Abstract
OBJECTIVE
Closed and conditionally closed practices appear to be increasing in many parts of Canada as reflected in the fact that more and more patients report difficulties finding family physicians who accept new patients. But the extent of, nature of, and factors related to open, closed, and conditionally closed practices are still largely unknown.
DESIGN
This study used data from the 2001 National Family Physician Workforce Survey for secondary analysis. Chi-square tests and logistic regression were used to examine factors related to FPs’ decisions to keep their practices open or to close them.
SETTING
Private offices, clinics, community health centres, and academic family medicine practice units in Canada.
PARTICIPANTS
Of 10 325 FPs surveyed, 2360 respondents who practised in emergency departments, hospitals, nursing homes, homes for the aged, walk-in clinics, and more than one setting were excluded. Overall response rate was 51.2%.
MAIN OUTCOME MEASURES
Practice status (open, conditionally closed, and closed), restrictions placed on conditionally closed practices, and factors associated with open practices.
RESULTS
The odds of having an open practice increased if respondents were male, younger than 35, working fewer hours at the time, or working in a group practice that included other types of physicians. Family physicians in rural and remote areas were much less likely than those in urban centres to close their practices. Conversely, FPs were more likely to close their practices when they perceived their communities to have good emergency department services and when other FPs in the community also had closed their practices.
CONCLUSION
Demographic and practice characteristics of physicians have an effect on whether practices are open, conditionally closed, or completely closed. But the broader practice environment, determined by such factors as geographic location and medical services available in the community, is equally important.
Abstract
OBJECTIF
Le nombre de pratiques fermées ou restreintes semble augmenter dans plusieurs régions du Canada, tel qu’indiqué par le fait qu’un nombre croissant de patients ont de la difficulté à trouver un médecin de famille (MF) qui accepte de nouveaux clients. Toutefois, les facteurs associés aux pratiques ouvertes, fermées ou restreintes de même que la nature et l’ampleur du phénomène sont encore peu connus.
TYPE D’ÉTUDE
Cette étude résulte d’une analyse secondaire des données du Sondage national de 2001 auprès des MF. On s’est servi de tests Chi2 et de régression logistique pour examiner les facteurs associés au fait qu’un MF décide de garder sa pratique ouverte ou de la fermer.
CONTEXTE
Bureaux privés, cliniques, centres de santé communautaires et unités de médecine familiale universitaires au Canada
PARTICIPANTS
Sur 10 325 MF sondés, 2360 répondants exerçant dans des services d’urgence, hôpitaux, maisons de soins infirmiers, foyers pour personnes âgées, cliniques sans rendez-vous ou dans plus d’un milieu ont été exclus. Le taux global de réponse était de 51,2 %.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Type de pratique (ouverte, restreinte ou fermée), conditions d’accès aux pratiques restreintes et facteurs associés aux pratiques ouvertes.
RÉSULTATS
Les répondants de moins de 35 ans, de sexe mâle, travaillant moins longtemps ou exerçant dans un groupe incluant d’autres types de médecins étaient plus susceptibles d’avoir une pratique ouverte. Par rapport aux MF des centres urbains, ceux des régions rurales ou éloignées étaient moins susceptibles de fermer leur pratique. Par ailleurs, les MF avaient plus de chances de fermer leur pratique s’ils estimaient que leur communauté disposait de bons services d’urgence ou quand d’autres MF de leur communauté avaient fermé leur pratique.
CONCLUSION
Les caractéristiques démographiques des médecins et leur type de pratique influencent le fait que leur pratique soit ouverte, restreinte ou complètement fermée. Mais des facteurs environnementaux plus larges, comme la situation géographique et la disponibilité de services médicaux dans la communauté, sont tout aussi importants.
EDITOR’S KEY POINTS.
An increasing number of family physicians have closed their practices to new patients.
This study suggests that FPs attempt to be responsible about limiting the size of their practices and to keep their practices open when patients have few medical care alternatives.
The odds of having an open practice increase if physicians are male, younger than 35, currently working fewer hours, or working in a group practice that includes other types of physicians.
Family physicians in rural and remote areas are much less likely than those in urban centres to close their practices.
POINTS DE REPÈRE DU RÉDACTEUR.
Un nombre croissant de médecins de famille n’acceptent plus de nouveaux patients.
Cette étude suggère que les MF s’efforcent d’agir de façon responsable lorsqu’il pensent limiter la taille de leur clientèle, gardant souvent leur pratique ouverte lorsqu’ils y a peu d’autres services médicaux disponibles.
La probabilité d’avoir une pratique ouverte augmente si le médecin a moins de 35 ans, est de sexe mâle, fait moins d’heures de travail ou exerce dans un groupe qui inclut d’autres types de médecins.
Les MF des régions rurales ou éloignées ont beaucoup moins de chances que ceux des centres urbains de fermer leur pratique.
In Canada, family physicians (the term “family physicians” here includes general practitioners) are seen as the entry point into the health care system. They deliver primary care services and refer patients to secondary and tertiary care.
Recently, an increasing number of FPs have closed their practices to new patients. According to the College of Physicians and Surgeons of Ontario, the percentage of its FP members willing to accept new patients declined from 39% in 2000 to 32% in 2002.1 A reported 74% of FPs in Saskatchewan have closed their practices to new patients.2 Closed medical practices have joined overcrowded emergency departments and long waiting lists as subjects of mass media coverage and public attention.3 Thus, an examination at the national level of factors influencing open and closed practices is timely. Although the problem is not unique to Canada, data from other countries are not entirely comparable because the Canadian health care system is different from all others.
This paper seeks to address three related issues. First, it identifies, at the national level, the proportion of FP practices open to new patients, conditionally closed, and completely closed. Second, it examines the conditions FPs set regarding when and what types of new patients will be accepted into their practices. Finally, it attempts to identify factors associated with having an open practice.
METHODS
This study is a secondary analysis of data collected in the 2001 National Family Physician Workforce Survey, a mailed survey of all FPs in Canada.4 Ethics approval was received before the survey was fielded. Overall response rate was 51.2%.4 Respondents included in this secondary analysis (n = 10 325) were those who reported that their main practice setting was an office-based practice in a private office, clinic, community health centre, or academic family medicine teaching unit and those who provided information on whether their practices were open or closed. Those who worked in emergency departments, hospitals, hospital inpatient units, nursing homes, homes for the aged, or walk-in clinics, as well as those who indicated more than one main practice setting, were excluded from the analysis (n = 2360).
Variables
Variables used in this analysis are described along with the rationale for their inclusion.
Practice status.
A question in the survey asked: “To what extent are you accepting patients into your main practice?” Family physicians who indicated that their practices were open to all new patients were considered to have open practices. Those who said their practices were closed but indicated that they would accept any patient who did not have a family physician were included in the open practice category, if they did not specify any restriction. Family physicians who indicated that their practices were completely closed and did not indicate any condition for accepting new patients were considered to have closed practices. Those indicating conditionally closed practices were further asked to indicate their conditions for accepting new patients.
Practice organization.
We thought that physicians in solo practice were less likely to accept new patients than those in FP-only or FP-and-specialist group practices, as the latter were more likely to have backup from other physicians.
Practice location.
We speculated that FPs practising in smaller or more remote communities would be less likely to close their practices. A previous study had found that physicians in rural areas were less likely to close their practices.5 Respondents’ postal codes were used to determine whether a practice was in an urban or a rural setting, using a definition based on population size and distance from urban centres.6
Sex.
We believed that male FPs would be more likely to have open practices because many female physicians, particularly younger ones, restrict their practice time because they have childbearing and child-rearing responsibilities.
Age.
Respondents were grouped into three age categories: 35 and younger, 36 to 54, and 55 or older. We believed that younger physicians, who could still be building up their practice, were most likely to have open practices.
Hours worked.
The effect of the number of hours worked was unclear. Physicians who worked longer hours could be more likely to accept new patients. Fewer hours of professional activity (indicating perhaps a capacity for more patients) could be associated with open practices. Hours spent on various professional activities were summed to show the total number of hours worked per week: less than 40 hours, 40 to 60 hours, and more than 60 hours.
Satisfaction.
A closed or conditionally closed practice might be associated with a greater sense of satisfaction with professional life, because the practice might seem more manageable. Answers to this question were grouped into three categories: dissatisfied, neutral, and satisfied.
Availability of FPs.
We thought that practices were more likely to be open in areas where more FPs accepted new patients because this might indicate a need for medical care in the community. In the survey, physicians were asked to subjectively assess, on a 5-point scale, the likelihood that other FPs in the community were accepting new patients. The “excellent” and “very good” categories were combined for our analysis.
Availability of emergency department services.
We predicted that practices were more likely to be closed if emergency department services were more available, since going to an emergency department could be seen as an alternative to seeing an FP. In the survey, FPs were asked to rate the availability of emergency department services on a 5-point scale. “Excellent” and “very good” were collapsed into one category.
Availability of medical services.
Physicians were asked to rate the availability of medical services in their community on a 4-point scale from “no problems” to “severe problems.” “No problem” and “minor problem” were combined into a single category.
Analysis
All analyses were done using the Statistical Package for the Social Sciences for Windows, version 11.5. Descriptive statistics were used to show the proportions of physicians who described their practices as open, conditionally closed, or closed. Chi-square tests were used to examine the association between practice status and the independent variables. Finally, the independent variables were entered into a forward stepwise logistic regression equation to examine the extent to which these factors are associated with having an open practice, taking the other factors into account.
RESULTS
Of the 10 325 physicians included in the analysis, 25.7% had open practices. Most physicians (67.6%) had conditionally closed practices, and a few (6.8%) indicated that their practices were completely closed.
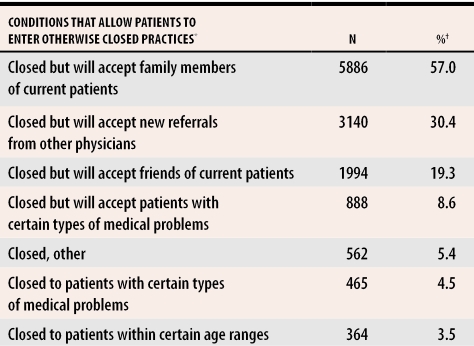
Conditions for conditionally closed practices
Of those who were conditionally accepting new patients, 40.7% imposed one condition, 33.8% had two conditions, 20.7% specified three conditions, and 4.8% indicated more than three conditions. The most common conditions are shown in Table 1. More than half of those with conditionally closed practices would make an exception for a family member of a current patient. About three of 10 FPs would accept a patient who had been referred to them by another physician. A few would accept, and some would exclude, patients who are children (0-12), teenagers (13-18), adults (19-59), or seniors (60+). Some said that they would not accept patients with certain health conditions, such as addictions, pregnancy, and mental health problems. Conversely, 8.6% said that they would accept new patients only if they had special health problems; the problems most often mentioned were AIDS, chronic or complex multisystem problems, and addictions.
Table 1.
Family physicians’ conditions for accepting new patients
*Includes all in office-based practice who also indicated their practice status.
†Physicians could specify more than one condition.
How well do various factors predict open practices?
Logistic regression was used to test the hypotheses and examine the predictive ability of the independent variables. Open practices were compared with conditionally closed and completely closed practices, which were collapsed into one category because so few physicians were in the “completely closed” category.
All predictor variables were entered in the forward stepwise regression model (available from the authors upon request). The model explained 31.1% of the variance observed. The overall ability of the model to predict the correct classification of a practice was 80.5%. It correctly predicted 93.5% of the closed and conditionally closed practices and 41.4% of the open practices. Factors important to the model are shown in Figures 1 and 2.
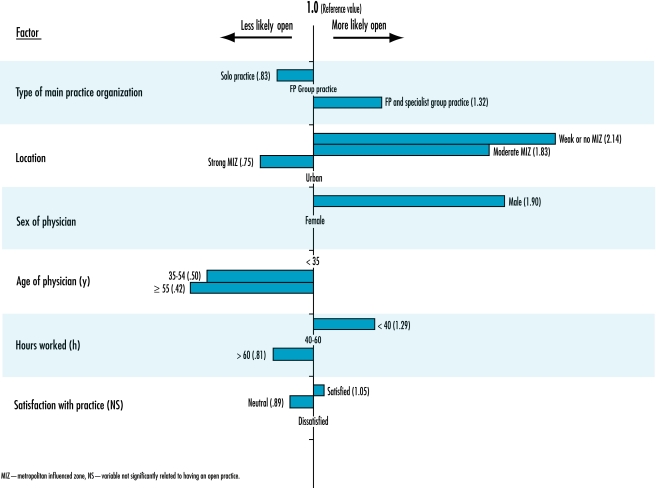
Figure 1.
Physician- and practice-related factors associated with FPs’ practices being open to new patients
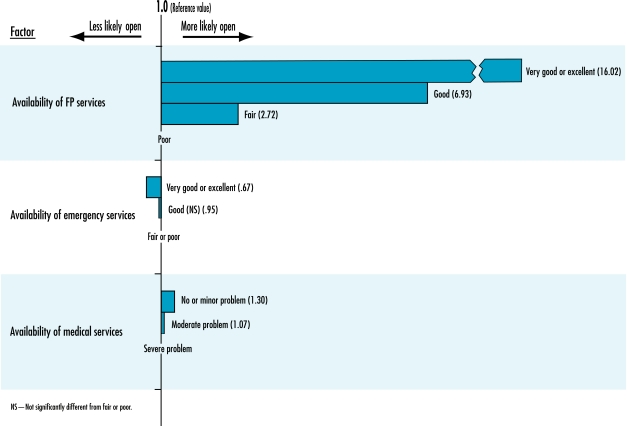
Figure 2.
Influence of physicians’ perceptions of service availability on the likelihood of having an open practice
Figure 1 presents how physicians and practice-related factors were associated with the likelihood of having an open practice. Solo FPs were least likely to have open practices. They were 0.83 times as likely to have open practices as FPs in FP-only group practices and only about half as likely to have open practices as FPs in FP-and-specialist group practices. Those in FP-and-specialist group practices were 1.32 times more likely to have open practices than those in FP-only group practices.
Geographic location of a practice was an important predictor. While only 25.7% of all practices were open practices, 53.2% of the practices in weak MIZ or no MIZ communities were open, and only 5.2% were completely closed. Practices in moderate and weak MIZ areas (ie, increasingly rural areas) were more likely to be open than urban practices. Practices located in strong MIZ communities (ie, city suburbs) were less likely to be open than those in urban areas (Figure 1).
Demographic and practice characteristics of physicians were also important. In simple bivariate analysis, 29.1% of male FPs had open practices compared with 20.3% of female FPs. In multivariate analysis, male physicians were almost twice as likely as their female counterparts to accept new patients. With respect to age, those aged 35 to 54 were half as likely as FPs younger than 35 to have open practices. Physicians 55 or older were much less likely to have open practices.
Physicians who typically worked less than 40 hours weekly were 1.29 times more likely than those working between 40 and 60 hours weekly to have open practices. Working more than 60 hours weekly was associated with a reduced likelihood of having an open practice. Although physician satisfaction was associated with having an open practice in bivariate analysis, when it was entered into the regression equation, the association became weaker and was not statistically significant.
Physicians’ perceptions of service availability were related to the likelihood of having open practices (Figure 2).
Practices in areas with very good or excellent possibilities of other FPs accepting new patients were more than 16 times as likely to be open as practices located in areas where FP availability was seen as poor. In areas where FP availability was perceived as good, practices were 6.93 times more likely to be open than in areas of poor availability.
Compared with areas where emergency department services were seen as fair or poor, communities with very good or excellent emergency department services had one third fewer open FP practices. No statistically significant difference in the likelihood of having open practices was observed between places seen to have good emergency department services and areas seen to have fair or poor services.
If availability of medical services in the community was not seen as a problem or was seen as a minor problem, practices were 1.3 times more likely to be open than if availability was seen as a severe problem. There was no statistically significant difference between communities where availability of medical services was seen as a moderate problem and communities where it was seen as a major problem.
DISCUSSION
It is interesting that family members and friends of current patients and patients referred by other physicians are likely to be able to enter conditionally closed practices, while people without connection to the practice are not. About 9% of FPs accepted patients only if they had certain medical problems, which suggests that they had specialized within a given area. Almost the same proportion of FPs closed their practices to patients with certain medical problems or of certain ages, however, suggesting an attempt to avoid dealing with patients or problems that FPs felt less comfortable in handling.
Our analysis suggests that practice and physician characteristics affect whether practices are open, conditionally closed, or completely closed. The odds of having an open practice increase if the FP is male, younger, currently working fewer hours, or working in a group practice. But the broader practice environment is just as important.
Family physicians with open practices appear to be responding to the medical care needs in their communities. Family physicians tend to keep their practices open when emergency department services are restricted. Family physicians in rural and remote areas are much less likely than those in cities or places near urban centres to close their practices, possibly because rural residents have few medical care alternatives. On the other hand, FPs are more likely to close their practices when they believe their communities have adequate emergency department services or when they think that many local FPs have closed practices. The latter could be a defensive move to avoid being overwhelmed by new patients who cannot find other FPs.
Family physicians who worked with other specialists in group practices were more likely to accept new patients. One possible explanation is that FP-and-specialist group practices tend to involve a greater number of physicians. Our findings suggest that having a larger number of health care providers working together is a way to keep practices open. Current health care policies appear to encourage physicians to work in larger networks of service providers.7-9
Clearly, our analysis offers just a snapshot taken at a particular time. The phenomenon of open and closed practices is a fluid one, changing from time to time in response to an evolving health care system, shifting medical service conditions in communities, and changing personal circumstances. While doing a study of Ontario FPs during the mid-1990s, we found that practice status could be quite changeable.10
Our study was constrained by some data limitations. For instance, it would be helpful if we had known how many months during the year a practice was completely or conditionally closed, and so forth. But these complex questions are difficult to pose in mailed surveys. Information on the size of group practices, while sought in the survey, was not given in ways that would produce reliable data; consequently, such data were not used in this analysis.
CONCLUSION
Increasing restrictions of the range of services offered in office-based primary care practice, restrictions on the types of patients seen, and the closure of practices to new patients are a growing concern for patients, policy makers, and politicians. The most recent (2004) National Physician Survey suggests that the extent to which FPs are closing their practices (18.2% in 2004 compared with 6.8% in 2001) is increasing, while the number of open practices is decreasing (20.2% compared with 25.7%).11 Although the way the question was asked differs slightly, the 2004 responses suggest that the problem of practice closure has become more serious than it was in 2001.
Our analysis suggests that FPs attempt to be responsible about limiting the size of their practices and appear to keep their practices open when patients have few medical care alternatives. Although demographic and practice characteristics affect whether practices are open, conditionally closed, or completely closed, the broader practice environment, such as geographic location and medical service conditions in the community, is equally important.
Our study has important implications. There is a need to re-examine current models of primary care and develop new models that will allow physicians to practise high-quality medicine while ensuring reasonable access to primary care services for the population. There are no easy ways to ensure that every Canadian will have ready access to an FP, regardless of where he or she lives. Our findings shed some light on the extent of the problem and the complexity of the issues involved.
Metropolitan influenced zones.
According to our study’s definition,5 “rural” refers to small communities outside the commuting zone of an urban centre called a metropolitan influenced zone (MIZ). Rural areas can be further divided into zones according to the strength of a city’s influence. Strong MIZ communities are those with 30% or more of their employed labour force working in urban areas. Moderate MIZ communities are those with at least 5% but less than 30% of their employed labour force working in urban areas. Weak MIZ communities are those with no more than 5% of their employed labour force working in urban areas. No MIZ communities are those with a very small employed labour force or no residents working in urban centres.
Acknowledgments
We thank the College of Family Physicians of Canada for granting permission to use the 2001 National Family Physician Workforce Survey data for this study. We also thank Dr J. Roger Pitblado of the Centre for Rural and Northern Health Research (CRaNHR) for doing the postal code conversion, Mr John Hogenbirk of CRaNHR for his assistance in analyzing the data, and Mr Vince Guerin of CRaNHR for formatting the tables.
Biographies
Dr Woodward is with the Centre for Health Economics and Policy Analysis and the Department of Clinical Epidemiology and Biostatistics at McMaster University in Hamilton, Ont.
Dr Pong is with the Centre for Rural and Northern Health Research and the Northern Ontario School of Medicine at Laurentian University in Sudbury, Ont.
Footnotes
Competing interests: None declared
References
- 1.College of Physicians and Surgeons of Ontario. A snapshot of the profession. Members’ Dialogue. 2003;11(5):8–11. [Google Scholar]
- 2.White G. Family physicians—looking in the mirror [editorial]. Can Fam Physician. 2003;49:1431. 1431-2 (Eng), 1435-7 (Fr) [PMC free article] [PubMed] [Google Scholar]
- 3.Hanson C. Family doctors turning people away: some physicians screening clients. Toronto Star Saturday, 2003 Oct. p. 1. R1, R3.
- 4.College of Family Physicians of Canada. The Janus project: Family physicians meeting the needs of tomorrow’s society: Results of the 2001 National Family Physician Workforce Survey. Mississauga, Ont: College of Family Physicians of Canada; 2002. [cited 2005 Nov 10]. Available from: http://www.cfpc.ca/English/cfpc/research/janus%20project/nfpws/default.asp?.s=1. [Google Scholar]
- 5.Woodward CA, Williams AP, Cohen M, Ferrier B. Closed and restricted practices. Recent family medicine graduates place limits on services. Can Fam Physician. 1997;43:1541–1547. [PMC free article] [PubMed] [Google Scholar]
- 6.du Plessis V, Beshiri R, Bollman RD, Clemenson H. Definitions of “rural”. Working paper #6. Ottawa, Ont: Agriculture Division, Statistics Canada; 2001. [Google Scholar]
- 7.Hamilton J. Quebec looks to rejig family practice. CMAJ. 2002;167(5):532. [PMC free article] [PubMed] [Google Scholar]
- 8.Hilditch JR. Changes in hospital emergency department use associated with increased family physician availability. J Fam Pract. 1980;11(1):91–96. [PubMed] [Google Scholar]
- 9.Romanow RJ. Building on values: the future of health care in Canada. Saskatoon, Sask: Commission on the Future of Health Care in Canada; 2002. [Google Scholar]
- 10.Brown JA, Abelson J, Woodward CA, Hutchison B, Norman GR. Fielding standardized patients in primary care settings. Int J Qual Health Care. 1998;10(3):199–206. doi: 10.1093/intqhc/10.3.199. [DOI] [PubMed] [Google Scholar]
- 11.College of Family Physicians of Canada. [cited 2005 November 24];National Physician Survey (NPS) 2004: Workforce, satisfaction and demographic statistics concerning current and future physicians in Canada. February 15, 2005: Physician statistical data tables. Extent to which Family Physicians are accepting new patients (Q17FP). Available from: http://www.cfpc.ca/nps/English/pdf/Physicians/Family_Physicians/Tables/Summary-Table/Q17FP.pdf.