It is important for family physicians to understand the role of rheumatoid factor (RF) in management of patients with rheumatoid arthritis (RA).
Rheumatoid factors are antibodies that recognize the Fc portion of IgG molecules as their antigens; RFs can be of any immunoglobulin isotype (IgM, IgG, IgE). Most of the RFs measured clinically are IgM RFs. Rheumatoid factors probably developed in humans as a mechanism for helping remove immune complexes from the circulatory system.
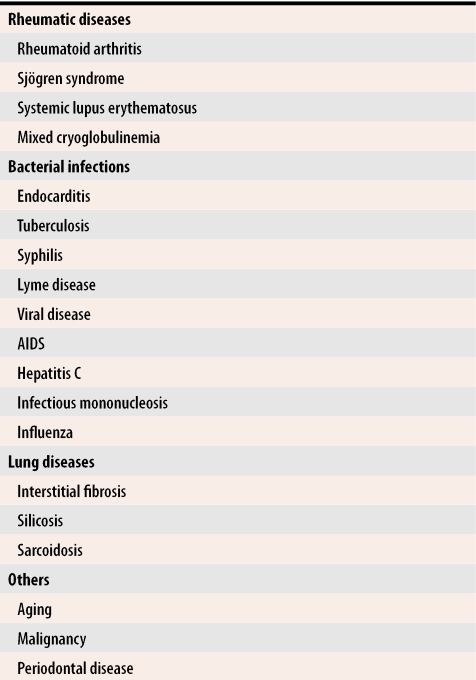
Many conditions associated with chronic inflammation are also associated with RF (Table 1). Incidence and titre increase with age. By age 70, up to 14% of the population will test positive for RF.1
Table 1.
Some diseases associated with testing positive for rheumatoid factor
Testing for RF is not a screening test for RA in patients with musculoskeletal pain without joint swelling. The predictive value of a test for RA depends on the sensitivity and specificity of the test and the pretest probability of RA. Because RF is present in numerous conditions other than RA, its specificity is limited; because RF is not present in all patients with RA, sensitivity is also reduced. In patients with diffuse musculoskeletal pain without joint swelling, the predictive value of the test is about 16%. In patients with a high pretest probability of RA (ie, those with symmetric polyarticular joint swelling), the predictive value of the RF factor increases to 80%.
For patients with RA, RF is an important predictor of poor prognosis.2 In high titres it portends increased joint erosion, extra-articular manifestations, and greater disability. Rheumatoid factor deposited in tissue is responsible for the formation of rheumatoid nodules. About 70% of RA patients test positive for RF at onset of RA, and 85% become positive during the first 2 years of the disease. Serum levels of RF do not change rapidly and cannot be used to follow disease activity.
Bottom line
Do not test for RF unless you have a high index of suspicion that a patient is suffering from RA.
Once a diagnosis of RA is made, you cannot use RF to monitor the effect of treatment, but it does have some value in predicting the future course of the disease.
“Just the Berries” for Family Physicians originated at St Martha’s Regional Hospital in 1991 as a newsletter for members of the Department of Family Medicine. Its purpose was to provide useful, practical, and current information to busy family physicians. It is now distributed by the Medical Society of Nova Scotia to all family physicians in Nova Scotia. Topics discussed are suggested by family physicians, and in many cases, articles are researched and written by family physicians.
Acknowledgments
I thank Dr Juris Lazovskis, a rheumatologist at the Cape Breton Regional Health Centre in Sydney, NS, for reviewing the draft copy of this article.
Biography
Dr Wilson is a community-based rheumatologist with a strong interest in continuing medical education. She works in Lunenberg, NS.
References
- 1.Mikkelson WM, Dodge HJ, Duff I, Kato H. Estimates of the prevalence of the rheumatic disease in the populations of Tecumseh, Michigan, 1959-60. J Chron Dis. 1967;20:351–369. doi: 10.1016/0021-9681(67)90009-4. [DOI] [PubMed] [Google Scholar]
- 2.Koopman WJ. Arthritis and allied conditions. 14th ed. Baltimore, Md: Lippincott Williams and Wilkins; 2001. [Google Scholar]