrition interventions
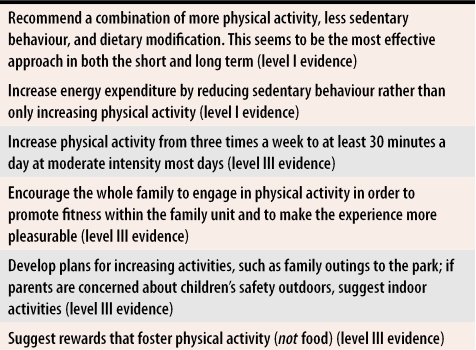
Physical activity.
Children’s interest in exercise and sports should be explored along with their body-image goals, and discussions should emphasize improving body composition, aerobic fitness, and muscle strength (level III evidence). The goal is to reduce sedentary activity and encourage physical activity. Table 435-38 presents recommendations for increasing physical activity.
Table 4.
Recommendations for physicians to use in physical activity interventions
Family-based behavioural treatment.
Approaches are based on the assumption that the family provides the main social learning environment for children, through modeling, feedback, and instruction on appropriate eating and physical activity habits.39-41 Family-based interventions can involve both parents and children or parents alone. Family-based interventions targeting parents and children have shown that changes in parents’ weight are a great predictor of changes in children’s weight (level I evidence).40 There is also evidence that treating childhood obesity with parents as the exclusive agents of change gets good results. A study looked at 60 obese children aged 6 to 11 years who were randomized to either an intervention group where only parents attended group sessions or a control group where only children attended group sessions and were followed for 1 year (level I evidence).39 Results revealed significant differences between groups in eating habits and a greater reduction in weight in the intervention group. The drop-out rate was nine times higher in the control group than in the intervention group.39 A 7-year follow-up of these children revealed that reduction in percentage overweight was greater among children in the intervention group than among those in the control group.41 These results provide strong evidence to support the role of parents in preventing and treating weight-related problems among children.
Pharmacologic intervention.
The two medications currently approved by the United States Food and Drug Administration for adolescents older than 16 years are sibutramine and orlistat. Sibutramine acts centrally in the hypothalamus on serotonin and norepinephrine pathways to affect appetite; orlistat, which is not absorbed, acts in the gut to inhibit pancreatic lipase, thereby decreasing fat absorption by about 30%. As with other aspects of obesity treatment, both medications require substantial lifestyle changes to ensure their efficacy.42 Safety and efficacy data on these drugs are unavailable, so they are not approved for pediatric use (level III evidence).
Bariatric surgery.
Surgical approaches have been used for morbidly obese adolescents older than 15 years, but are clearly not appropriate for many patients. Adolescents contemplating gastric bypass surgery should undergo extensive evaluation by a multidisciplinary team for medical, psychological, and nutritional screening before surgery. Bypass surgery revealed such complications as iron and vitamin D deficiency, cholelithiasis, protein-calorie malnutrition, wound infection, peritonitis, gastric rupture, and even death.43
Multidisciplinary approach.
Mild uncomplicated obesity can usually be managed in primary physicians’ offices. Patients presenting with obesity-associated comorbidity require more intensive treatment. Treatment plans should be formulated by multidisciplinary teams, and close medical follow-up should involve physicians, dietitians, exercise physiologists, health educators, social workers, and psychologists. Treatment plans should include specialized therapy regimens that allow children to grow normally (level III evidence).2,3
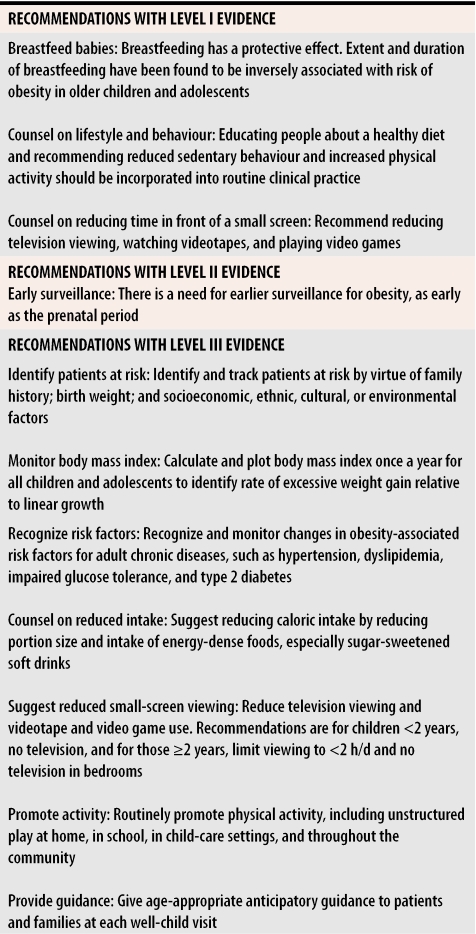
Family physicians’ role
Because pediatric obesity is increasing at epidemic rates1-3,5 and is accompanied by health problems, it is important to identify it in primary care and to understand the factors that lead to excess weight gain. Table 52,3,29,44-47 lists ways family physicians can help reverse this epidemic.
Table 5.
Recommendations for prevention and health supervision
Family physicians can play an important role in prevention and treatment of pediatric obesity by addressing five targets.
Encourage breastfeeding: Breastfeeding has a protective effect against childhood obesity (level I evidence).44
Suggest limiting television viewing: Current recommendations suggest limiting television time (level I evidence).18 Children younger than 2 years should watch no television and those 2 years and older should watch less than 2 hours a day and not have television sets in their bedrooms (level III evidence).1,2,46
Recommend reducing caloric intake: Reduce portion sizes and intake of energy-dense foods (level III evidence),21,22,29,44-46 especially sugar-sweetened soft drinks (level I evidence).34
Encourage physical activity: Increasing energy expenditure by decreasing children’s sedentary behaviour and increasing physical activity levels is likely to reduce pediatric obesity (level I evidence).35,36
Get parents onside: Evidence confirms the role of parents in preventing and treating weight-related problems in children (level I evidence).39,41
Studies have not confirmed the effectiveness of family physicians’ addressing these targets, but do suggest that incorporating these targets into routine clinical practice is beneficial (level II evidence).31,32,48-50
Conclusion
Considering that more than 25% of Canadian children aged 7 to 13 years are overweight or obese, we need widespread preventive efforts to ensure they do not face increased risk of problems later in adolescence or adulthood. Expert opinion suggests that prevention and treatment of pediatric obesity should involve patients, parents, families, and the entire community.7 Pediatric obesity should be a public health priority, and we should join forces across disciplines (eg, the media, food organizations, schools, and government) to mount an effective public health campaign for prevention and early treatment of obesity. Family physicians are often the first medical practitioners to see obese pediatric patients and are well placed to help prevent and manage the condition.
Levels of evidence.
Level I: At least one properly conducted randomized controlled trial, systematic review, or meta-analysis
Level II: Other comparison trials, non-randomized, cohort, case-control, or epidemiologic studies, and preferably more than one study
Level III: Expert opinion or consensus statements
Biography
Dr Plourde is doing research in the Department of Social and Preventive Medicine in the Division of Kinesiology at Laval University in Quebec city, Que.
Footnotes
Competing interests: None declared
References
- 1.Lobstein T, Baur L, Uauy R. for the International Association for the Study of Obesity of the International Obesity Task Force. Obesity in children and young people: a crisis in public health. Obes Rev. pp. 4–104. [DOI] [PubMed]
- 2.Eissa MA, Gunner KB. Practice guidelines: evaluation and management of obesity in children and adolescents. J Pediatr Health Care. 2004;18:35–38. doi: 10.1016/j.pedhc.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Elliott MA, Copperman NM, Jacobson MS. Pediatric obesity prevention and management. Minerva Pediatr. pp. 265–276. [PubMed]
- 4.Willms JD, Tremblay MS, Katzmarzyk PT. Geographic and demographic variation in the prevalence of overweight Canadian children. Obes Res. 2003;11:668–673. doi: 10.1038/oby.2003.95. [DOI] [PubMed] [Google Scholar]
- 5.De Onis M, Blossner M. Prevalence and trends of overweight among pre-school children in developing countries. Am J Clin Nutr. pp. 1032–1039. [DOI] [PubMed]
- 6.O’Brien SH, Holubkov R, Reis EC. [cited 2006 Jan 25];Identification, evaluation, and management of obesity in an academic primary care center. 2004 114:154–159. doi: 10.1542/peds.114.2.e154. Available from: http://pediatrics.aappublications.org/cgi/content/full/114/2/e154. [DOI] [PubMed]
- 7.Willms JD. Early childhood obesity: a call for surveillance and preventive measures. CMAJ. 2004;171:243–244. doi: 10.1503/cmaj.1040938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation in Geneva, 3-5 Jun 1997. Geneva, Switz: World Health Organization; 1998. [PubMed] [Google Scholar]
- 9.Grummer-Strawn LM, Mei Z. [cited 2006 Jan 25];Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. 2004 113:81–86. doi: 10.1542/peds.113.2.e81. Available from: http://pediatrics.aappublications.org/cgi/content/full/113/2/e81. [DOI] [PubMed]
- 10.Binns HJ, Ariza AJ. Guidelines help clinicians identify risk factors for overweight in children. Pediatr Ann. pp. 18–22. [DOI] [PubMed]
- 11.Snyder EE, Walts B, Perusse L, Chagnon YC, Weisnagel SJ, Rankinen T, et al. The human obesity gene map: the 2003 update. Obes Res. pp. 369–439. [DOI] [PubMed]
- 12.Skinner JD, Bounds W, Carruth BR, Morris M, Ziegler P. Predictors of children’s body mass index: a longitudinal study of diet and growth in children aged 2 to 8 y. Int J Obes Relat Metab Disord. pp. 476–482. [DOI] [PubMed]
- 13.Seidman DS, Laor A, Gale R, Stevenson DK, Danon YL. A longitudinal study of birth weight and being overweight in late adolescence. Am J Dis Child. 1991;145:782–785. [PubMed] [Google Scholar]
- 14.Tremblay MS, Willms JD. Is the Canadian childhood obesity epidemic related to physical inactivity? Int J Obes Relat Metab Disord. pp. 1100–1105. [DOI] [PubMed]
- 15.Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States, 1986-1990. Arch Pediatr Adolesc Med. pp. 356–362. [DOI] [PubMed]
- 16.Dennisson BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109:1028–1035. doi: 10.1542/peds.109.6.1028. [DOI] [PubMed] [Google Scholar]
- 17.Robinson T. Reducing children’s television viewing to prevent obesity: a randomised controlled trial. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 18.Berkey CS, Rockett HR, Field AE, Gillman MW, Frazier AL, Camargo CA, Jr, et al. [cited 2006 Jan 25];Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. 2000 105:56–65. doi: 10.1542/peds.105.4.e56. Available from: http://pediatrics.aappublications.org/cgi/content/full/105/4/e56. [DOI] [PubMed]
- 19.National Institutes of Health, National Heart, Lung, and Blood Institute. National Cholesterol Education Program 1991 Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. NIH Publication No. 91-2732. Bethesda, Md: US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute; 1991. [Google Scholar]
- 20.Cavadini C, Siega-Riz AM, Popkin BM. US adolescent food intake trends from 1965 to 1996. Arch Dis Child. pp. 18–24. [DOI] [PMC free article] [PubMed]
- 21.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–508. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 22.St-Onge MP, Keller KL, Heymsfield SB. Changes in childhood food consumption patterns: a cause for concern in light of increasing body weights. Am J Clin Nutr. pp. 1068–1073. [DOI] [PubMed]
- 23.Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med. pp. 1350–1355. [DOI] [PubMed]
- 24.Goran MI. Metabolic precursors and effects of obesity in children: a decade of progress, 1990-1999. Am J Clin Nutr. pp. 158–171. [DOI] [PubMed]
- 25.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. pp. 869–873. [DOI] [PubMed]
- 26.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 27.Goran MI, Ball GD, Cruz ML. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab. pp. 1417–1427. [DOI] [PubMed]
- 28.Sinha R, Fisch G, Teague B, Tamborlane WV, Banyas B, Allen K, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med. pp. 802–810. [DOI] [PubMed]
- 29.American Academy of Pediatrics. Policy statement. Committee on Nutrition. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 30.Barlow SE, Dietz WH. [cited 2006 Jan 25];Obesity evaluation and treatment: Expert Committee recommendations [The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services]. 102:29. doi: 10.1542/peds.102.3.e29. Available from: http://pediatrics.aappublications.org/cgi/content/full/102/3/e29. [DOI] [PubMed]
- 31.Plourde G. Treating obesity; lost cause or new opportunity? Can Fam Physician. 2000;46:1806–1813. [PMC free article] [PubMed] [Google Scholar]
- 32.Etelson D, Brand DA, Patrick PA, Shirali A. Childhood obesity: do parents recognize this health risk? Obes Res. pp. 1362–1368. [DOI] [PubMed]
- 33.Wright JD, Wang CY, Kennedy-Stephenson J, Ervin RB. Dietary intake of ten key nutrients for public health, United States: 1999–2000. J Clin Endocrinol Metab. 2004;89:2540–2547. [Google Scholar]
- 34.Ebbeling CB, Leidig MM, Sinclair KB, Hangen JP, Ludwig DS. A reduced-glycemic load diet in the treatment of adolescent obesity. Arch Pediatr Adolesc Med. pp. 773–779. [DOI] [PubMed]
- 35.Epstein LH, Paluch RA, Gordy CC, Dom J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. pp. 220–226. [DOI] [PubMed]
- 36.Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioural-physical activity intervention for the treatment of childhood obesity. Pediatrics. 2005;115:443–449. doi: 10.1542/peds.2004-2172. [DOI] [PubMed] [Google Scholar]
- 37.Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. pp. 409–418. [DOI] [PubMed]
- 38.Epstein LH, Goldfield GS. Physical activity in the treatment of childhood overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. pp. 553–559. [DOI] [PubMed]
- 39.Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. Am J Clin Nutr. pp. 1130–1135. [DOI] [PubMed]
- 40.Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med. 2004;158:342–347. doi: 10.1001/archpedi.158.4.342. [DOI] [PubMed] [Google Scholar]
- 41.Golan M, Crow S. Targeting parents exclusively in the treatment of childhood obesity: long-term results. Obes Res. pp. 357–361. [DOI] [PubMed]
- 42.Phelan S, Wadden TA. Combining behavioural and pharmacologic treatments of obesity. Obes Res. pp. 560–574. [DOI] [PubMed]
- 43.Inge TH, Garcia V, Daniels S, Langford L, Kirk S, Roehrig H, et al. A multidisciplinary approach to the adolescent bariatric surgical patient. J Pediatr Surg. pp. 442–447. [DOI] [PubMed]
- 44.Gillman MW, Rifas-Shiman SL, Camargo CA, Jr, Berkey CS, Frazier AL, Rockett HR, et al. Risk of overweight among adolescents who were breastfed as infants. JAMA. 2001;285:2461–2467. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- 45.Campbell K, Waters E, O’Meara S, Summerbell C. Interventions for preventing obesity in childhood. A systematic review. Obes Rev. pp. 149–157. [DOI] [PubMed]
- 46.Whitaker RC. Obesity prevention in pediatric primary care. Four behaviours to target. Arch Pediatr Adolesc Med. pp. 725–726. [DOI] [PubMed]
- 47.Dennisson BA, Boyer PS. Risk evaluation in pediatric practice aids in prevention of childhood overweight. Pediatr Ann. pp. 25–30. [DOI] [PubMed]
- 48.Nawaz H, Adams ML, Katz DL. Physician-patient interactions regarding, diet, exercise, and smoking. Prev Med. pp. 652–657. [DOI] [PubMed]
- 49.Calfas KJ, Long BJ, Sallis JF, Wooten WJ, Pratt M, Patrick K. A controlled trial of physician counselling to promote the adoption of physical activity. Prev Med. pp. 225–233. [DOI] [PubMed]
- 50.Lu MC, Lange L, Slusser W, Hamilton J, Halfon N. Provider encouragement of breast-feeding: evidence from a national survey. Obstet Gynecol. 2001;97:290–295. doi: 10.1016/s0029-7844(00)01116-9. [DOI] [PubMed] [Google Scholar]