Abstract
OBJECTIVE
To describe Canadian family physicians’ prescribing practices with regard to Alzheimer disease (AD).
DESIGN
Cross-sectional survey administered by facsimile.
SETTING
Four regions in Canada (British Columbia, the Prairie Provinces, Ontario, and the Atlantic Provinces).
PARTICIPANTS
A stratified random sample of 1000 Canadian family physicians (250 per region) chosen from the Canadian Medical Directory; 81 of whom were excluded as ineligible.
MAIN OUTCOME MEASURES
Prescribing practices regarding cholinesterase inhibitors (ChIs) for patients with AD.
RESULTS
Response rate was 36.3%. About 27% of respondents reported that ChIs were prescribed for less than 10% of their AD patients, while 12.5% reported that ChIs were prescribed for more than 90% of their AD patients. More physicians prescribed ChIs in the two regions with provincial formulary coverage (Prairie Provinces and Ontario) than in the two regions without coverage (British Columbia and Atlantic Provinces). Factors that significantly predicted lower prescribing rates included female sex, perception of ChIs’ effectiveness, and self-reported knowledge of ChIs.
CONCLUSION
Canadian physicians’ prescribing patterns for ChIs vary; the optimal prescribing rate is unclear. Provincial coverage of these drugs along with physicians’ sex, knowledge of ChIs, and perception of the effectiveness of ChIs appear to influence prescribing rates.
Abstract
OBJECTIF
Décrire les habitudes de prescription des médecins de famille canadiens en regard de la maladie d’Alzheimer (MA).
TYPE D’ÉTUDE
Enquête transversale par télécopie.
CONTEXTE
Quatre régions du Canada (Colombie Britannique, provinces des Prairies, Ontario et provinces Atlantiques).
PARTICIPANTS
Un échantillon stratifié de 1000 médecins de famille canadiens (250 par région) choisis à partir de l’Annuaire médical canadien; 81 d’entre eux n’étaient pas éligibles et ont été exclus.
PRINCIPAL PARAMÈTRE À L’ÉTUDE
Mode de prescription habituel des inhibiteurs de la cholinestérase (Ich) pour les patients atteints de la MA.
RÉSULTATS
Le taux de réponse était de 36,3%. Environ 27% des répondants déclaraient prescrire des ICh à moins de 10% de leurs patients MA, tandis que 12,5% en prescrivaient à plus de 90% de ces patients. Un plus grand nombre de médecins en prescrivaient dans les deux régions où ces médicaments étaient couverts par un régime provincial (provinces des Prairies et Ontario).Les principaux facteurs prédictifs d’un faible taux de prescription incluaient le sexe féminin, certains doutes sur l’efficacité des Ich et une connaissance insuffisante de ces agents.
CONCLUSION
Au Canada, la façon de prescrire les Ich varie selon les médecins; on ne connaît pas la façon idéale. Il semble que le taux de prescription est influencé par la présence d’une couverture provinciale pour ces médicaments, mais aussi par le sexe du médecin, sa connaissance des Ich et son opinion sur leur efficacité.
EDITOR’S KEY POINTS.
Prescribing cholinesterase inhibitors (ChIs) to patients with mild-to-moderate Alzheimer disease (AD) is recommended in recent guidelines, but there are concerns about the drugs’ effectiveness, side effects, and cost. This report describes how Canadian family doctors prescribe these medications.
Just over 25% of family doctors prescribe ChIs to <10% of their AD patients; almost 13% report prescribing them to >90% of their AD patients.
Prescribing frequency was higher in regions where the drug was covered under provincial formulary. Women physicians, those concerned about effectiveness, and those with less knowledge of ChIs prescribed them less frequently.
POINTS DE REPÈRE DU RÉDACTEUR.
Les plus récentes directives de pratique recommandent de prescrire des inhibiteurs de l’acétylcholinestérase (Ich) aux patients atteints d’une maladie d’Alzheimer (MA) d’intensité légère à modérée, mais certains s’interrogent sur l’efficacité, les effets indésirables et le coût de ces agents. Cet article décrit la façon dont les médecins de famille canadiens prescrivent ces médicaments.
Un peu plus de 25% des médecins de famille prescrivent des ICh à 10% de leurs patients MA; près de 13% déclarent en prescrire à plus de 90% de ces patients.
Le taux de prescription était plus élevé dans les régions où ces médicaments étaient couverts par un régime provincial. Ceux qui en prescrivaient le moins souvent étaient les femmes médecins et ceux qui doutaient de leur efficacité ou qui connaissaient moins bien ces agents.
The Canadian Study of Health and Aging estimated that 8% of Canadians older than 65 and 35% older than 85 suffer from dementia and projected that the prevalence of dementia will triple by the year 2030.1 Alzheimer disease (AD) is the most common cause of dementia; it accounts for about 60% of all cases of dementia in Canada. Until recently, no medications were available to treat AD.1 Since 1997, three acetylcholinesterase inhibitors (ChIs) have been licensed in Canada for treating patients with mild-to-moderate AD.
Several recent reviews of ChIs concluded that their use can result in modest improvements in global measures of change, cognition, activities of daily living, and neuropsychiatric symptoms (eg, motivation, agitation).2-8 Claims that ChIs can delay the need for nursing-home care are based on poorly controlled extrapolations from clinical trials.2 The recent AD2000 study of donepezil found short-term benefits in cognition and function, but no reduction in institutionalization or progression of disability after 3 years (although the confidence intervals were quite wide).9
Adverse events from ChIs include nausea, vomiting, diarrhea, abdominal pain, and insomnia, and occur in about 5% to 10% of patients.2-7 Adverse events might be avoided by slowly titrating the dose and are reversible with cessation of therapy.2
A recent meta-analysis by Lanctot and colleagues estimated that the number of AD patients needed to treat for one additional patient to benefit (ie, minimal improvement or better) was 12 (95% confidence interval [CI] 9 to 16), and the number needed to treat for one additional patient to experience an adverse event was 12 (95% CI 10 to 18).3 Clinical guidelines in Canada and the United States recommend the use of ChIs in informed and willing patients with mild to moderate AD, in the absence of contraindications.10,11 The Canadian guideline suggests that reasonable treatment goals include the following: slowing the course of the disease, stabilization or improvement in cognitive or functional abilities, improvement in mood or behaviour, or improvement in quality of life of the patient and caregiver.10 The guideline recommends that after initiation of treatment, the primary care physician should reassess the patient regularly, such as every 3 months, with input from caregivers, who should be encouraged to keep written records of their personal impressions of the performance of the patient, and with the use of standardized cognitive and functional status measurements.10
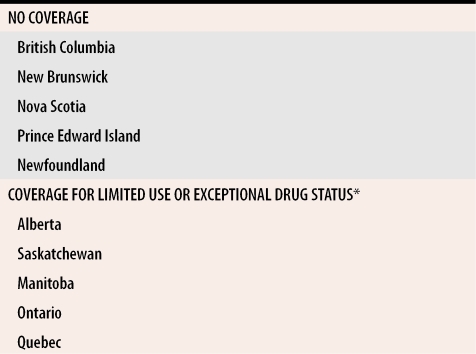
These drugs, however, are relatively expensive ($140/mo), so their cost-effectiveness remains in question because there is inadequate evidence that they have long-term benefits or improve quality of life.2,6 The status of ChIs on provincial drug formularies is different in various provinces (Table 1).
Table 1. Provincial coverage of acetylcholinesterase inhibitors.
Formulary status at the time of the survey (July 2002).
*Limited use or exceptional drug status are terms used in various provinces to denote medications covered under specific conditions (eg, in Ontario, cholinesterase inhibitors are covered for mild-to-moderate Alzheimer disease), but not routinely covered for everyone insured.
Family physicians are generally the first contact for patients needing treatment for AD. Decisions about whether to prescribe ChIs for individual patients can be complex because of the need to balance potential benefits against risks for these vulnerable patients whose cognitive impairment can interfere with adherence to medication regimens. Except for a small study in Quebec,12 Canadian family physicians’ prescribing practices for treatment of AD have not been formally studied. This study aims to describe these prescribing practices, to explore regional variation in prescribing practices, and to establish what determines whether ChIs are prescribed.
METHODS
Subjects
From a list of 29 113 practising family physicians in the Canadian Medical Directory (CD-ROM 2001 version), about 250 names were randomly selected from each of four Canadian regions: British Columbia, the Prairie Provinces (Alberta, Saskatchewan, Manitoba), Ontario, and the Atlantic Provinces (Nova Scotia, New Brunswick, Prince Edward Island, Newfoundland) for a total of 1000 names. The province of Quebec was excluded from the study because the questionnaire was available only in English. Demographic information, including age, sex, province of practice, and year of graduation, was obtained for each participating physician from the Canadian Medical Directory.
A letter introducing the study was printed in coloured ink13 and mailed to the 1000 physicians. The two-page survey was sent by facsimile 2 weeks after the letter. Nonrespondents received a second facsimile 2 weeks later. Remaining nonrespondents received a mailed survey with a postage-paid return envelope after 2 additional weeks. To ensure confidentiality, each questionnaire was numbered, and the number was linked to the physician’s name in a separate file used only to identify nonrespondents for the purpose of sending the questionnaire again. Identifying information transmitted by facsimile was removed by an administrative assistant immediately upon receipt of the questionnaire.
Questionnaire
A literature review and interviews with local experts in family medicine, pharmacy, geriatrics, and neurology helped the investigators select survey items. The comprehensive list of items was reviewed, edited, and simplified by the investigators, and the final questionnaire was pilot-tested on five family physicians in Toronto, Ont, for clarity and content validity. Minor revisions were made to the questionnaire based on feedback received from the pilot study.
Respondents were asked to report how frequently they prescribed ChIs for treatment of AD, their opinions about the effectiveness of ChIs and the most appropriate time to initiate these drugs, their approach to prescribing these drugs, the factors that might influence their prescribing practices with respect to AD, and their knowledge about use of ChIs for patients with AD. Information on physicians’ practices was collected also.
Data analysis
Simple means and proportions were computed for continuous and categorical variables. Proportions were compared using the Chi-square test. A logistic regression model was used to determine the effect of the following factors on how frequently ChIs were prescribed: physician’s sex, year of graduation, rural or urban location, affiliation with a long-term care facility, opinion of the effectiveness of ChIs, self-reported knowledge of ChIs, reported visit by a pharmaceutical representative to discuss ChIs, and coverage of ChIs on provincial formularies. These factors were chosen a priori because they were thought to be important. Physicians were given four choices for reporting the percentage of their AD patients taking ChIs: <10%, 10% to 50%, 51% to 90%, and >90%. Responses to this question were converted to a dichotomous variable with <10% representing low-frequency prescribing and ≥10% representing high-frequency prescribing. Goodness-of-fit of the regression model was tested using the Hosmer-Lemeshow statistic, with P values < .05 indicative of poor fit.14 The model’s discriminatory ability was assessed with the C statistic, with values >.50 indicating discriminative ability better than chance and a value of 1.0 indicating perfect discrimination.15 All analyses were performed using SAS version 8.2 from the SAS Institute in North Carolina.
The sample size of 250 was chosen because even a modest-to-low response rate would give adequate precision for region-specific estimates of proportions for each answer category (CIs no larger than ±8.8% and ±10.5% for response rates of 50% and 35%, respectively). The study was reviewed and approved by the University Health Network Research Ethics Board.
RESULTS
Respondents
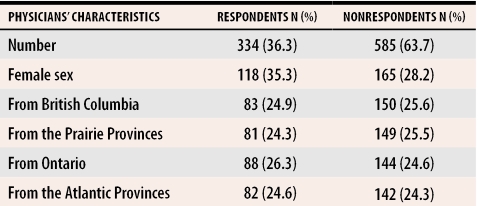
Of the 1000 physicians surveyed, 919 were eligible for the study. Physicians were excluded because they could not be located (31), were retired (17), or identified themselves as specialists (33). A total of 334 physicians (36.3% of the sample) responded to the survey. The only significant difference between respondents and nonrespondents was that respondents were more likely to be female (P = .03) (Table 2). Table 3 shows the practice characteristics of respondents.
Table 2. Profile of respondents and nonrespondents.
Mean year of graduation for respondents and nonrespondents was 1980.
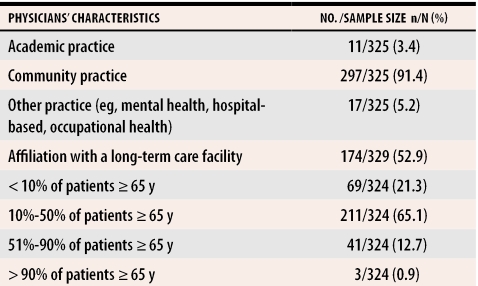
Table 3.
Practice characteristics of respondents
Responses
Prescribing frequency.
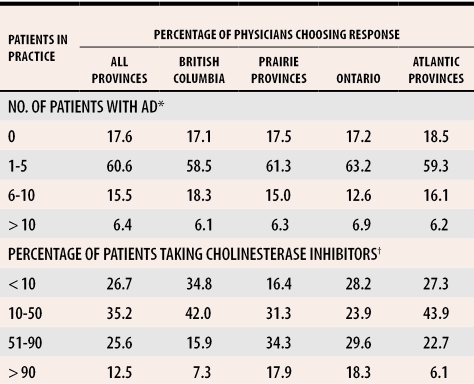
Physicians in all four regions reported about the same numbers of patients with AD in their practices (Table 4). Of the 256 physicians who responded on frequency of prescribing ChIs, more than 25% reported that < 10% of their AD patients were taking ChIs, and more than 10% indicated that > 90% of their AD patients were taking ChIs, with significant prescribing differences between regions with and without formulary coverage of ChIs (P < .035).
Table 4.
Percentage of physicians reporting numbers of patients with AD seen in their practices in a typical month and percentage of patients with AD taking cholinesterase inhibitors
AD—Alzheimer disease.
*There was no significant difference across all regions in the number of patients with AD physicians reported in their practices (P = .999).
†There was a significant difference across all regions in percentage of patients with AD taking cholinesterase inhibitors (P = .009). All comparisons between regions with and without formulary coverage for cholinesterase inhibitors were significantly different (P < .035); comparisons between regions with similar formulary coverage were not significant (P > .35).
Self-reported knowledge of ChIs.
Most of the physicians (82.2%) considered themselves somewhat knowledgeable about ChIs. A few (7.5%) considered themselves very knowledgeable, and a few (10.2%) considered themselves not knowledgeable.
Continuing education.
When physicians were asked whether they had had continuing medical education (CME) on ChIs during the last year, 54.9% reported attending a CME event, 82.2% reported reading journal articles, and 71.3% reported having spoken with pharmaceutical representatives about these drugs.
Perceived effectiveness.
In response to a question about the perceived effectiveness of ChIs, 1.3% of respondents considered them ineffective, 25.4% minimally effective, 65.0% somewhat effective, and 8.4% very effective. No respondent thought them extremely effective.
Approach to prescribing.
Regarding prescribing, 56.8% routinely recommended use of ChIs, 0.9% routinely recommended against use of ChIs, 31.5% generally deferred AD treatment recommendations to specialists, and 10.7% gave other responses (eg, left it up to patients or families to weigh risks and benefits).
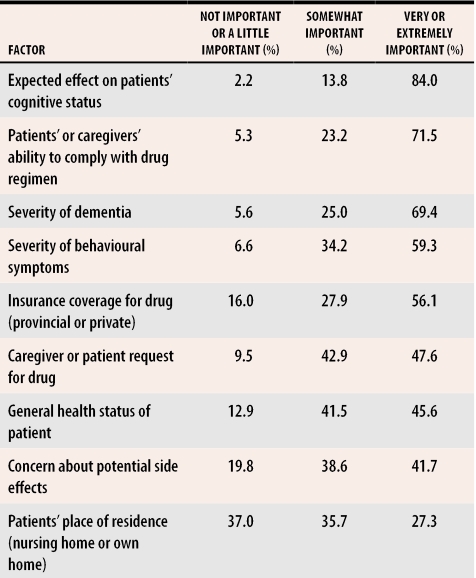
Factors affecting prescribing decisions.
The most important of nine factors respondents reported as being very or extremely important in their decisions to prescribe ChIs were the expected effect on cognitive status, patients’ or caregivers’ ability to comply with medical regimens, the severity of the dementia, the severity of behavioural symptoms, and the availability of insurance coverage for the drug (Table 5).
Table 5.
Factors affecting prescribing of cholinesterase inhibitors
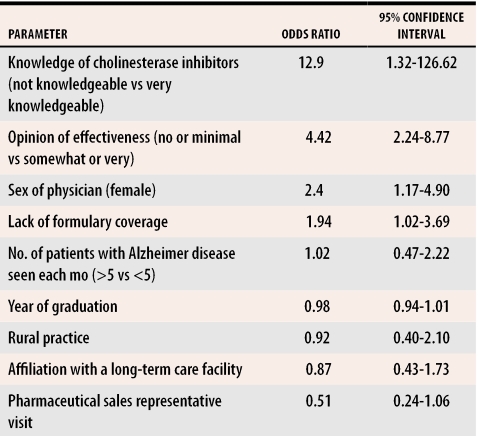
Logistic regression model
Respondents from provinces without formulary coverage of ChIs were nearly twice as likely to report that < 10% of their AD patients were taking ChIs (Table 6). Several physician factors predicted that respondents would report that < 10% of their AD patients were taking ChIs: female sex, lack of knowledge about ChIs, and perceptions that ChIs have no or little effectiveness. The regression model was well calibrated (Hosmer-Lemeshow statistic 5.78, P = .67) and had moderate-to-good discriminatory ability (C statistic 0.75).
Table 6. Predictors of low cholinesterase inhibitor use.
Logistic regression predicting the likelihood of physicians reporting that < 10% of their patients with Alzheimer disease were taking cholinesterase inhibitors.
DISCUSSION
This study provides new information about Canadian family physicians’ knowledge and views about ChIs, their ChI prescribing practices for AD patients, and the factors that might influence their prescribing practices. About a quarter of respondents (26.7%) reported that < 10% of their AD patients were taking ChIs, while slightly more than 10% of respondents (12.5%) indicated that > 90% of their AD patients were taking ChIs. Acetylcholinesterase inhibitors were prescribed more frequently in regions with formulary coverage, suggesting that formulary coverage influences prescribing of medications, as has been shown in other studies.16,17 Other factors that might influence regional variation in prescribing are differences in drug marketing and in the quality of continuing medical education. Additional factors that might contribute to variations in prescribing ChIs include concerns about contraindications to ChI use for certain patients and the fact that some patients and caregivers refuse this therapy.
Respondents’ knowledge of ChIs and their perceptions of the effectiveness of ChIs significantly influenced how many of their AD patients were taking ChIs. Also, some respondents (31.5%) indicated that they preferred that specialists make decisions about prescribing ChIs. This suggests that many family physicians are not confident about prescribing ChIs or about treating patients with AD. Attempts to promote optimal prescribing of ChIs should include educating physicians about the evidence regarding the effectiveness and safety of ChIs and other treatments for AD.
A recent Quebec survey of family physicians regarding the factors influencing their prescribing of ChIs to AD patients found that most physicians reported the following factors as important: adverse drug effects, severity of dementia, ease of drug administration, patient’s health, patient’s compliance, patient’s place of residence, and cost of the medication.12 These factors largely correspond with those identified in our study, except for patient’s place of residence, which was identified by only 28.2% of our respondents as being very or extremely important in their decisions to prescribe ChIs.
Female physicians were less likely to prescribe ChIs. This is consistent with a study of drug prescribing for older people in New Brunswick that found that high prescribers were more often male.18 Other studies have shown that female physicians are more likely to provide preventive screening and counseling19 and to order imaging scans.20
The variability in ChI use by region and physician factors raises important questions about the optimal prescribing rate and the possibility of underprescribing or overprescribing by some physicians. These findings, along with the growing prevalence of AD in Canada, speak to the pressing need to establish updated treatment guidelines and to ensure that these guidelines and the evidence on which they are based are disseminated to family physicians across the country. Consideration should also be given to establishing a program of confidential prescriber feedback and education to try to optimize AD drug prescribing, as was shown to be effective for antibiotic prescribing.21
Limitations
The response rate was relatively low (36.3%), but is in keeping with response rates in other surveys of family physicians. For example, a recent survey of ChI use among Quebec physicians had a response rate of 35.4%.12 Some factors that might have contributed to our low response rate were our request that survey responses be sent by facsimile to a Toronto number that was long distance for all but Toronto respondents; our lack of compensation to those surveyed (even token compensation has been shown to significantly improve response rates13,22); and the fact that the survey was carried out during the summer months, a period when many physicians are on holiday.
Our results might have been biased if physicians who responded to the survey were more interested or more knowledgeable about prescribing for AD patients than those who did not. If this were the case, our results would not be generalizable to a wider population of family physicians, and ChIs might actually be prescribed much less frequently than our study suggests. Also, the results might overrepresent the views of female physicians, as they were more likely to respond to the survey. Finally, we were able to assess prescribing frequency based only on physicians’ self-report, which could inaccurately represent actual prescribing rates.
Conclusion
Our survey found that prescribing patterns for ChIs in Canada varied. More than 25% of respondents indicated that <10% of their office patients with AD were taking ChIs, and more than 10% reported that >90% were taking ChIs. Our results suggest that being a female physician, lacking knowledge of ChIs, perceiving ChIs to be ineffective, and lack of formulary coverage of ChIs can reduce prescribing rates. With the increasing prevalence of AD in Canada, establishing up-to-date evidence-based guidelines for optimal prescribing of ChIs for AD patients and finding ways to encourage physicians to follow these guidelines are needed.
Acknowledgments
Dr Melinda Hillmer was supported by the University of Toronto Nu Sigma Nu Fraternity Summer Scholarship. Dr Krahn is partially supported by a Canadian Institutes of Health Research Investigator Award and by the F. Norman Hughes Chair in Pharmacoeconomics in the Faculty of Pharmacy at the University of Toronto. Dr Naglie is partially supported by the Mary Trimmer Chair in Geriatric Medicine Research at the University of Toronto. Mr Hillmer is partially supported by a Canadian Institutes of Health Research Doctoral Award.
Biographies
Dr Hillmer is a first-year internal medicine resident in the Faculty of Medicine at the University of Toronto in Ontario.
Dr Krahn is an internist at the University Health Network and an Associate Professor in the Departments of Medicine, Pharmacy, and Health Policy, Management and Evaluation at the University of Toronto. He holds the F. Norman Hughes Chair in Pharmacoeconomics in the Faculty of Pharmacy at the University of Toronto and an Investigator Award from the Canadian Institutes of Health Research.
Mr Hillmer is a doctoral candidate in clinical epidemiology in the Department of Health Policy, Management and Evaluation at the University of Toronto.
Dr Pariser, a family physician on staff at Sunnybrook and Women’s College Health Sciences Centre, is in private practice in Toronto and is an Assistant Professor in the Department of Family and Community Medicine at the University of Toronto.
Dr Naglie is a staff geriatrician at the University Health Network and the Toronto Rehabilitation Institute. He holds the Mary Trimmer Chair in Geriatric Medicine Research at the University of Toronto, is a senior scientist at the Toronto General Research Institute and at the Toronto Rehabilitation Institute, and is an Associate Professor in the Departments of Medicine and Health Policy, Management and Evaluation at the University of Toronto.
Footnotes
Competing interests: None declared
References
- 1.Canadian Study of Health and Aging: study methods and prevalence of dementia. CMAJ 1994;150:899-913. [PMC free article] [PubMed]
- 2.National Institute for Health and Clinical Excellence. Donepezil, rivastigmine and galantamine for the treatment of Alzheimer’s disease. Report 19. London, UK: National Institute for Clinical Excellence; 2001. [cited 2005 November 23]. Available at: http://www.nice.org.uk. [Google Scholar]
- 3.Lanctot KL, Herrmann N, Yau KK, Khan LR, Liu BA, LouLou MM, Einarson TR. Efficacy and safety of cholinesterase inhibitors in Alzheimer’s disease: a meta-analysis. CMAJ. 2003;169:557–564. [PMC free article] [PubMed] [Google Scholar]
- 4.Birks J, Grimley EJ, Iakovidou V, Tsolaki M. Rivastigmine for Alzheimer’s disease. Cochrane Database Syst Rev. 2000. CD001191. [DOI] [PubMed]
- 5.Olin JT, Schneider L. Galantamine for Alzheimer’s disease. Cochrane Database Syst Rev. 2002. CD001747. [DOI] [PubMed]
- 6.Wolfson C, Oremus M, Shukla V, Momoli F, Demers L, Perrault A, et al. Donepezil and rivastigmine in the treatment of Alzheimer’s disease: a best-evidence synthesis of the published data on their efficacy and cost-effectiveness. Clin Ther. 2002;24:862–886. doi: 10.1016/s0149-2918(02)80004-2. [DOI] [PubMed] [Google Scholar]
- 7.Birks JS, Harvey RJ. Donepezil for dementia due to Alzheimer’s disease. Cochrane Database Syst Rev. 2003. CD001190. [DOI] [PubMed]
- 8.Trinh N-H, Hoblyn J, Mohanty S, Yaffe K. Efficacy of cholinesterase inhibitors in the treatment of neuropsychiatric symptoms and functional impairment in Alzheimer disease: a meta-analysis. JAMA. 2003;289:210–216. doi: 10.1001/jama.289.2.210. [DOI] [PubMed] [Google Scholar]
- 9.AD2000 Collaborative Group. Long-term donepezil treatment in 565 patients with Alzheimer’s disease (AD2000): randomised double-blind trial. Lancet. 2004;363:2105–2115. doi: 10.1016/S0140-6736(04)16499-4. [DOI] [PubMed] [Google Scholar]
- 10.Patterson CJ, Gauthier S, Bergman H, Cohen CA, Feightner JW, Feldman H, et al. Canadian Consensus Conference on Dementia: a physician’s guide to using the recommendations. CMAJ. 1999;160:1738–1742. [PMC free article] [PubMed] [Google Scholar]
- 11.Doody RS, Stevens JC, Beck C, Dubinsky RM, Kaye JA, Gwyther L, et al. Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1154–1166. doi: 10.1212/wnl.56.9.1154. [DOI] [PubMed] [Google Scholar]
- 12.Oremus M, Wolfson C. Factors influencing the prescribing of cholinesterase inhibitors to Alzheimer’s disease patients [abstract]. Vol. 6. Geriatr Today: J Can Geriatr Soc 2003; p. 65. [Google Scholar]
- 13.Edwards P, Roberts I, Clarke M, Di Guiseppi C, Pratap S, Wentz R, et al. Increasing response rates to postal questionnaires: systematic review. BMJ. 2002;324:1183–1185. doi: 10.1136/bmj.324.7347.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosmer DW, Taber S, Lemeshow S. The importance of assessing the fit of logistic regression models: a case study. Am J Public Health. pp. 1630–1635. [DOI] [PMC free article] [PubMed]
- 15.Ash AS, Shwartz M. Evaluating the performance of risk-adjustment methods: dichotomous measures. In: Iezzono LI, editor. Risk adjustment for measuring health care outcomes. Ann Arbor, Mich: Health Administration Press; 1994. p. 423. [Google Scholar]
- 16.Carroll NV. How effectively do managed care organizations influence prescribing and dispensing decisions? Am J Manag Care. 2002;8:1041–1054. [PubMed] [Google Scholar]
- 17.Godwin M, Chapman J, Mowat D, Racz W, McBride J, Tang J. Delisting of drugs in Ontario. How attitudes and prescribing strategies of family physicians in the Kingston area changed. Can Fam Physician. 1996;42:1309–1316. [PMC free article] [PubMed] [Google Scholar]
- 18.Davidson W, Molloy DW, Somers G, Bedard M. Relation between physician characteristics and prescribing for elderly people in New Brunswick. CMAJ. 1994;150:917–921. [PMC free article] [PubMed] [Google Scholar]
- 19.Henderson JT, Weisman CS. Physician gender effects on preventive screening and counseling: an analysis of male and female patients’ health care experiences. Med Care. 2001;39:1281–1292. doi: 10.1097/00005650-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Rosen MP, Davis RB, Lesky LG. Utilization of outpatient diagnostic imaging. Does the physician’s gender play a role? J Gen Intern Med. 1997;12:407–411. doi: 10.1046/j.1525-1497.1997.00071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hux JE, Melady MP, DeBoer D. Confidential prescriber feedback and education to improve antibiotic use in primary care: a controlled trial. CMAJ. 1999;161:388–392. [PMC free article] [PubMed] [Google Scholar]
- 22.Dillman DA. Survey implementation. In: Mail and Internet surveys: the tailored design method. 2nd ed. New York, NY: John Wiley & Sons, Inc; 1999. pp. 167–170. [Google Scholar]