Abstract
We evaluated the effectiveness of a dentist-implemented behavioral intervention in which brief escape from dental treatment was provided on a regular basis, independent of the child's behavior. Within a multiple baseline design across subjects, 5 children, ages 4 to 7 years, were provided with temporary escape from dental treatment on a fixed-time schedule. The intervals were signaled by an electronic timer worn by the dentist. Clinically significant reductions were observed in physically disruptive behavior across all 5 children with the introduction of noncontingent escape, and verbally disruptive behavior was markedly reduced in 4 of the 5 children. In addition, the dental staff's use of physical restraint was reduced to near zero across all 5 children. The research extends the literature in both clinical dentistry and in applied behavior analysis by demonstrating that a dentist can easily and effectively implement noncontingent reinforcement to produce clinically significant and socially important changes in children's health behavior.
Keywords: noncontingent reinforcement, escape, dental visits, disruptive behavior
For children undergoing restorative dental treatment, a visit to the dentist can feature pinching, pressure, scraping, and a host of unpleasant sounds, foreign tastes, and uncomfortable, painful sensations. By nature, restorative dental work is invasive. The only positive outcome for a child is a clean bill of health and not having to return until the next check-up. The least favorable outcome is the promise of additional visits requiring more invasive procedures. It should come as no surprise that the dental clinic is a place many children would like to avoid.
As a result, children undergoing restorative dental treatment can be very disruptive and difficult to manage. Common disruptive behaviors such as crying, wiggling, kicking, and tantrums (Carr, Wilson, Nimer, & Thorton, 1999; Pinkham, 1999) can make dental procedures more difficult by requiring extra time and effort (Kuhn & Allen, 1994). In addition, sudden movements and other disruptive behaviors during invasive procedures may expose the child to increased risk of injury. Although most children seen in clinical practice are well behaved, recent estimates suggest that 20% to 25% of all children exhibit disruptive problems at the dentist (Brill, 2000; Raadal, Milgrom, & Weinstein, 1995). In addition, these problems are strongly correlated with age, with younger preschool-aged children being more challenging than school-aged children (Allen, Hutfless, & Larzelere, 2003). Furthermore, these problems are compounded when invasive procedures are required. For example, data from private practice suggest that the younger the child and the more threatening or invasive the procedure, the more often negative disruptive behavior is observed (Brill, 2000). Indeed, dentists agree that the young child requires considerable effort for effective management (Pinkham, 1999), and many general practitioners are not willing to provide young children with anything more than an examination or prophylaxis care (Cotton et al., 2001).
Over the years, numerous interventions have been developed in an effort to help dentists manage the disruptive behavior of children during dental treatment. Pharmacological interventions have included general anesthesia, nitrous oxide, and conscious sedation (Carr et al., 1999; Pinkham, 1999). Although they are effective, drugs can produce untoward side effects that present markedly increased dangers in smaller children (Pinkham). Invasive behavior-management techniques such as reprimands and restraint have also been shown to reduce disruptive behavior, but are not acceptable to parents (Allen, Hodges, & Knudsen, 1995; Peretz & Zadik, 1999). In addition, both anesthesia and restraint procedures come with increased legal risk (e.g., Bross, 2004).
In response, the American Academy of Pediatric Dentistry has appealed to researchers to develop alternative noninvasive behavior-management techniques (McTigue, 2004). Behavioral researchers have been involved in these efforts, investigating distraction procedures (e.g., Filcheck et al., 2004), modeling techniques (e.g., Conyers et al., 2004), and even pain-reduction procedures (Allen, Kotil, Hutfless, Larzelere, & Beiraghi, 2002). In addition, the use of contingent escape for cooperative behavior has been explored as a noninvasive means of reducing disruptive behavior in the clinic. The use of contingent escape evolved from a functional assessment that suggested that the unpleasant sensations associated with invasive dental procedures had established escape as a potent reinforcer and, as a result, evoked behavior that had resulted previously in escape from unpleasant situations (e.g., crying, thrashing, pushing away or blocking instruments) (Allen & Stokes, 1989). Disruptive behavior during dental treatment that resulted in brief, intermittent access to escape (i.e., reinforcement) could be expected to continue. Also, observations suggested that cooperative behavior typically resulted in the continuation of invasive treatment (i.e., punishment). In the original contingent escape procedure, this contingency was reversed; brief periods of escape from ongoing dental treatment were provided contingent on cooperative behavior (e.g., lying still, being quiet) while disruptive behavior was placed on extinction. In a series of investigations, contingent escape was found to result in dramatic and rapid reductions in the disruptive behavior of young children (Allen, Loiben, Allen, & Stanley, 1992; Allen, Stark, Rigney, Nash, & Stokes, 1988; Allen & Stokes, 1987).
Nevertheless, the contingent escape procedure required both training of and vigilance by the dentist. Unfortunately, dentists are not reimbursed for time spent engaged in behavior management, nor are they reimbursed for learning those skills (Sheller, 2004). So, although data from previous studies suggested that the procedure did not require more time to implement than traditional behavior-management procedures (e.g., Allen et al., 1992), the training did take time. In addition, the contingency requires continued effort by the dentist, who must monitor the child's behavior and make judgments about whether and when to deliver escape. Perhaps not surprisingly, Allen et al. (1992) found that maintaining adherence to the protocol was challenging, a problem that has been observed in similar situations that place high task demands on the behavior-change agents (e.g., Vollmer, Marcus, & Ringdahl, 1995). Thus, there remains a need to develop effective procedures that require less response effort.
One possible means of reducing the response effort associated with the contingent escape procedure is to remove the contingency and therefore the need to continuously monitor behavior. The traditional model of noncontingent reinforcement is comprised of a fixed-time (FT) schedule of reinforcement (in which reinforcement is delivered based on time), extinction (during which no contingent consequences are delivered), and schedule thinning (in which the schedule of noncontingent reinforcement is gradually thinned) (Marcus & Vollmer, 1996; Vollmer, Iwata, Zarcone, Smith, & Mazaleski, 1993). Noncontingent reinforcement guarantees more consistent delivery of the reinforcement, and because the procedure is time based rather than performance based, it improves the ease of implementation (Hagopian, Fisher, & Legacy, 1994; Lalli, Casey, & Kates, 1997; Vollmer et al., 1993). That is, the change agent must be familiar with the schedule (i.e., time) of reinforcement but is not required to struggle with the decision criteria required by other contingency-based interventions (Kahng, Iwata, DeLeon, & Wallace, 2000). The ease of implementation may result in greater adherence to the intervention protocol and ultimately to greater maintenance of gains (Tucker, Sigafoos, & Bushell, 1998).
To date, applications of noncontingent reinforcement to reduce escape-maintained behaviors have typically focused on instructional settings (e.g., Kodak, Miltenberger, & Romaniuk, 2003; Vollmer et al., 1995). In addition, past studies of noncontingent escape (NCE) typically have relied on individuals with advanced training in behavior-change methods to implement the procedures. In the only exception we could find, Coleman and Holmes (1998) demonstrated that speech therapists with little formal training in behavior analysis could effectively implement a NCE procedure to reduce disruptive behavior. Yet, it remains unknown whether an untrained provider can implement NCE procedures effectively in a typical health-care setting during routine health-care delivery.
The purpose of the present study was twofold. First, the intent was to extend applied research on the development of noninvasive techniques to manage disruptive behavior during restorative dentistry by investigating the efficacy of NCE in the dental clinic. Second, we hoped to expand the applied behavioral literature by investigating whether dentists could, without formal training in behavioral technology, implement NCE effectively.
Method
Participants and Setting
Five children, ranging from 4 to 7 years old (3 girls and 2 boys), had been referred from a large midwestern university pediatric dental clinic due to significant problems with disruptive behavior. Children were required to need at least three visits for tooth preparation and restoration procedures to be included in the study. Consistent with standard clinic procedures, the visits were scheduled once a week, with each visit lasting between 45 and 90 min. There were no restrictions based on gender, race, or ethnic origin. Children with cognitive disabilities and those who did not speak English were excluded.
Apparatus
During the treatment condition, a MotivAider® was attached to the dentist's waistband to signal time-based breaks. This pager-sized device emits a pulsing vibration on a fixed-time schedule that can range from once every second to once every 24 hr. In addition, a videocamera recorded all baseline and treatment sessions. The camera was placed on a tripod in one corner of the examination room.
Measures
Child Behavior
Child behavior, including body movements, complaints, moaning, and crying, were recorded on a 15-s partial-interval schedule (Allen et al., 1992). Body and head movements were coded if either one continuous motion or smaller repetitive motions (without interruption of 1 s or more) were observed by any body movement of 15 cm or more or by any head movement of 15 mm or more. Complaints or crying was coded for any crying, moaning, gagging, or complaining about dental procedures or pain. Complaints in response to questions by the dentist were not scored. Scoring began when the dentist or dental assistant looked at and touched the child's mouth. Both looking and touching were required before coding because this represented when restorative dental work officially began; either looking or touching might occur independently but would not be sufficient to conduct restorative dental work. Scoring was discontinued 5 s after the dentist looked away or stopped touching the child.
Staff Behavior
The number of physical restraints of the child was recorded. Restraints included holding of any part of the child's body by a dental assistant to restrict movement. Light touches to calm or comfort the child were not scored.
Reliability
A predoctoral intern scored the child's and dentist's behaviors. Another predoctoral intern, naive to the experimental hypothesis, served as a reliability observer. Each observer was trained to 85% agreement. Reliability observations were conducted on 29% of the observations. Interobserver reliability was determined by calculating the number of agreements between observers on the occurrence and nonoccurrence of disruptive behavior, dividing by the number of agreements plus disagreements, and multiplying by 100%. Overall reliability for disruptive behavior was 91% (range, 79% to 100%).
Treatment Integrity
To ensure the integrity of the independent variable, the dentist's use of the NCE contingency was recorded. The observers maintained a simple frequency count of the occurrence of each break. The total number of actual breaks was compared to the total projected by the schedule of breaks. Integrity of the NCE procedure was calculated for 55% of dental visits and was found to be 94% (range, 86% to 100%).
Design and Procedure
Design
The investigation used a multiple baseline across subjects design. Baseline and experimental conditions were introduced across subjects after varying numbers of visits.
Baseline
Procedures during baseline were those typically followed at the dental clinic. A routine restorative dental visit typically began with the dentist examining the teeth that required restoration (i.e., repairs), applying the topical anesthetic (benzocaine), and injecting the local anesthetic (lidocaine). Next, the dentist placed a mouth prop between the upper and lower teeth and began removal of the tooth decay via a dental handpiece (i.e., drill). The appointment concluded with the placement of the dental restoration (e.g., filling, crown). Prior to each step of the treatment, the dentist explained what would be done and the sensations that the child might experience and delivered praise for being cooperative. Following treatment, each patient received a prize (e.g., stickers, balls, toy jewelry) regardless of his or her behavior.
Treatment
The dentist was fitted with the MotivAider® and was instructed to follow standard dental procedures. Prior to the start of treatment, the dentist showed the patient the device and said, “Look at this pager. It tells me when we are supposed to rest. Whenever it buzzes, we will stop and take a break.” Initially, the frequency of the breaks occurred often (FT 15 s). The length of these intervals was selected based on a relatively rich schedule compared to what is typically available in this setting. During the visit, the observer, who was present during each examination, sat quietly coding behavior, and there were no interactions with the dentist other than to prompt the dentist to thin the schedule of reinforcement so that increasingly longer periods of time passed before a break was taken. The observer prompted the dentist to thin the schedule by 10- to 20-s increments based on low occurrences of disruptive behavior until a terminal schedule of FT 1 min was reached.
Prior to the start of dental treatment, the dentist conducted 2 min of practice with the child. All breaks throughout practice and treatment lasted approximately 10 s. The child was positioned in the dental chair, and the dentist stated, “Let's practice our breaks. Some breaks will happen often and sometimes they will take longer.” The dentist placed instruments to be used during treatment inside the child's mouth, but only feigned dental treatment until the MotivAider® signaled the break. On feeling the vibration, the dentist stated, “It's break time.” Breaks during practice occurred at 10-s intervals for the 1st min and at 20-s intervals for the 2nd min. The practices were conducted to allow the child the opportunity to experience breaks and how they would be provided. The initial schedule of 10 s was used to yield a high number of exposures to NCE. The FT 20-s schedule allowed practices to occur with a leaner schedule of reinforcement. At the end of the practice sessions, the dentist proceeded with the standard treatment until the next break was signaled. During breaks, the dentist removed all instruments and fingers from the child's mouth. The child was allowed to sit up and move freely. When breaks ended, the child was repositioned as is typically done at the onset of treatment. Although the breaks were intended to occur only when scheduled, the dentist was permitted to remove burs, needles, or other sharp instruments to reduce the risk of injury in cases of severe disruptive behavior and was told to manage disruptive behavior as he or she typically would.
Results
Baseline
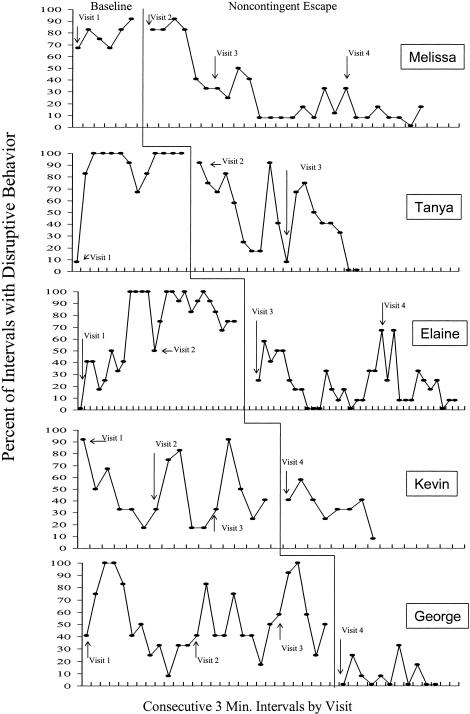
The frequency of occurrence of disruptive behavior for each child during each restorative dental treatment visit is presented in Figure 1. During baseline, high or increasing rates of disruptive behavior were evident for 3 of the participants (Melissa, Elaine, and Tanya), whereas 2 participants (Kevin and George) showed initially high levels of disruptive behavior that decreased to moderate levels near the end of each visit. This pattern was repeated across three baseline visits and was considered stable before treatment was introduced. This within-session downward trend is a common occurrence during dental treatment, when procedures performed in the early part of a visit (i.e., injections, drilling, etc.) are more invasive and tend to occasion more escape behavior than in the latter part of a visit. Therefore, results are best evaluated by comparing mean disruptive behavior for each visit or by comparing baseline visits with intervention visits interval by interval.
Figure 1. Percentage of 15-s intervals containing disruptive behavior per 3 min of treatment for each child across subsequent visits.
Treatment
With the introduction of NCE, there were marked reductions in disruptive behavior for 4 of the children. For 3 of the participants (Elaine, George, and Tanya), these reductions were observed within the first session that NCE was implemented. For Melissa, reductions were not clearly evident until her second treatment visit. However, Melissa continued to experience reductions at subsequent visits, as did Elaine and Tanya. By the conclusion of treatment, these 4 individuals had experienced, on average, a 56% reduction in disruptive behavior.
Figure 1 also shows that, unlike the other 4 participants, Kevin did not exhibit marked reduction in overall disruptive behavior. Mean levels of disruptive behavior between baseline and treatment were only marginally different (47% and 35%, respectively), and there is considerable overlap in data points across conditions. However, in contrast to the three baseline visits in which disruptive behavior was quite frequent during the first 6 to 10 min of each visit, Kevin did exhibit a marked reduction in the frequency of disruptive behavior early in the NCE treatment visit.
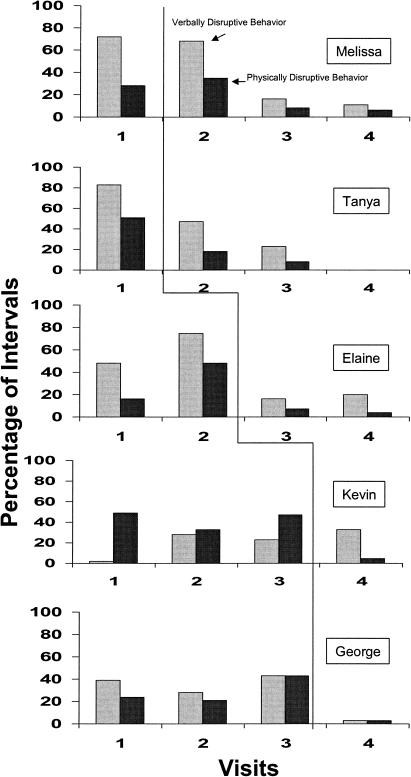
In an effort to more closely analyze the impact of NCE on specific response topographies, the mean verbally disruptive (i.e., complaining and crying) and physically disruptive (i.e, body and head movement) behavior rates were examined for each individual. Figure 2 shows that, as expected, the reductions in disruption observed for Melissa, Elaine, George, and Tanya reflect corresponding reductions in both verbally and physically disruptive behavior. However, data for Kevin reveal that verbally and physically disruptive behaviors responded differentially to the NCE treatment. The occurrence of verbally disruptive behavior increased from an average of 17% of baseline intervals to 33% in treatment, whereas physically disruptive movements decreased from 43% in baseline to 5% in the treatment phase.
Figure 2. Percentage of verbally disruptive behavior (light shaded bars) and physically disruptive behavior (dark shaded bars) per visit for each child across baseline and treatment.
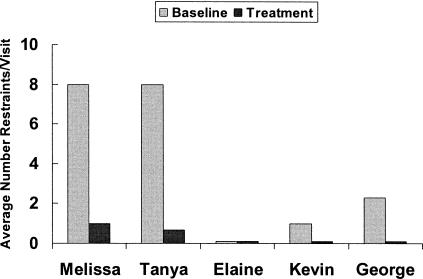
The coding system not only provided measures of disruptive behavior frequency but also was an indirect measure of response intensity. The number of restraints used each session was coded and provided a direct measure of staff behavior and an indirect measure of the intensity of child disruptiveness. Figure 3 shows the average number of times restraint was used per visit by the dental staff for each participant in baseline and in treatment. These results demonstrate that NCE was effective in reducing the number of restraints used for managing Melissa, Tanya, Kevin, and George. Elaine did not require any restraints in baseline or treatment conditions.
Figure 3. Average number of restraints per visit in baseline (light shaded bars) and in treatment (dark shaded bars) for each child.
Discussion
Overall, the results of this investigation demonstrate that the use of NCE by a dentist was an effective means of reducing the disruptive behavior of 5 young children undergoing restorative dental treatment. Physically disruptive behavior was markedly reduced in all 5 children, and verbally disruptive behavior was markedly reduced in 4 of them. In addition, the dental staff's use of physical restraint was reduced to near zero. This last factor is particularly important because the required use of restraint has been found to be the single best predictor of dentists' satisfaction with children's behavior (Allen et al., 2003). Finally, at the conclusion of treatment, overall disruptive behavior for each child occurred, on average, less than 30% of the time, a rate that has been found to be acceptable by dentists (Ingersoll, Nash, & Gamber, 1984).
This study extends a line of previous research demonstrating that exposing children to temporary escape can be an effective means by which to manage disruptive behavior in the dental setting (Allen et al., 1988, 1992; Allen & Stokes, 1987). Although previous studies demonstrated the effectiveness of contingent escape, this investigation demonstrated that the noncontingent delivery of escape also can produce clinically significant changes in behavior. In addition, the effects were achieved with greater ease of implementation. No more than a few minutes were required to explain the protocol to the dentist and familiarizing him with the cuing device, and yet high levels of treatment integrity were observed. No expensive equipment was necessary, nor was standard dental treatment significantly altered. This is important because previous investigations of efforts to apply behavioral technology in dental settings have cited limitations related to procedural drift, time spent training personnel, and knowledge and effort required to implement techniques appropriately (Allen et al., 1988, 1992; Allen & Stokes, 1987; Stark et al., 1989; Stokes & Kennedy, 1980). The improved ease of implementation may mean that the technique is more likely to be used and adhered to, which may increase the effectiveness of NCE and decrease the need to rely on more invasive means to manage behavior (Tucker et al., 1998).
This investigation also extends the applied behavior-analytic literature regarding the clinical applications of NCE. Relatively few studies have evaluated the effects of NCE in clinical contexts, and this is the first study to evaluate its effects in a health-care setting. Although many recent researchers have chosen to study novel, arbitrary responses in an attempt to better understand the mechanisms by which NCE produces its effects (e.g., Ecott & Critchfield, 2004; Ringdahl, Vollmer, Borrero, & Connell, 2001), studies in applied settings with socially relevant behaviors remain important. This investigation demonstrated that NCE can be an effective intervention in a relatively uncontrolled clinical setting with typical children who exhibit clinically significant problem behaviors. The present study also extends the results of Coleman and Holmes (1998) by demonstrating the practical utility of the NCE procedure, implemented here by a service provider with no formal training in behavior analysis. This type of study can be important for the dissemination of applied behavior analysis as a discipline that possesses technology that can promote the development and maintenance of child health behavior (Allen, Barone, & Kuhn, 1993).
Interestingly, the effects of the noncontingent reinforcement procedure were immediate for several of the children and more delayed for others. Explaining these differences can be challenging. In trying to understand how noncontingent reinforcement produces changes in behavior, researchers have speculated about the role of extinction (i.e., disruptions in the response–reinforcer contingency), satiation (i.e., a disestablishing operation), and adventitious reinforcement (i.e., the noncontingent reinforcement accidentally strengthens an alternative behavior) (Ecott & Critchfield, 2004). The increased availability of escape may have served as an abolishing operation for escape-maintained behavior; however, this investigation does not provide specific insights about mechanisms of change, and it is unclear whether one or more mechanisms played a role.
The fact that the dentist was able to implement the NCE procedure with relatively little training and almost no disruption to his usual routine is at once a strength and a limitation of the investigation. For example, the dentist was free to use other management techniques as needed (e.g., restraint, verbal redirection, praise) and did so on a regular basis. Although baseline observations suggest that these interventions were ineffective in reducing significant problem behaviors, their interactive effects, when combined with NCE, are unknown. Thus, praise for desirable behaviors (i.e., lying still, following dentist's directions, remaining calm) appeared to have little impact during baseline but may have contributed to the effects of NCE during intervention. Indeed, Kodak et al. (2003) speculated that praise might be an effective reinforcer of appropriate behavior only after NCE reduces escape behavior. In addition, extinction-based procedures have often been found to be more effective when combined with other techniques (Cooper, 1987; Marcus & Vollmer, 1996), and the same may be true for NCE.
The investigation also is limited by the absence of a systematic approach to thinning the schedule of reinforcement. That is, although the intervention phase began with all children obtaining escape on an FT 15-s schedule, there was no specific rule for thinning the schedule other than subjective evaluations of improvement. This was done, in large part, to maintain the ease of implementation for the dentist, because calculations of specific disruptive behavior rates would have permitted data-based decision making but would have been prohibitive for the dentist. As a result, the exact schedule of thinning cannot be replicated, and implementation was dependent, in part, on the observer prompting the dentist to thin the schedule. In addition, the cuing device itself introduced some complications because it could program only one schedule of reinforcement at a time, requiring the dentist to suspend dental treatment momentarily to set the new schedule (e.g., FT 25 s) when thinning was desired. Even this small amount of response effort could, over time, result in a dentist abandoning the procedure. Future studies should look at automating the schedule thinning to further simplify the procedure, reduce response effort, and make the dentist completely self-sufficient. Ultimately, applied behavior analysis is not only about establishing efficacious interventions but is also about finding procedures that are responsive to the context in which the services are to be provided.
Acknowledgments
This research was based in part on a doctoral dissertation submitted to Louisiana State University by the first author under the supervision of the second author. Thanks to Mary Lou Kelley, George Noell, Drew Gouvier, and Nathan Call for comments on an earlier version of this manuscript.
References
- Allen K.D, Barone V.J, Kuhn B. A behavioral prescription for promoting behavior analysis within pediatrics. Journal of Applied Behavior Analysis. 1993;26:493–502. doi: 10.1901/jaba.1993.26-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen K.D, Hodges E.D, Knudsen S.K. Comparing four methods to inform parents about child behavior management: How to inform for consent. Pediatric Dentistry. 1995;17:180–185. [PubMed] [Google Scholar]
- Allen K.D, Hutfless S, Larzelere R. Evaluation of two predictors of child disruptive behavior during restorative dental treatment. Journal of Dentistry for Children. 2003;70:221–225. [PubMed] [Google Scholar]
- Allen K.D, Kotil D, Hutfless S, Larzelere R, Beiraghi S. Comparison of computerized anesthesia delivery with traditional syringe in preschool children. Pediatric Dentistry. 2002;24:315–320. [PubMed] [Google Scholar]
- Allen K.D, Loiben T, Allen S.J, Stanley R.T. Dentist-implemented contingent escape for management of disruptive child behavior. Journal of Applied Behavior Analysis. 1992;25:629–636. doi: 10.1901/jaba.1992.25-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen K.D, Stark L.J, Rigney B.A, Nash D.A, Stokes T.F. Reinforced practice of children's cooperative behavior during restorative dental treatment. Journal of Dentistry for Children. 1988;55:273–277. [PubMed] [Google Scholar]
- Allen K.D, Stokes T.F. The use of escape and reward in the management of young children during dental treatment. Journal of Applied Behavior Analysis. 1987;20:381–390. doi: 10.1901/jaba.1987.20-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen K.D, Stokes T.F. Pediatric behavioral dentistry. In: Hersen M, Eisler R, Miller P, editors. Progress in behavior modification. Newbury Park, CA: Sage; 1989. pp. 60–90. In. Eds. [PubMed] [Google Scholar]
- Brill W.A. Child behavior in a private pediatric dental practice associated with types of visits, age, and socio-economic factors. Journal of Clinical Pediatric Dentistry. 2000;25(1):1–7. doi: 10.17796/jcpd.25.1.545025p1g72x730q. [DOI] [PubMed] [Google Scholar]
- Bross D.C. Managing pediatric dental patients: Issues raised by the law and changing views of proper child care. Pediatric Dentistry. 2004;26:125–130. [PubMed] [Google Scholar]
- Carr K.R, Wilson S, Nimer S, Thorton J.B. Behavior management techniques among pediatric dentists practicing in the southeastern United States. Pediatric Dentistry. 1999;21:347–353. [PubMed] [Google Scholar]
- Coleman C.L, Holmes P.A. The use of noncontingent escape to reduce disruptive behavior in children with speech delays. Journal of Applied Behavior Analysis. 1998;31:687–690. doi: 10.1901/jaba.1998.31-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conyers C, Miltenberger R, Maki A, Barenz R, Jurgens M, Sailer A, et al. A comparison of response cost and differential reinforcement of other behavior to reduce disruptive behavior in a preschool classroom. Journal of Applied Behavior Analysis. 2004;37:411–415. doi: 10.1901/jaba.2004.37-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper J.O. Extinction. In: Cooper J.O, Heron T.E, Heward W.L, editors. Applied behavior analysis. Englewood Cliffs, NJ: Prentice Hall; 1987. pp. 255–274. In. Eds. [Google Scholar]
- Cotton K.T, Seale N.S, Kanellis M.J, Damiano P.C, Bidaut-Russell M, McWhorter A.G. Are general dentists' practice patterns and attitudes about treating Medicaid-enrolled preschool age children related to dental school training? Pediatric Dentistry. 2001;23:51–55. [PubMed] [Google Scholar]
- Ecott C.L, Critchfield T.S. Noncontingent reinforcement, alternative reinforcement, and the matching law: A laboratory demonstration. Journal of Applied Behavior Analysis. 2004;37:249–265. doi: 10.1901/jaba.2004.37-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filcheck H, Allen K.D, Ogren H, Darby B, Holstein B, Hupp S. The use of choice-based distraction to decrease the distress of children at the dentist. Child & Family Behavior Therapy. 2004;26(4):59–68. [Google Scholar]
- Hagopian L.P, Fisher W.W, Legacy S.M. Schedule effects of noncontingent reinforcement on attention-maintained destructive behavior in identical quadruplets. Journal of Applied Behavior Analysis. 1994;27:317–325. doi: 10.1901/jaba.1994.27-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B.D, Nash D.A, Gamber C. The use of contingent audiotaped material with pediatric dental patients. Journal of the American Dental Association. 1984;109:717–719. doi: 10.14219/jada.archive.1984.0170. [DOI] [PubMed] [Google Scholar]
- Kahng S.W, Iwata B.A, DeLeon I.G, Wallace M.D. A comparison of procedures for programming noncontingent reinforcement schedules. Journal of Applied Behavior Analysis. 2000;33:223–231. doi: 10.1901/jaba.2000.33-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodak T, Miltenberger R.G, Romaniuk C. The effects of differential negative reinforcement of other behavior and noncontingent escape on compliance. Journal of Applied Behavior Analysis. 2003;36:379–382. doi: 10.1901/jaba.2003.36-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn B.R, Allen K.D. Expanding child behavior management technology in pediatric dentistry: A behavioral science perspective. Pediatric Dentistry. 1994;16:13–17. [PubMed] [Google Scholar]
- Lalli J.S, Casey S.D, Kates K. Noncontingent reinforcement as treatment for severe problem behavior: Some procedural variations. Journal of Applied Behavior Analysis. 1997;30:127–137. doi: 10.1901/jaba.1997.30-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus B.A, Vollmer T.R. Combining noncontingent reinforcement and differential reinforcement schedules as treatment for aberrant behavior. Journal of Applied Behavior Analysis. 1996;29:43–51. doi: 10.1901/jaba.1996.29-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McTigue D.J. Behavior management for the pediatric dental patient. Pediatric Dentistry. 2004;26:110. [PubMed] [Google Scholar]
- Peretz B, Zadik D. Parents' attitudes toward behavior management techniques during dental treatment. Pediatric Dentistry. 1999;21:201–204. [PubMed] [Google Scholar]
- Pinkham J.R, editor. Pediatric dentistry: Infancy through adolescence (3rd ed.) Philadelphia: Saunders; 1999. Ed. [Google Scholar]
- Raadal M, Milgrom P, Weinstein P. The prevalence of dental anxiety in children from low income families and its relationship to personality traits. Journal of Dental Research. 1995;74:1439–1443. doi: 10.1177/00220345950740080201. [DOI] [PubMed] [Google Scholar]
- Ringdahl J.E, Vollmer T.R, Borrero J.C, Connell J.E. Fixed-time schedule effects as a function of baseline reinforcement rate. Journal of Applied Behavior Analysis. 2001;34:1–15. doi: 10.1901/jaba.2001.34-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheller B. Challenges of managing child behavior in the 21st century dental setting. Pediatric Dentistry. 2004;26(2):111–113. [PubMed] [Google Scholar]
- Stark L.J, Allen K.D, Hurst M, Nash D.A, Rigney B, Stokes T. Distraction: Its utilization and efficacy with children undergoing dental treatment. Journal of Applied Behavior Analysis. 1989;22:297–307. doi: 10.1901/jaba.1989.22-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes T.F, Kennedy S.H. Reducing child uncooperative behavior during dental treatment through modeling and reinforcement. Journal of Applied Behavior Analysis. 1980;13:41–49. doi: 10.1901/jaba.1980.13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker M, Sigafoos J, Bushell H. Use of noncontingent reinforcement in the treatment of challenging behavior: A review and clinical guide. Behavior Modification. 1998;22:529–547. doi: 10.1177/01454455980224005. [DOI] [PubMed] [Google Scholar]
- Vollmer T.R, Iwata B.A, Zarcone J.R, Smith R.G, Mazaleski J.L. The role of attention in the treatment of attention-maintained self-injurious behavior: Noncontingent reinforcement and differential reinforcement of other behavior. Journal of Applied Behavior Analysis. 1993;26:9–21. doi: 10.1901/jaba.1993.26-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer T.R, Marcus B.A, Ringdahl J.E. Noncontingent escape as treatment for self-injurious behavior maintained by negative reinforcement. Journal of Applied Behavior Analysis. 1995;28:15–26. doi: 10.1901/jaba.1995.28-15. [DOI] [PMC free article] [PubMed] [Google Scholar]