Abstract
OBJECTIVE
To describe medical marijuana use from the perspectives of patients with multiple sclerosis.
DESIGN
A qualitative, descriptive design was used. Participants discussed their medicinal marijuana use in one-to-one, semistructured interviews.
SETTING
Interviews were conducted at a time and place convenient to participants.
PARTICIPANTS
Six men and eight women with multiple sclerosis participated.
METHOD
Potential participants identified themselves to the researcher after receiving an invitation in a mailed survey. Eligibility was confirmed, and purposive sampling was used to recruit subjects. A range of issues emerged from the interviews. Interviews and data analysis continued until saturation occurred.
MAIN FINDINGS
Descriptions fell into three broad areas: patterns of use, legal or social concerns, and perceived effects. Consumption patterns ranged from very infrequent to very regular and were influenced by symptoms, social factors, and supply. Legal concerns expressed by most respondents were negligible. Social concerns centred on to whom use was revealed. The perceived benefits of use were consistent with previous reports in the literature: reduction in pain, spasms, tremors, nausea, numbness, sleep problems, bladder and bowel problems, and fatigue and improved mood, ability to eat and drink, ability to write, and sexual functioning. Adverse effects included problems with cognition, balance, and fatigue and the feeling of being high. Although participants described risks associated with using marijuana, the benefits they derived made the risks acceptable.
CONCLUSION
Further research is needed to clarify the safety and efficacy of marijuana use by patients with multiple sclerosis. If evidence of benefit is seen, medicinal marijuana should be made available to patients who could benefit from it. Until then, discussing medicinal marijuana use with patients will be awkward for health professionals.
Abstract
OBJECTIF
Décrire ce que pensent les patients atteints de sclérose en plaques de l’usage médical de la marijuana.
TYPE D’ÉTUDE
On a utilisé une étude qualitative et descriptive. Les participants ont discuté de l’usage médical qu’ils faisaient de la marijuana lors d’entrevues semi-structurées individuelles.
CONTEXTE
Les entrevues avaient lieu au moment et à l’endroit qui convenaient aux participants.
PARTICIPANTS
Six hommes et huit femmes atteints de sclérose en plaques.
MÉTHODE
Les participants potentiels ont contacté le chercheur après avoir reçu une invitation lors d’une enquête postale. Après confirmation de leur éligibilité, les sujets ont été recrutés par échantillonnage raisonné. Les entrevues ont permis d’identifier plusieurs sujets différents. Les entrevues ainsi que l’analyse des données ont été poursuivies jusqu’à obtention d’une saturation.
PRINCIPALES OBSERVATIONS
Les sujets abordés étaient de trois ordres: modèle d’utilisation, préoccupations légales ou sociales et effets perçus. Les modèles d’utilisation variaient de «très rarement» à «très régulièrement» et ils étaient influencés par les symptômes, les facteurs sociaux et l’approvisionnement. La plupart des participants étaient très peu préoccupés par l’aspect légal. Les préoccupations sociales dépendaient surtout des personnes mises au courant. Les avantages rapportés concordaient avec les résultats déjà publiés: diminution des douleurs, spasmes, tremblements, nausées, engourdissements, insomnies, troubles vésicaux et intestinaux et fatigue, et amélioration de l’humeur, de la capacité de manger et de boire, de l’écriture et de l’activité sexuelle. Les effets indésirables incluaient la fatigue, les problèmes d’équilibre ou d’ordre cognitif et la sensation d’exaltation. Même s’ils connaissaient les risques découlant de l’usage de la marijuana, les participants considéraient que les avantages retirés rendaient ces risques acceptables.
CONCLUSION
D’autres études seront nécessaires pour clarifier l’efficacité et l’innocuité de l’usage de la marijuana chez les patients souffrant de sclérose en plaques. Si on démontrait que cette drogue est bénéfique, on devrait en faciliter l’accès aux patients susceptibles d’en bénéficier. D’ici là, il demeure inopportun pour le professionnel de la santé de discuter de l’usage médical de la marijuana avec son patient.
EDITOR’S KEY POINTS.
Marijuana is being used increasingly by patients both informally and, more recently, within a medical context to relieve a variety of symptoms. Family doctors could be asked to support patients’ decisions or even to complete a legal exemption for its use.
In these multiple sclerosis patients, consumption was highly variable: some had never used it before the diagnosis; others were regular recreational users before the illness presented. Patterns of consumption were equally variable: from a few times a year to regular use several times a day.
Some patients used marijuana to relieve specific symptoms while others used it for “maintenance.” Supply was usually not a problem, but cost occasionally was. Most patients did not feel threatened by its illegal status.
Despite side effects and social and legal constraints, most patients believed the benefits outweighed the risks. They shared information with their family doctors who were considered sympathetic. Some were aware of the medical exemption, but preferred to manage marijuana use themselves and were satisfied with the legal status quo.
POINTS DE REPÈRE DU RÉDACTEUR.
De plus en plus de patients consomment de la marijuana à des fins personnelles ou, plus récemment, dans un contexte médical, pour soulager divers symptômes. Le médecin de famille pourrait être appelé à conseiller le patient sur ce choix ou à rédiger une demande d’exemption légale pour son usage.
Chez ces patients atteints de sclérose en plaques, la consommation était très variable; certains n’en avaient jamais utilisée avant le diagnostic; d’autres en consommaient régulièrement à des fins récréatives avant l’apparition de la maladie. Les modèles de consommation étaient aussi variables: de quelques fois par année à plusieurs fois par jour.
Certains patients utilisaient la marijuana pour soulager des symptômes spécifiques tandis que d’autres s’en servaient comme «traitement d’entretien». L’approvisionnement ne posait généralement pas de problème, mais le coût était parfois un obstacle. La plupart des patients n’étaient pas préoccupés par la nature illégale de la drogue.
Malgré les effets indésirables et les contraintes sociales et légales, la plupart des patients considéraient que les avantages l’emportaient sur les risques. Ils en discutaient avec leur médecin de famille si celui-ci semblait sympathique. Certains connaissaient l’exemption médicale, mais préféraient gérer eux-mêmes l’utilisation de la drogue et se satisfaisaient du statut quo légal.
Patients with a variety of diseases and conditions are choosing to use cannabis to relieve symptoms.1 Consistent with the rationale frequently provided for using complementary and alternative medicines (CAM) generally,2 medicinal cannabis users often report cannabis to be effective where conventional medicine has failed.1
Multiple sclerosis (MS) is an example of a chronic illness for which conventional medicine often offers only partial relief.3-5 Prevalence studies indicate that 2% of the general Canadian population uses marijuana medicinally6 and 14% to 16% of people with MS use marijuana medicinally.7,8 As is the case with many complementary therapies, use of marijuana has preceded scientific endorsement of its safety and efficacy. Unlike other CAM, marijuana is an illegal substance; its possession, sale, or consumption can lead to criminal charges.
A few trials have evaluated use of cannabis extracts (delta-9-tetrahydrocannabinol, cannabidiol) or synthetic cannabinoids (eg, nabilone) in MS patients.9-13 While subjective improvements have been reported in many of these studies, there have been fewer reports of objective improvements. The largest randomized trial to date (n = 630) revealed no improvement in spasticity scores among patients given cannabinoids, although the results suggest these compounds are useful for increasing mobility and for pain control.14 Fewer studies have examined the effects of cannabis in its smoked form, commonly referred to as marijuana. Two case studies described improvements in clinical ratings of tremor, spasticity, and ataxia15 and suppression of pendular nystagmus after marijuana was consumed.16 Results of a small trial (n = 10) showed impaired postural control and balance after smoking marijuana; however, subjective improvement in performance was reported.17 Respondents to mailed surveys have reported improvement in several MS symptoms including spasticity, pain, tremor, emotional dysfunction, and sleeplessness after smoking marijuana.7,8,18
Several recent descriptive studies have focused on medicinal cannabis use by Canadians with a range of conditions. In these studies, marijuana was reported to relieve numerous physical and psychological symptoms. Most people smoked marijuana, and patterns of consumption varied.1,8,19-21 Ware and colleagues suggest that many practitioners across Canada have encountered patients who are either already using cannabis, or who, in light of media interest, come to their physicians requesting advice or information.21
There are no published reports about the social, legal, and financial aspects of medicinal marijuana use by people with MS. The purpose of this study is to describe this broader context and the experience of medicinal marijuana use by people with MS, and the perceived effects of use. This description will give physicians a greater understanding of the issues surrounding medicinal marijuana use by people with MS. This knowledge in turn could assist physicians in discussing medicinal marijuana use with patients. Although focused on a specific patient group, these findings could add to understanding about other patient groups who use marijuana medicinally.
METHOD
Sample
A survey examining the use of CAM generally, and marijuana specifically, was mailed to a sample of 780 patients from the MS clinic database at Foothills Provincial Hospital in Calgary, Alta. Details of this survey are reported elsewhere.8,22 Potential interviewees identified themselves by responding to an invitation letter in the survey. Eligibility criteria were using medicinal marijuana, being at least 18 years old, and having a diagnosis of clinically definite MS or laboratory-supported MS. Purposive sampling was used to achieve similar numbers of men and women and to include people with a range of disability. The final sample size was determined by achievement of saturation (ie, new participants were interviewed until no new information was found).
Data collection
A qualitative descriptive design23 was used. Data were collected using semistructured interviews conducted by the first author. An interview guide, developed specifically for this study, drew from the medical literature, articles in the media, and written comments made in the survey. The interview guide reflected these variables but was flexible, allowing respondents to speak freely and allowing the interviewer to ask further questions relevant to individual participants. All descriptions were elicited in a non-directive manner.
The interviews were tape-recorded and transcribed with participants’ permission. Participants could review the transcript and withdraw information if they wished. Participants completed a questionnaire containing eight sociodemographic and illness-related questions.
Data analysis
Taped interview data were transcribed verbatim, verified for accuracy by the interviewer and the informants (when they desired), and entered into Ethnograph 5.0.24
Qualitative content analysis was completed by the first author using methods recommended by Miles and Huberman25 in 1994. Those authors advocated use of three concurrent activities in qualitative analysis: data reduction, data display, and conclusion drawing or verification.25
The analyst evaluated consistency by recoding a sample of randomly selected data and comparing it with the initial coding. Credibility of the analysis was assessed by establishing equivalence in coding decisions and interpretations on a sample of data between the primary analyst and a second researcher skilled in qualitative methods. A summary of the main interview themes was sent to four participants for review to validate the researcher’s interpretation of the data.26
Ethics approval was received from the Conjoint Health Research Ethics Board at the University of Calgary.
FINDINGS
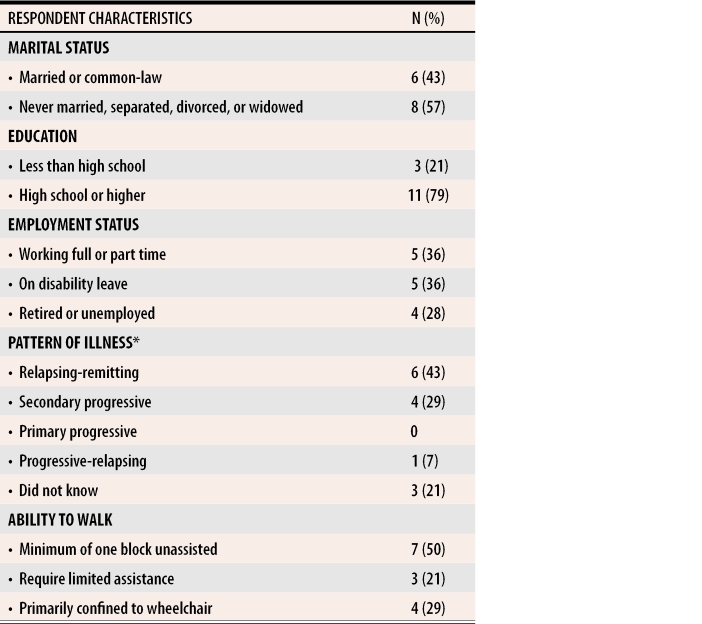
Interviews were conducted with 14 people. Median interview time was 45 minutes (range 25 to 90 minutes). Sociodemographic and illness characteristics are shown in Table 1.
Table 1. Sociodemographic and illness-related characteristics of participants.
Six respondents were male; eight were female; median age was 43 years (range 38 to 49).
*Median time since diagnosis 11.5 years (range 5 to 16 years).
Ten participants reviewed their transcripts: four declined. No problems with content were identified. Results of the multiple coding strategies demonstrated high correspondence.
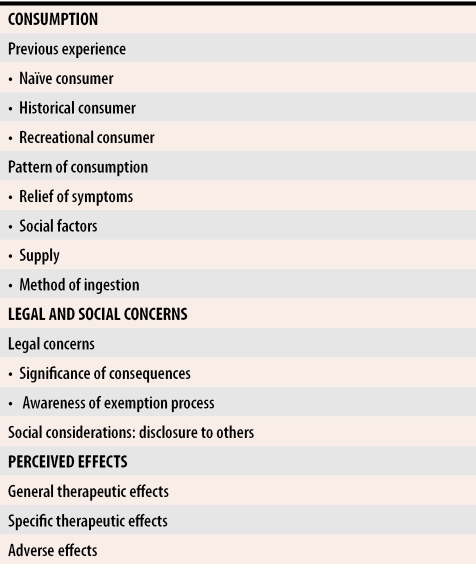
Participants’ descriptions of their experiences with marijuana consumption are summarized in Table 2 and described in detail below. Descriptions fell into three broad areas: consumption, social and legal concerns, and perceived effects.
Table 2.
Participants’ descriptions of marijuana use
Consumption
Previous experience with marijuana varied among participants. Some described themselves as naïve to marijuana before their current medical use. Others spoke of having used marijuana in high school or university, but not having used it for some time. A third group were long-standing recreational users who, because of illness, had come to use marijuana medicinally. Patterns of consumption varied considerably from very infrequent (eg, once or twice yearly) to several times daily. Consumption patterns were influenced by symptoms, social factors, and supply.
Symptoms.
Marijuana was used to obtain relief both from both specific symptoms (eg, pain, spasms) and general symptoms (eg, “feeling crummy”). Frequency of use for some was directly influenced by the frequency of these symptoms. Others experienced more persistent symptoms and eventually used marijuana as a last resort. Others used marijuana for “maintenance;” marijuana was used throughout the day as a way of controlling symptoms and facilitating more normal functioning.
Social factors.
Employment status affected the pattern of marijuana consumption. Not surprisingly, people who held jobs confined their consumption to leisure times, primarily evenings and weekends. They acknowledged difficulty in “trying to work under the effects.” These people managed their symptoms during the day but frequently reported using marijuana after work or before retiring at night.
Social affiliations also influenced consumption patterns. Some participants described knowing people who were recreational users, and they used marijuana when these other people were using it. A few respondents indicated they used marijuana only when they were at home alone. These respondents were married and had partners who, while supportive of their decision to use marijuana, did not use it themselves.
Supply.
A few respondents were dependent on others to supply them. Reasons for this were that a friend or spouse was a recreational user who maintained a supply, or that the friend or spouse viewed it as part of his or her caregiving role. Some initially expressed uncertainty when asked whether they would know how to find a supply of marijuana for themselves; however, they later indicated they might know someone who could help them find it.
Others purchased their own supply. Most stated they knew their suppliers personally and trusted the privacy of the transaction and the quality of the product. Several people said that if they were unable to obtain marijuana from their usual sources, they would likely do without rather than “hanging out in the bar” or “walking the streets” to find new sources. Most participants gave the impression that getting the drug was relatively easy. One participant stated, “There’s tons of it around; it’s not hard to find. … There is always somebody who knows somebody.” In contrast, one participant said finding marijuana was becoming increasingly difficult. This participant was more isolated than most, as she lived alone and was not independently mobile.
The cost of marijuana varied from negligible in the case of those whose supply was provided by friends to estimates of between $50.00 and $500.00 monthly. For some, cost precluded use. For others, the cost meant that other areas of spending had to be cut back.
Method of ingestion.
All participants smoked marijuana through cigarettes or pipes. A few people were tobacco smokers, so smoking marijuana did not pose problems for them. Those who were non-smokers were not worried about the health effects of smoking for several reasons (eg, believing that using a water pipe would remove toxins, the fact that only “a few puffs” were ever consumed, and believing that having MS was a greater threat to their health than smoking marijuana could ever be). Smoking concerned a couple of participants because their lack of coordination made burns a risk.
Social and legal concerns
Legal concerns.
Most indicated that concerns about the legal consequences of marijuana use were negligible for two reasons. First, people described their use of marijuana as very discreet. The substance was obtained through trusted sources and consumption was confined primarily to the privacy of their homes. The risk of being caught was perceived as extremely low. Second, the consequences of being caught were not perceived as severe enough to deter people. A few respondents believed that the small amounts they had would be regarded as for “personal use” (versus trafficking) and that the consequences for possession of such amounts would be minimal. Moreover, recognizing the current debate over its legal, medicinal status, others believed their reason for use would minimize consequences if they were caught.
Awareness of the exemption process varied among participants. Those who were aware had limited knowledge of the process and had not applied for the exemption. They believed that it would be more trouble than it was worth given the “bureaucracy,” “red tape,” and expectation that they would have to “jump through hoops.” Participants believed the exemption would provide no tangible benefits because, at the time of the interviews, marijuana would still have to be purchased out of pocket from illegal sources. One participant thought that being granted an exemption would open patients up to unwanted scrutiny, stating that “[A]s soon as you get on that [list], then everything becomes suspect.” Some saw legalization as a way for the government to make money; a few suggested that the potency of a legal supply would be insufficient. Although participants were generally in favour of legalizing marijuana for medicinal use, they appeared content to maintain the status quo with respect to their current, individual use.
Social considerations.
Some participants described themselves as very private. They had not disclosed to others outside their immediate families that they had MS, much less that they were using marijuana. Information was shared on a “need to know” basis. Other participants indicated they were quite open about their use, stating that while they did not flaunt it, they did not hide it either. A few participants had children living with them. Use was generally kept hidden from younger children, but was disclosed to older children.
A few participants reported they told people about their use of marijuana based on their perceptions of how these others would react. The decision to disclose or not was often made following efforts to gauge others’ reactions to their use. While most people described family and friends as supportive of their marijuana use, a few experienced disapproval. Disapproval was based on the legal status of marijuana, on its potentially negative effects, and on its being addictive. A couple of the recreational users said that family members had some difficulty in viewing their current use as medicinal, given their previous recreational use.
Anticipation of potential reactions was also important in decisions about discussing use with health care professionals: “It took me a while just because I wasn’t sure of what their reaction would be. So you just sort of slide little things in here and there.” In addition to surreptitiously testing the waters, participants described using other factors, such as age and attitudes toward CAM generally, to anticipate the reaction of health professionals. If negative reactions were anticipated, use was not divulged. When use had been disclosed, physicians’ and other health care professionals’ reactions were minimal, described as ranging from neutral to mildly interested. Nobody indicated that use of marijuana was discouraged. Some participants acknowledged that physicians were not in a position to encourage use. A couple of people indicated they had been questioned about their use of other therapies when they entered drug trials and that they had disclosed their use at that time. These participants readily discontinued marijuana use for the duration of the trials.
Perceived effects
The effects of marijuana were described as both an overall sense of relaxation and relief of specific symptoms. Relaxation was described physically as affecting the whole body, providing sensations of “tingling” and “floating.” Relaxation was spoken of in psychological terms, as providing relief by “removing stresses” and by creating a feeling of “mellowness” or “sense of peace.” These feelings were reported as “almost instant” by many participants, and their duration varied from a couple of hours to well into the next day.
Specific therapeutic effects included reduction in pain, spasms, tremors, nausea, numbness, bladder and bowel problems, and fatigue and improved mood, ability to eat and drink, ability to write, and sexual functioning. Many people reported greater ease in falling asleep and more restful sleep. Several people commented on a reduced need for conventional medications (eg, painkillers, muscle relaxants) with marijuana use.
A few participants described negative, or unwanted, side effects, such as problems with cognition (decreased lucidity, decreased concentration, forgetfulness), and problems with balance and fatigue. Behaviour associated with the “high” were thought undesirable by some (eg, giggling, “grinning like an idiot,” extreme fatigue).
The therapeutic effects of marijuana could not be separated entirely from the experience of a “high.” While several people acknowledged this, they emphasized that the motivation for use was not to get high, but rather to obtain relief of their symptoms. Others spoke of trying to optimize therapeutic effects while minimizing negative effects by controlling the dose they used or by using immediately before going to bed at night.
DISCUSSION
To our knowledge, this was the first study to describe the effects of marijuana and the broader context of medicinal marijuana use among people with MS. Given the small sample and single diagnosis, it is possible the experiences of participants in this study are dissimilar to those of other medicinal marijuana users.
Experience with marijuana use and consumption patterns varied among participants. The frequency and pattern of marijuana use was influenced in part by symptoms; this finding is consistent with descriptions given by patients with other illnesses or conditions.1 Employment and social connections were also identified as influencing patterns of consumption in this study; employment limited opportunities for consumption; social connections increased them. Participants conceded that the latter point brought a recreational aspect to use; others have reported a blurring of the line between recreational and medicinal uses.1,19
Several studies have reported on the perceived therapeutic effects of marijuana for symptom relief in MS. Descriptions of the therapeutic benefits and side effects experienced with marijuana were compatible with those reported in earlier studies.15-18 Smoking was the preferred method of ingestion and did not provoke concern regarding respiratory health. A unique consideration identified in this study was the possibility of sustaining burns due to impaired physical ability to grasp a cigarette or pipe securely.
Participants in this study gave the impression they were not overly concerned with the illicit nature of their consumption and had not had any interactions with the justice system. This was different from the findings of others.1 Like participants in the study by Ogborne et al, however, many believed the reason for use would serve to mitigate consequences were they ever confronted.
Disclosure to physicians was not universal, as others have reported.1,19 Further exploration of this finding in our study suggested decisions to share this information depended on perceptions of how physicians would react. If negative reactions were anticipated, people did not reveal their consumption.
Implications for health professionals
This study describes how illicit medicinal marijuana use affects the lives of people with MS with regard to perceived effects, social implications, and legal concerns. Although participants in this study might have been eligible for an exemption to use marijuana medicinally, none had applied, making their consumption illegal under current regulations.27 Whatever regulations are in place, some people likely will choose to use marijuana without going through legal channels.
Results suggest that health care professionals did not routinely ask participants about marijuana use. Those who voluntarily disclosed use did so based on how they perceived these professionals would react. Questioning patients about their use of all conventional medication, illicit drugs, and CAM should be routine in taking patient histories. It is possible that this group of patients did not recall being asked these questions or that they began using marijuana after their early or initial clinical visits.
Physicians are put in a difficult position with respect to patient’s illicit use of marijuana, whether patients provide information voluntarily or in response to direct questions. On one hand, patients have autonomously chosen to use marijuana and might perceive benefits from its use. Discouraging patients could damage the therapeutic relationship and prevent patients from further discussing marijuana use, or other illegal practices affecting their health. On the other hand, the lack of scientific evidence for marijuana’s safety and effectiveness coupled with its ambiguous legal standing makes it difficult to condone this behaviour in good conscience.
Practitioners must exercise professional judgment when discussing illicit medicinal marijuana use with patients. Asking patients about use allows them to be monitored for both therapeutic and adverse effects. Health professionals might choose to go one step further and provide information about safe administration, potential side effects, and contraindications to use. Such information has been published in the scientific literature.28
In contrast, practitioners may choose not to discuss illicit marijuana use with patients beyond noting that it is consumed. They may feel unable to condone the activity and unprepared to give advice on the issue. In either situation, health professionals can inform patients of the exemption options available in their jurisdictions and can direct them toward reliable sources of information.
Physicians are bound by their ethical obligation to protect patient confidentiality and cannot disclose information learned in the context of professional relationships outside of the health care team unless they have patients’ informed consent, unless it is legally required, or unless failure to disclose would cause harm to that person or to other people.29 Practitioners experiencing dilemmas should obtain guidance from their professional licensing bodies or legal advisors.
Conclusion
Participants reported that marijuana was effective in helping them to manage symptoms of MS. Participants’ descriptions suggest the risks encountered in marijuana use in terms of legal concerns, social considerations, financial costs, and side effects were outweighed by the benefits experienced in terms of symptom relief. Discussing medicinal marijuana use with patients can be enhanced by awareness of these issues. The debate over the legal status of medicinal marijuana and the lack of sufficient evidence supporting or refuting its efficacy make health professionals’ role challenging.
Acknowledgments
Funding provided by the Multiple Sclerosis Society of Canada is gratefully acknowledged. We sincerely appreciate the contributions of people who participated in interviews and shared their experiences. We thank Dr Meredith McKague for her assistance with establishing the credibility of the data analysis.
Biographies
Dr Page is a Research Associate for the Office of Medical Bioethics in the Faculty of Medicine at the University of Calgary in Alberta.
Dr Verhoef is a Professor in the Department of Community Health Sciences in the Faculty of Medicine at the University of Calgary.
Footnotes
Competing interests: The Multiple Sclerosis Society of Canada offered funding of $11 988.08. Neither author received benefits from any other organization with an interest in the subject matter of this article.
References
- 1.Ogborne AC, Smart RG, Weber T, Birchmore-Timney C. Who is using cannabis as a medicine and why: an exploratory study. J Psychoactive Drugs. 2000;32(4):435–443. doi: 10.1080/02791072.2000.10400245. [DOI] [PubMed] [Google Scholar]
- 2.Vincent C, Furnham A. Why do patients turn to complementary medicine? An empirical study. Br J Clin Psychol. 1996;35:37–48. doi: 10.1111/j.2044-8260.1996.tb01160.x. [DOI] [PubMed] [Google Scholar]
- 3.Weiner HL. A 21 point unifying hypothesis on the etiology and treatment of multiple sclerosis. Can J Neurol Sci. 1998;25(2):93–101. doi: 10.1017/s0317167100033680. [DOI] [PubMed] [Google Scholar]
- 4.Evans CF, Shriver LP. Multiple sclerosis: emerging opportunities for therapeutic intervention. Curr Drug Target CNS Neurol Disord. 2002;1:17–30. doi: 10.2174/1568007023339526. [DOI] [PubMed] [Google Scholar]
- 5.Rudick RA. Disease-modifying drugs for relapsing-remitting multiple sclerosis and future directions for multiple sclerosis therapeutics. Arch Neurol. 1999;56:1079–1084. doi: 10.1001/archneur.56.9.1079. [DOI] [PubMed] [Google Scholar]
- 6.Ogborne AC, Smart RG, Adlaf EM. Self-reported medical use of marijuana: a survey of the general population. CMAJ. 2000;162:1685–1686. [PMC free article] [PubMed] [Google Scholar]
- 7.Clark AJ, Ware MA, Yazer E, Murray TJ, Lynch ME. Patterns of cannabis use among patients with multiple sclerosis. Neurology. 2004;61(11):2098–2100. doi: 10.1212/01.wnl.0000127707.07621.72. [DOI] [PubMed] [Google Scholar]
- 8.Page SA, Verhoef MJ, Stebbins RA, Metz L, Levy JC. Cannabis use as described by people with multiple sclerosis. Can J Neurol Sci. 2003;30:201–205. doi: 10.1017/s0317167100002584. [DOI] [PubMed] [Google Scholar]
- 9.Brenneisen R, Elsohly MA, Henn V, Spiess Y. The effect of orally and rectally administered delta-9-tetrahydrocannabinol on spasticity: a pilot with 2 patients. Int J Clin Pharmacol Ther. 1996;34(10):446–452. [PubMed] [Google Scholar]
- 10.Clifford DB. Tetrahydrocannabinol for tremor in multiple sclerosis. Ann Neurol. 1981;13(6):669–671. doi: 10.1002/ana.410130616. [DOI] [PubMed] [Google Scholar]
- 11.Hamann W, di Vadi PP. Analgesic effect of the cannabinoid analogue nabilone is not mediated by opioid receptors. Lancet. 1999;353(9152):560. doi: 10.1016/s0140-6736(98)05429-4. [DOI] [PubMed] [Google Scholar]
- 12.Fox P, Bain PG, Glickman S, Carroll C, Zajicek J. The effect of cannabis on tremor in patients with multiple sclerosis. Neurology. 2004;62:1105–1109. doi: 10.1212/01.wnl.0000118203.67138.3e. [DOI] [PubMed] [Google Scholar]
- 13.Killestein J, Hoogervorst ELJ, Reif M, Kalkers NF, van Loenen AC, Staats PGM, et al. Safety, tolerability and efficacy of orally administered cannabinoids in MS. Neurology. 2002;58:1404–1407. doi: 10.1212/wnl.58.9.1404. [DOI] [PubMed] [Google Scholar]
- 14.Zajicek J, Fox P, Sanders H, Wright D, Vickery J, Nunn A, et al. Cannabinoids for treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): multicentre randomised placebo-controlled trial. Lancet. 2003;362:1517–1526. doi: 10.1016/S0140-6736(03)14738-1. [DOI] [PubMed] [Google Scholar]
- 15.Meinck HM, Schonle PW, Conrad B. Effect of cannabinoids on spasticity and ataxia in multiple sclerosis. J Neurol. 1989;236(2):120–122. doi: 10.1007/BF00314410. [DOI] [PubMed] [Google Scholar]
- 16.Schon F, Hart PE, Hodgson TL, Pambakian ALM, Ruprah M, Williamson EM, et al. Suppression of pendular nystagmus by smoking cannabis in a patient with multiple sclerosis. Neurology. 1999;53:2209–2210. doi: 10.1212/wnl.53.9.2209-a. [DOI] [PubMed] [Google Scholar]
- 17.Greenberg HS, Werness SAS, Pugh JE, Andrus RO, Anderson DJ, Domino EF. Short-term effects of smoking marijuana on balance in patients with multiple sclerosis and normal volunteers. Clin Pharmacol Ther. 1994;55(3):324–328. doi: 10.1038/clpt.1994.33. [DOI] [PubMed] [Google Scholar]
- 18.Consroe P, Musty R, Rein J, Tillery W, Pertwee R. The perceived effects of smoked cannabis on patients with multiple sclerosis. Eur Neurol. 1997;38(1):44–48. doi: 10.1159/000112901. [DOI] [PubMed] [Google Scholar]
- 19.Furler MD, Einarson TR, Millson M, Walmsley S, Bendayan R. Medicinal and recreational marijuana use by patients infected with HIV. AIDS Patient Care STDs. 2004;18(4):215–228. doi: 10.1089/108729104323038892. [DOI] [PubMed] [Google Scholar]
- 20.Ware MA, Doyle CR, Woods R, Lynch ME, Clark AJ. Cannabis use for chronic non-cancer pain: results of a prospective survey. Pain. 2003;102(1-2):211–216. doi: 10.1016/s0304-3959(02)00400-1. [DOI] [PubMed] [Google Scholar]
- 21.Ware MA, Gamsa A, Persson J, Fitzcharles MA. Cannabis for chronic pain: case series and implications for clinicians. Pain Res Manage. pp. 95–99. [DOI] [PubMed]
- 22.Page SA, Verhoef MJ, Stebbins RA, Metz L, Levy JC. Complementary and alternative medicine use by people with multiple sclerosis. Chronic Dis Can. 2003;24(2/3):75–79. [PubMed] [Google Scholar]
- 23.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 24.The Ethnograph, version 5.0. Thousand Oaks, Calif: Scolari, Sage Publications Software, Inc; 1998. [Google Scholar]
- 25.Miles MB, Huberman AM. Qualitative data analysis. 2nd ed. Thousand Oaks, Calif: Sage Publications Ltd; 1994. [Google Scholar]
- 26.Mays N, Pope C. Rigor and qualitative research. BMJ. 1995;311:109–112. doi: 10.1136/bmj.311.6997.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Government of Canada. Medical marihuana access regulations SOR/2001-27 pursuant to the Controlled Drugs and Substances Act s.c.1996, c.19, ss55(1). Ottawa, Ont: Government of Canada; 2001. [Google Scholar]
- 28.Sibbald B. A primer for patient’s use of medical marijuana [news]. CMAJ. 2001;165:329. [PMC free article] [PubMed] [Google Scholar]
- 29.Canadian Medical Association. Canadian Medical Association code of ethics. Ottawa, Ont: Canadian Medical Association; 1996. [Google Scholar]