Abstract
OBJECTIVE
To determine whether rural family physicians thought they had received enough months of rural exposure during family medicine residency, how many months of rural exposure those who were satisfied with their training had had, and how many months of rural exposure those who were not satisfied with their training wanted.
DESIGN
Mailed survey.
SETTING
Rural Canada.
PARTICIPANTS
Rural family physicians who had graduated between 1991 and 2000 from a Canadian medical school.
MAIN OUTCOME MEASURES
Respondents’ opinions about whether their exposure to rural medicine during training had been adequate.
RESULTS
Response rate was 59% (382/651). After excluding physicians who had not had Canadian family medicine residency training, 348 physicians remained, and of those, 58% thought they had had adequate rural exposure during residency. Median duration of rural training among those who thought they had had enough rural exposure was 6 months; median duration of rural exposure among those who thought they had not had enough was 2 months. Median duration of rural exposure desired by those who thought they had not had enough rural training was 6 months. Some physicians wanted much more than 6 months of rural training; for example, one quarter of those satisfied with their rural training had had 10 or more months of rural rotations. Fewer than 1% of respondents thought they had received too much rural training. There was no significant difference in number of months of rural training preferred by men and women (P = .94). One third of respondents had graduated from rural-focused family practice residency programs. Rural program graduates were more likely than non–rural program graduates to report that the duration of their rural training was adequate (84% vs 46%, P < .0001) and to report more mean months of rural exposure (8.9 vs 3.4; P < .0001).
CONCLUSION
Typical rural family physicians prefer to have 6 months of rural exposure during residency. This finding is consistent with the recommendation of a College of Family Physicians of Canada committee that rural family medicine training programs offer at least 6 months of rural rotations. Almost half of rural family physicians wished they had had more rural training. Both rural-focused and non–rural-focused programs should consider providing opportunities for pursuing elective rotations in rural areas in addition to mandatory rotations if they want to respond to these preferences for training.
Abstract
OBJECTIF
Déterminer si les médecins de famille ruraux croyaient avoir reçu un nombre suffisant de mois d’exposition à la médecine rurale durant leur résidence en médecine familiale, le nombre de mois d’exposition rurale dont avaient bénéficié ceux qui étaient satisfaits et celui qu’auraient souhaité ceux qui n’étaient pas satisfaits de leur formation.
TYPE D’ÉTUDE
Enquête postale
CONTEXTE
Régions rurales canadiennes
PARTICIPANTS
Médecins de famille ruraux diplômés de facultés de médecine canadiennes entre 1991 et 2000.
PRINCIPAL PARAMÈTRE À L’ÉTUDE
Opinion des répondants, à savoir si leur exposition à la médecine rurale durant leur formation avait été satisfaisante.
RÉSULTATS
Le taux de réponse était de 59 % (382/651). Des 348 médecins retenus après exclusion de ceux qui n’avaient pas fait leur résidence en médecine familiale au Canada, 58 % jugeaient avoir eu une formation rurale adéquate durant leur résidence. Pour ces derniers, la durée médiane de la formation avait été de 6 mois, alors qu’elle était de 2 mois pour ceux qui estimaient n’avoir pas eu une formation suffisante. Pour ceux qui ne croyaient pas avoir eu assez de formation rurale, la durée médiane qu’ils auraient souhaitée était de 6 mois. Certains médecins auraient souhaité beaucoup plus que cela; par exemple, le quart de ceux qui avaient eu une formation rurale satisfaisante avaient eu 10 mois ou plus de stages ruraux. Moins de 1% des répondants estimaient avoir eu trop de formation rurale. Il n’y avait pas de différence significative entre les hommes et les femmes pour le nombre de mois de formation rurale souhaité (P = 0,94). Le tiers des répondants étaient issus de programmes de résidence en médecine familiale axés sur les régions rurales. Par rapport aux diplômés des programmes non ruraux, ceux qui provenaient des programmes ruraux étaient plus susceptibles de déclarer avoir reçu une durée de formation rurale adéquate (84 % vs 46 %, P < 0,0001) et d’avoir eu plus de mois d’exposition rurale en moyenne (8,9 vs 3,4; P < 0,0001).
CONCLUSION
Le médecin de famille rural typique préfère une durée de formation rurale de 6 mois durant sa résidence. Cela concorde avec la recommandation d’un comité du Collège des médecins de famille du Canada qui suggérait que les programmes de formation en médecine familiale rurale doivent offrir au moins 6 mois de stages en milieu rural. Près de la moitié des médecins de famille ruraux auraient souhaité avoir plus de formation rurale. Qu’ils soient ou non axés sur la médecine rurale, les programmes de formation devraient offrir, outre les stages obligatoires, la possibilité de stages optionnels en région rurale afin de mieux répondre aux vœux des stagiaires.
EDITOR’S KEY POINTS.
Rural areas in Canada suffer from a chronic shortage of physicians. One key strategy employed in Canada, the United States, and Australia to address this problem has been to establish rural-focused training programs, particularly at the postgraduate level.
This study examines whether rural physicians thought they had had sufficient exposure to rural medicine during residency.
Six months was the median duration of rural training of those who thought they had had enough rural exposure, and was also the median length of rural training desired by those who thought they had not had enough rural exposure.
POINTS DE REPÈRE DU RÉDACTEUR.
Il existe une pénurie chronique de médecins dans les régions rurales au Canada. Une des mesures clés utilisées au Canada, aux États-Unis et en Australie pour corriger cette situation a consisté à créer des programmes de formation axés sur les milieux ruraux, notamment au niveau post-universitaire.
Cette étude voulait déterminer si les médecins ruraux croyaient avoir reçu une exposition suffisante à la médecine rurale au cours de leur résidence.
La durée médiane de la formation rurale pour les médecins qui croyaient avoir eu une formation rurale suffisante était de 6 mois, et c’était aussi la durée médiane qu’auraient souhaitée ceux qui estimaient n’avoir pas eu une exposition suffisante.
Canada suffers from a chronic rural-urban maldistribution of physicians.1 One key strategy employed in Canada,2-4 the United States,5,6 and Australia7 to address this problem has been to establish rural-focused training programs, particularly at the postgraduate level. These programs conduct a portion of residency training in rural communities and have relatively high rates of placement of graduates into rural areas.8,9
Questions remain, however, about the ideal duration of rural exposure during training. Our previous research in 2002 demonstrated wide variation among the 12 rural residency programs in Canada in minimum standards for duration of rural training, from 4 to 12 months within the 2-year curriculum.4 The advantage of rural rotations is that prospective physicians can gain clinical experience in environments with little or no immediate specialist backup, meet rural mentors, develop rural social networks, visit communities where they might want to work in the future, and gain an appreciation of rural lifestyles. Urban rotations, on the other hand, offer more intense exposure to specialty medicine, advanced diagnostic equipment, and rare pathologies; provide opportunities for developing links with specialists; and allow residents to observe the care given to rural patients who are referred to large urban centres.
In 1999, the College of Family Physicians of Canada (CFPC) sponsored a consensus panel on rural education that recommended a minimum of 6 months’ rural exposure during residency.10 This recommendation was based on the expert opinion of panel members and not on any empirical evidence. The effect of this recommendation appears to be limited. Our 2002 review of rural training programs 3 years after the recommendation4 showed that the CFPC guidelines had not led to consensus on minimum rural training requirements for Canadian residency programs. Further, Canadian guidelines differ from those of the American Academy of Family Physicians where a program with as few as 3 rurally located block months can qualify for designation as a “rural training program in family medicine.”11
This study examines whether rural physicians thought they had had sufficient exposure to rural medicine during residency, and whether recently graduated rural physicians’ self-reported preferences for duration of rural exposure during postgraduate training are consistent with CFPC guidelines and with the amount of rural training actually offered by residency programs. A mismatch between preferences for duration of rural training and either the expert recommendations or the actual training offered would suggest that current recommended or actual rural training times need to be modified.
METHODS
We surveyed all Canadian family physicians and general practitioners who had graduated between 1991 and 2000 from Canadian medical schools and were practising in 2002 in rural areas or small towns, as defined by Statistics Canada.12 This includes towns with populations of up to 10 000 people that are outside the commuting zone of larger urban centres. Potential respondents were identified from the Southam Medical Database and were sent the questionnaire. A French version of the questionnaire was sent to physicians in Quebec and Francophone physicians in New Brunswick. Physicians received two mailings and a reminder card in between. A third mailing was sent to regions where the response rate remained below 50% after the initial mailings.
Questions of interest included the following.
How many months did you spend doing rural rotations during your 2-year residency?
Do you think that this was the right amount of exposure to make you feel comfortable practising in rural areas?
How many months of rural rotations do you believe is ideal? (Respondents answered this question only if they thought they had not received the right amount of rural exposure.)
The study received ethics approval from Sunnybrook and Women’s College Health Sciences Centre.
In the analysis, we excluded physicians who had not completed a 2-year family medicine residency in Canada. We used bivariate analytic methods (t tests and continuity-adjusted chi-square tests) to examine differences in responses to these questions by whether or not respondents attended rural-focused family medicine residency programs. These programs were identified through a separate telephone survey of family medicine residency program directors.4
RESULTS
Of the 784 physicians surveyed, 133 were ineligible for various reasons (eg, invalid address or not in rural family medicine). Completed and eligible questionnaires made up an effective response rate of 59% (382/651). After excluding physicians who had not had Canadian family medicine residency training, 348 physicians (91% of respondents) remained. Mean age of physicians in the final sample was 34 years; 61% were female. Respondents had, on average, 5.3 months of rural rotations.
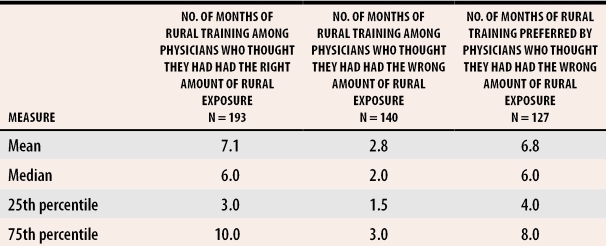
Overall, 58% of respondents thought they had had the right amount of rural exposure during residency training. Those who thought they had had enough rural exposure had spent a median of 6 months in rural training; 6 months was also the median duration of rural training desired by those who thought they had not had enough exposure. Distributions of both responses were skewed to the right; mean preferred training times were greater than median preferred times (Table 1). Fewer than 1% of respondents reported that they had received too much rural training. There was no significant difference in number of months of rural training preferred by men and women (P = .94).
Table 1. Number of months of rural training preferred and undertaken by rural family physicians.
Fifteen physicians did not respond to the question on months of rural training, and an additional 13 physicians who thought they had had the wrong amount of exposure did not report their preferred duration of rural training.
Overall, 33% of respondents had graduated from rural-focused family practice residency programs. Of those who reported having had adequate rural exposure, 47% had graduated from rural-focused programs; of those reporting having had inadequate rural exposure, only 13% had graduated from rural-focused programs. Rural program graduates were more likely than non–rural program graduates to report that the amount of rural training they had received was adequate (84% vs 46%, P < .0001) and that they had had more mean months of rural exposure (8.9 vs 3.4, P < .0001).
DISCUSSION
This study suggests that 6 months of a 2-year family medicine residency program is the preferred duration of rural exposure for typical rural family physicians. This is precisely the minimum length of time recommended by the CFPC’s consensus panel10 based on expert opinion. This study now provides evidence to support the recommendation. Six months is twice the minimum duration recommended by the American Academy of Family Physicians (AAFP). Further research is needed to confirm whether results of this study are generalizable to the United States. If so, perhaps policies should reflect residents’ training preferences. In Canada, two of the 12 rural programs have a minimum duration of rural training of 4 months,4 which is shorter than the stated preference for rural training. Results of this study suggest that program directors should consider adjusting the minimum duration of rural training in their programs to conform with the CFPC standard.
We found that the mean preferred duration of training is greater than the median preferred duration and that there was considerable variation in preference for duration of rural training. Nine of the 12 rural programs offered the option of completing at least 12 months of rural training in total. This option would appear to meet the demands of almost all rural physicians. Two of the 12 programs offered the option of completing 6 to 9 months of rural rotations. Given that one quarter of those who thought they had had adequate rural training did 10 or more months of rural rotations, these programs might wish to consider adjusting the total months of elective and mandatory rural rotations available.
Although this study demonstrates some room for improvement in rural-focused programs to meet rural physicians’ expectations for training, a greater problem exists in non–rural-focused programs. More than half of non–rural program graduates thought they had had inadequate rural training, compared with one in six rural program graduates. Although non–rural programs might not need to have stringent minimum standards for rural training, they might be able to accommodate the needs of rural physicians by offering greater flexibility to do rural electives. Among the eight non–rural programs, two offered a maximum of 4 months of rural training, two offered 5 months, and three offered 6 months.4 Because the number of rural training programs has increased in recent years,4 physicians interested in rural medicine might not need to train in non–rural-focused programs to the extent they did in the past. Greater flexibility to do rural training in non–rural programs might still be beneficial, however, particularly for physicians who realize only in the midst of their postgraduate training that they wish to do rural medicine.
Limitations
This study has some important limitations. First, it surveyed physicians who graduated anywhere from 2 to 11 years before so results might have been affected by recall bias. We found no notable differences in preferences for duration of training by graduation year, however. Second, this study examines only rural physicians’ preferences for training and not whether clinical skills vary by length of rural training. Such a consideration might be more important than preferences when setting benchmarks for length of training.
Conclusion
Typical rural family physicians prefer 6 months of rural rotations during residency. This finding is consistent with the current CFPC recommendation that rural family medicine training programs offer at least 6 months of rural rotations. There was wide variation in the number of months of rural rotations preferred, and almost half the respondents wished they had had more rural training. Both rural-focused and non–rural-focused programs should consider providing adequate opportunities for pursuing elective rotations in rural areas if they want to respond to rural physicians’ preferences for duration of rural training.
Acknowledgments
We gratefully acknowledge funding for this study from the Canadian Institutes of Health Research grant no. 54126.
Biography
Dr Chan was a Senior Scientist at the Institute for Clinical Evaluative Sciences in Toronto, Ont, and an Assistant Professor in the Faculty of Medicine at the University of Toronto at the time of the study. He is now Chief Executive Officer of the Health Quality Council in Saskatoon, Sask, and is an Adjunct Professor in the College of Medicine at the University of Saskatchewan. Ms Degani was a Research Coordinator at the Institute for Clinical Evaluative Sciences at the time of the study. Dr Crichton teaches in the North Eastern Ontario Family Medicine Program at the University of Ottawa. Dr Pong is on staff in the Centre for Rural and Northern Health Research at Laurentian University in Sudbury, Ont. Dr Rourke teaches in the Southwestern Ontario Rural Medicine Unit in the Faculty of Medicine and Dentistry at the University of Western Ontario in London and is Dean of the Faculty of Medicine at Memorial University of Newfoundland in St John’s. Dr Goertzen and Dr McCready teach in the Northwestern Ontario Medical Programme in the Faculty of Health Sciences at McMaster University in Hamilton.
Footnotes
Competing interests: None declared
References
- 1.Commission on the Future of Health Care in Canada, RJ Romanow (commissioner) Building on values: the future of health care in Canada. Final report. Catalogue no. CP32-85/2002E-IN. Ottawa, Ont: Government of Canada; 2002. [Google Scholar]
- 2.Moores DG, Woodhead-Lyons SC, Wilson DR. Preparing for rural practice. Enhanced experience for medical students and residents. Can Fam Physician. 1998;44:1045–1050. [PMC free article] [PubMed] [Google Scholar]
- 3.Gray JD, Steeves LC, Blackburn JW. The Dalhousie University experience of training residents in many small communities. Acad Med. 1994;69(10):847–851. doi: 10.1097/00001888-199410000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Krupa LK, Chan BT. Canadian rural family medicine training programs. Growth and variation in recruitment. Can Fam Physician. 2005;51:852–853. [PMC free article] [PubMed] [Google Scholar]
- 5.Stearns JA, Stearns MA. Graduate medical education for rural physicians: curriculum and retention. J Rural Health. 2000;16(3):273–277. doi: 10.1111/j.1748-0361.2000.tb00472.x. [DOI] [PubMed] [Google Scholar]
- 6.Schwarz MR. The WAMI Program: 25 years later. Med Teach. 2004;26(3):211–214. doi: 10.1080/01421590410001696416. [DOI] [PubMed] [Google Scholar]
- 7.Rourke JT, Strasser R. Education for rural practice in Canada and Australia. Acad Med. 1996;71(5):464–469. doi: 10.1097/00001888-199605000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Acosta DA. Impact of rural training on physician work force: the role of postresidency education. J Rural Health. 2000;16(3):254–261. doi: 10.1111/j.1748-0361.2000.tb00469.x. [DOI] [PubMed] [Google Scholar]
- 9.Rosenthal TC, McGuigan MH, Anderson G. Rural residency tracks in family practice: graduate outcomes. Fam Med. 2000;32(3):174–177. [PubMed] [Google Scholar]
- 10.College of Family Physicians of Canada. Postgraduate education for rural family practice. Vision and recommendations for the new millennium. Mississauga, Ont: College of Family Physicians of Canada; 1999. [Google Scholar]
- 11.American Academy of Family Physicians. Rural residency, definition. Leawood, Kan: American Academy of Family Physicians; 2005. [cited 2005 April 6]. Available at: http://www.aafp.org/x25069.xml. [Google Scholar]
- 12.Statistics Canada. 1996 census dictionary. Catalogue no. 92-351-XRE. Ottawa, Ont: Statistics Canada; 1996. [Google Scholar]