Abstract
OBJECTIVE
To examine self-reported health care use and health care–seeking behaviour of patients meeting DSM-IV’s diagnostic criteria for generalized anxiety disorder (GAD).
DESIGN
Survey of outpatients recruited at three different times of the day using questionnaires on worry and anxiety (a six-item screening questionnaire based on DSM-IV criteria for GAD), on perceived health problems, and on health care use and health care–seeking behaviour. The assessment package also included well validated assessment instruments for insomnia and depression symptoms. All patients seeking health care were invited to participate. Participants completed the survey as they waited in the reception area.
SETTING
Four randomly selected community-based medical clinics of Quebec city’s metropolitan area.
PARTICIPANTS
A final sample of 1110 patients among 1878 outpatients invited to participate included 219 (19.7%) who tested positive for GAD.
MAIN OUTCOME MEASURES
Self-reported worry and anxiety (based on DSM-IV criteria for GAD), self-perceived health problems, health care use and health care–seeking behaviour, insomnia, and symptoms of depression.
RESULTS
Participants who tested positive on a screening test for GAD reported more annual medical visits (5.3 versus 3.4) than other patients. Those who reported at least five annual medical visits were nearly four times more likely to have positive results for GAD. Women were 1.6 times more likely to have positive results than men were. Patients who tested positive reported insomnia-type sleep disturbances, depressive symptoms, fatigue, and gastric problems significantly more often than others. Forty-two percent had consulted a family physician in the past year with a complaint of anxiety. Eighty percent of patients who tested positive reported they believed they had an anxiety problem, and this belief predicted positive test results (odds ratio = 20.3). Yet most reported not having sought other types of medical or psychological care specifically for anxiety in the past year.
CONCLUSION
Some patients in this sample with symptoms of GAD mainly seek primary care for their symptoms. Questions about excessive worrying and anxiety, as part of routine examination, can increase recognition of GAD.
Abstract
OBJECTIF
Examiner l’utilisation des services de santé et le comportement de recherche de soins rapportés par les patients répondant aux critères du DSM-IV pour l’anxiété généralisée (AG).
TYPE D’ÉTUDE
Enquête effectuée auprès de patients externes recrutés à trois moments différents de la journée à l’aide de questionnaires sur l’inquiétude et l’anxiété (questionnaire de dépistage de l’AG en six points basé sur les critères du DSM-IV), sur la perception qu’ils ont de leurs problèmes de santé, et sur leurs habitudes de recherche et d’utilisation des soins médicaux. L’évaluation comprenait aussi des outils éprouvés pour évaluer les symptômes d’insomnie et de dépression. Tous les patients qui consultaient pour des soins médicaux étaient invités à participer. Les participants ont répondu aux questions pendant qu’ils attendaient dans la salle d’attente.
CONTEXTE
Quatre cliniques médicales extra-hospitalières de la région métropolitaine de la ville de Québec.
PARTICIPANTS
Un total de 1878 patients ont été invités à participer. Sur les 1110 sujets finalement retenus, 219 (19,7%) répondaient aux critères d’AG.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Inquiétude et anxiété rapportées par les patients (selon les critères du DSM-IV pour l’AG), perception du patient de ses problèmes de santé, son comportement de recherche et d’utilisation des soins de santé, et la présence d’insomnie et de symptômes de dépression.
RÉSULTATS
Par rapport aux autres participants, ceux qui répondaient positivement au test de dépistage de l’AG déclaraient une plus grande fréquence de visites médicales (5,3 vs 3,4/an). Ceux qui avouaient en faire cinq ou plus par année avaient presque quatre fois plus de chances d’avoir un résultat positif pour l’AG. Les femmes avaient 1,6 fois plus de chances d’avoir des résultats positifs que les hommes. Les patients avec des résultats positifs rapportaient des troubles du sommeil de type insomnie, des symptômes de dépression, de la fatigue et des troubles gastriques avec une fréquence significativement plus élevée que les autres participants. Quarante-deux pour cent d’entre eux avaient consulté un médecin de famille pour un problème d’anxiété dans l’année précédente. Quatre-vingt pour cent des patients positifs ont dit qu’ils croyaient avoir un problème d’anxiété, et cette croyance permettait de prédire un résultat positif au dépistage (rapport de cotes = 20,3). Pourtant, la plupart déclaraient ne pas avoir cherché d’autres types d’aide médicale ou psychologique pour l’anxiété au cours de l’année précédente.
CONCLUSION
Certains des patients de cet échantillon qui présentent des symptômes d’AG s’adressent surtout aux services de santé primaires pour leurs symptômes. En posant des questions sur l’anxiété et l’inquiétude excessive durant un examen de routine, le médecin pourra mieux dépister l’AG.
EDITOR’S KEY POINTS.
Generalized anxiety disorder (GAD) is quite common among patients presenting to family doctors, but it is often unrecognized due to a focus on physical complaints as well as comorbidity with depression and other mental illness.
This community survey in Quebec city found that patients testing positive for GAD reported more annual medical visits to their doctors than those who tested negative. Those visiting more than five times were much more likely to have positive results for GAD.
While most patients who tested positive for GAD recognized that they had anxiety problems, they did not consult medical or psychological resources other than their family doctors. The burden of care is with family physicians.
Patients who tested positive for GAD frequently presented with symptoms of fatigue, depression, sleep disturbance, and gastric problems. Many patients were aware of their increased anxiety—cues for alert family physicians.
POINTS DE REPÈRE DU RÉDACTEUR.
L’anxiété généralisée (AG) est très fréquente chez les patients qui consultent le médecin de famille, mais elle est souvent ignorée parce qu’on s’attarde avantage aux problèmes physiques et qu’il y a présence de dépression ou d’autres maladies mentales concomitantes.
Cette enquête de terrain effectuée dans la ville de Québec a montré que les patients trouvés positifs au dépistage de l’AG déclaraient plus de visites annuelles à leur médecin que ceux qui avaient des résultats négatifs. Ceux qui consultaient plus de cinq fois avaient plus de chance d’avoir des résultats positifs pour l’AG.
La plupart des patients trouvés positifs au dépistage de l’AG reconnaissaient avoir des problèmes d’anxiété, et pourtant ils n’avaient pas recours à des ressources médicales ou psychologiques autres que leur médecin de famille. C’est surtout à ce dernier qu’incombe le fardeau des soins.
Les patients avec des résultats positifs pour l’AG consultaient fréquemment pour fatigue, dépression, troubles du sommeil et malaises gastriques. Plusieurs étaient conscients qu’ils présentaient des signes d’anxiété excessive susceptibles d’alerter leur médecin de famille.
Generalized anxiety disorder (GAD) is characterized by persistent excessive worry regarding a certain number of activities and events and by symptoms of anxiety. Worry, the core feature of GAD, is difficult to control and causes substantial distress and impairment in social, occupational, and other important spheres of daily life. Many somatic symptoms are associated with the presence of worry, but three of the following are compulsory for GAD diagnosis: restlessness, fatigue, inability to concentrate, irritability, tension, and disturbed sleep.1
Generalized anxiety disorder usually follows a long-term course with waxing and waning symptoms.1-3 Spontaneous remissions are uncommon and, in most cases, GAD will have been present for many years before it is recognized and treated appropriately.2-4 Patients with GAD are at risk of serious social, occupational, and educational impairment and of greater need for medical treatment.5-10 Comorbidity, especially major depression, is common and complicates treatment.11,12 When GAD coexists with a medical condition, the medical prognosis is worse.2
Evidence suggests that GAD is common in primary health care.8,10,13-16 Several authors suggest that GAD is difficult to identify in primary care.4,8,10,15,17-19 The main explanation is that many of these patients have several somatic symptoms that dominate their concern17-19; they seldom present directly and openly with anxiety complaints.4,17,18 Some experts suggest that patients might fail to discuss anxiety openly with doctors because they fear stigma associated with mental health problems,20 while others might be unable to recognize a link between somatic symptoms and anxiety, or to recognize abnormal levels of anxiety.21
Many questions about why GAD seems hard to diagnose still are unanswered. For example, it remains unclear whether other resources are consulted for anxiety or somatic symptoms along with family doctors; if they are, what types of resources are most consulted? Types of complaints also deserve more attention. Asking these patients openly whether they consider their anxiety to be troublesome might also help explain why GAD would sometimes go unrecognized in family practice.
This exploratory study aimed to examine some health care–seeking behaviours of patients who have positive results for GAD and to document frequency of positive results from GAD screening tests in a sample of patients from community-based primary health care clinics in the Quebec city metropolitan region.
METHOD
A survey using a self-administered assessment package was conducted in four community-based primary health care clinics between May and August 2002. The protocol was approved by Laval University’s ethics committee, and informed consent was obtained from all respondents. Two family doctors served as consultants on the study.
Medical clinics were randomly selected from the telephone directory. First, telephone contact was made to solicit collaboration; then the protocol and instruments were presented. Four clinics (out of 21 contacted) agreed to collaborate. Three distinct parts of the metropolitan area were covered by the recruitment, which was held at different times of the day to maximize sample representativeness.
All patients presenting at the registration counter were invited to participate. The study was presented as a survey on self-perceived health and health care use in the past year. To be included, patients had to be 18 years or older, to be consulting a physician for themselves, and to be able to fill out questionnaires autonomously. Questionnaires were presented in a random order and were completed while patients waited for their appointments.
Measures
Demographic characteristics and health-related behaviours.
Data on demographic characteristics and health-related and health care–seeking behaviours were collected using a survey adapted from a prior study.22 The survey, composed of 25 multiple-choice and open-ended questions, was devised by a team of psychologists and family doctors working in the insomnia and anxiety field. For this study specifically, the protocol was pilot-tested with 10 respondents.
Worry and anxiety.
The self-reported worry and anxiety questionnaire (WAQ)23 is based on DSM-IV diagnostic criteria for GAD. It is composed of six items: a free-recall question concerning worry themes and five items evaluated on 9-point Likert-type scales (0 to 8) covering the degree of lack of control over worries, the associated somatic symptoms, and the extent of interference with daily life. The WAQ has been devised as a first-line screening instrument; it shows good sensitivity (89.5%) and satisfactory specificity and test-retest reliability.23 The scoring algorithm yields positive or negative results, but quantification of severity and interference with functioning is possible.23
Mood.
The widely used Beck depression inventory-II24,25 reliably informs clinicians of the presence and severity of depressed mood. It includes 21 items rated on four-point scales (0 to 3). It shows adequate validity, excellent internal consistency, and excellent temporal stability.26
Sleep.
The seven-item insomnia severity index 27 assesses insomnia according to DSM-IV criteria. This self-report measure shows good internal consistency and appropriate test-retest reliability.28
Statistical analyses
Proportions were compared using chi-square tests; mean comparisons were performed using paired t tests or one-way analysis of variance adjusting for variance inequality when needed; 95% confidence intervals and effect sizes (d) are reported. Logistic regressions were computed to examine predictors of GAD. Differences were considered statistically significant at P < .05. Analyses were performed using SAS release 8.2.
RESULTS
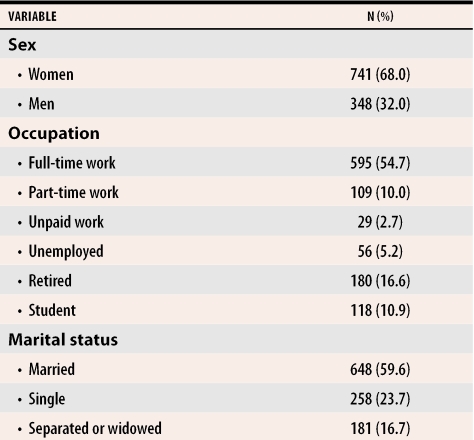
Of the 1878 patients invited, 768 refused to participate (360 patients) or did not meet inclusion criteria (408 patients). The final sample comprised 1110 patients, of which 219 (19.7%) tested positive for GAD on the WAQ. Table 1 shows sample characteristics.
Table 1. Sociodemographic characteristics of the sample.
Mean age of respondents was 42 (SD 15.7) and level of education was 14.7 years (SD 3.2).
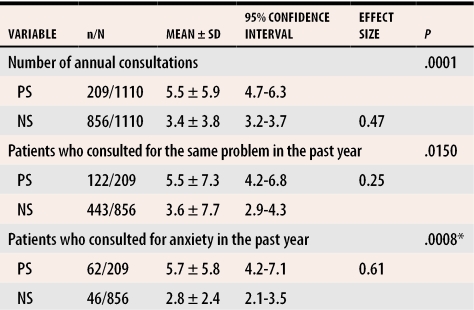
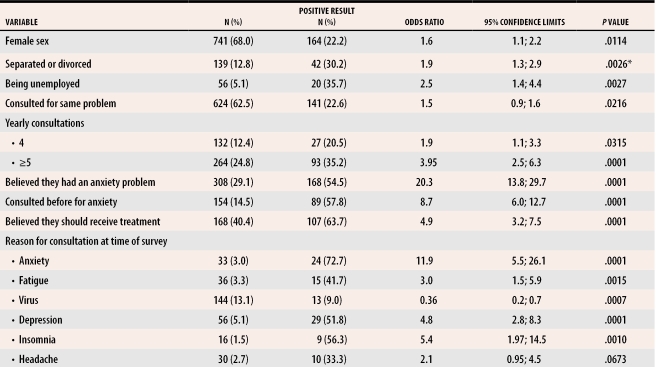
Table 2 shows health care–seeking behaviours of patients with positive results (PS) and negative results (NS) on the screening test, while Table 3 shows logistic regression results predicting PSs.
Table 2.
Health care–seeking behaviours according to positive or negative results of GAD screening test
PS—patients who tested positive on the worry and anxiety questionnaire, NS—patients who tested negative on the worry and anxiety questionnaire. *Adjusted for inequality of the variances.
Table 3.
Predictors of a positive GAD screening result
Demographic variables
A higher proportion of women (22.1% vs 15.5% men) were in the PS group and were 1.6 times more likely to have PSs for GAD. Separated or divorced respondents were nearly twice (odds ratio [OR] = 1.9) and unemployed patients were more than twice (OR = 2.5) as likely to have PSs. No significant differences were observed for age and education level.
Health care–seeking behaviours
Patients with PSs reported consulting physicians significantly more often (P < .0001) than patients with NSs, averaging 5.4 (standard deviation [SD] = 5.9) consultations annually compared with 3.4 (SD = 3.8), respectively. A total of 44.5% in the PS group reported consulting a general practitioner five times or more yearly, compared with 20.0% in the NS group (P < .0001). These “higher health care users” were nearly four times as likely to have positive results.
Patients with PSs reported having consulted significantly more often (P = .01; d = 0.25) in the past year for the same complaint, averaging 5.5 (SD = 7.3) compared with 3.4 (SD = 7.7) consultations among NS patients; this was also a significant predictor of PSs (OR = 1.5).
A total of 42% of PS patients reported having consulted specifically for anxiety in the past year compared with 7.7% of NS patients (P = .0001). Patients with PSs reported an average of 5.6 (SD = 5.8) medical consultations specifically for anxiety compared with 2.8 (SD = 2.4) for the NS group (P = .0008). Among PS patients, 80% believed they had an anxiety problem; they were 20 times more likely to have PSs. Among those, 61.5% believed they should receive treatment for this condition. Patients with PSs, however, did not consult other resources (eg, psychiatrists, physiotherapists, psychologists) for anxiety significantly more often (Table 3).
At the time of the survey, a higher proportion of PS patients reported consulting for anxiety symptoms, fatigue, depression, and sleep difficulties, and a higher proportion reported consulting for headaches; the latter difference did not reach significance (P = .06). A higher proportion of NS patients reported consulting for colds, flu, or symptoms of infection.
Health-related characteristics
More PS patients presented with (self-reported) complaints of feeling depressed and mood-related disorders (which included burnout and exhaustion), sleep difficulties, and gastric problems (which included stomach ulcers, acidity, esophageal reflux, and slow digestion).
Patients with PSs also reported significantly higher (P = .0001; d = 1.5) Beck depression inventory-II scores (M = 20.7; SD = 11.2) than NS patients (M = 8.2; SD = 7.3) and significantly higher (P = .0001; d = 1.3) insomnia severity index scores (M = 13.3, SD = 5.5) than NS patients (M = 6.7, SD = 4.9), indicating more insomnia symptoms.
DISCUSSION
Results of this exploratory study show that PS patients reported consulting family physicians significantly more often than other patients, which is in line with results of larger-scale studies.9-12 This study’s results go further, suggesting that more than five annual consultations were associated with a greater likelihood of having PSs. When multiple consultations are not better explained by patients’ medical status, further investigation into GAD could be warranted. Some reasons for requesting the consultation can also serve as hints. In this sample, PS patients complained more often of feeling depressed and had significantly higher Beck depression inventory-II scores, which could reflect ongoing worries and anxiety29 or comorbidity.30-33 Insomnia symptoms were also significantly higher in the PS group. The correlation of insomnia symptoms and GAD suggests that insomnia sometimes indicates an underlying anxiety disorder.34,35 In all cases, differential diagnosis remains essential. Fatigue, gastric problems, and headaches were also presented more often by PS patients but were not corroborated by any psychometric measure we administered.
A key finding is that most PS patients believed they had an anxiety problem but, despite this, did not report consulting other professionals specifically for anxiety more often than NS patients. This observation has important clinical implications. First, it further supports the hypothesis that symptoms of this disorder are treated mostly in primary care.15,16 Second, it suggests that most of these patients did recognize that at least some of their symptoms were related to anxiety, contrary to the hypothesis that patients fail to recognize such connections.21 Perhaps patients avoid complaining of anxiety openly to treating doctors. Educating patients and their families might help them better recognize anxiety symptoms and help reduce the stigma of mental illness.20 High-yield questions about excessive anxiety and worrying, as part of routine examinations, could also help reduce this fear and guide investigation. In this study, patients who believed they had an anxiety problem were 20 times more likely to have PSs; this could be a useful avenue for further investigation.
Self-reported screening tests could also represent a useful and time-saving way to recognize GAD. As a first-line screening instrument, the WAQ favors sensitivity over specificity, which is one of its goals and strengths because the probability of letting false-negative results escape investigation is minimized. Positive results will nevertheless require confirmation through clinician assessment of differential diagnoses and coexisting conditions.
Limitations
Results of this study must be interpreted with caution. First, the true number of GAD cases was not assessed. In this sample, 19.7% tested positive for GAD. Although we estimate that patients with GAD are numerous in primary health care, we do not have a prevalence estimate. This rate is probably inflated by our screening instrument’s higher sensitivity (over specificity). Preliminary results from another study, however, suggest that WAQ’s false-positive results in most cases identify another anxiety disorder. Second, results are based on patients’ self-reports. Recalling how many times one generally consults a physician might not be an easy task for frequent health care users. The ideal design would be to collect this information directly from medical files.
Further, in a self-selected sample, the choice to fill out a questionnaire introduces a selection bias. This bias is almost always present in this type of research but might be attenuated by various recruitment procedures. For example, it would be interesting to compare acceptance rates if solicitation came directly from medical teams in settings other than waiting rooms. In our sample, more women than men agreed to fill out the survey. Even if this difference were controlled for in the analyses, it also limits generalizability. The observation that women volunteer more often for surveys has been widely discussed. This factor could be bypassed if solicitation came from other sources.
Finally, although more PS patients reported consulting physicians specifically for anxiety, most (58%) reported not having done so in the past year. What is unclear from this study is whether they were already receiving treatment for anxiety, failed to mention anxiety, or did not consult for anxiety at all. Again, corroboration of these results with chart reviews and physicians’ clinical observations would help to answer this question.
Conclusion
This study represents an attempt to better understand why GAD is considered difficult to recognize in primary health care.4,8,17-19,36 Studies likely to further our comprehension might examine how frequently GAD is indeed diagnosed, the characteristics of patients with GAD, and how GAD is managed in primary care. Implementing different GAD education strategies and assessing their effect on diagnosis and treatment are also warranted.
This study sought to document some health care–seeking behaviours of patients with GAD in order to better understand why GAD is considered difficult to recognize in primary health care. Results showed that patients with GAD reported consulting family physicians significantly more often than other patients, but did not report consulting other resources more often, suggesting that patients with GAD might mostly seek treatment from primary care physicians. Most of these patients believed they had an anxiety problem, thus invalidating the hypothesis that these patients fail to acknowledge that their anxiety level is troublesome. Educating patients and their families might boost recognition of GAD and reduce the stigma associated with mental illness.
Acknowledgments
Dr Bélanger thanks statistician François Harel for supervising her data analysis.
Biography
Dr Bélanger is a postdoctoral researcher, Dr Ladouceur is a Professor, and Dr Morin is a Professor, all at École de Psychologie and the Centre de Recherche Robert-Giffard at Laval University in Quebec city, Que.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 2.Ballenger JC, Davidson JR, Lecrubier Y, Nutt DJ, Borkovec TD, Rickels K, et al. Consensus statement on generalized anxiety disorder from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry. pp. 53–58. [PubMed]
- 3.Keller MB. The long-term clinical course of generalized anxiety disorder. J Clin Psychiatry. pp. 11–16. [PubMed]
- 4.Bradwejn J, Berner M, Shaw B. Malade d’inquiétude. Montréal, Qué: Grosvenor Inc; 1992. [Google Scholar]
- 5.DuPont RL, Rice DP, Miller LS, Shiraki SS, Rowland CR, Harwood HJ. Economic costs of anxiety disorders. Anxiety. pp. 167–172. [DOI] [PubMed]
- 6.Lydiard RB. An overview of generalized anxiety disorder: disease state—appropriate therapy. Clin Ther. pp. 3–19. [DOI] [PubMed]
- 7.Roy-Byrne PP. Generalized anxiety and mixed anxiety-depression: association with disability and health care utilization. J Clin Psychiatry. pp. 86–91. [PubMed]
- 8.Weiller E, Bisserbe JC, Maier W, Lecrubier Y. Prevalence and recognition of anxiety syndromes in five European primary care settings. A report from the WHO study on Psychological Problems in General Health Care. Br J Psychiatry Suppl. pp. 18–23. [PubMed]
- 9.Pelissolo A, Andre C, Chignon JM, Dutoit D, Martin P, Richard-Berthe C, et al. [Anxiety disorders in private practice psychiatric out-patients: prevalence, comorbidity and burden (Delta Study)]. Encephale. pp. 510–519. [PubMed]
- 10.Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depress Anxiety. pp. 162–171. [DOI] [PubMed]
- 11.Gaynes BN, Magruder KM, Burns BJ, Wagner HR, Yarnall KS, Broadhead WE. Does a coexisting anxiety disorder predict persistence of depressive illness in primary care patients with major depression? Gen Hosp Psychiatry. pp. 158–167. [DOI] [PubMed]
- 12.Schonfeld WH, Verboncoeur CJ, Fifer SK, Lipschutz RC, Lubeck DP, Buesching DP. The functioning and well-being of patients with unrecognized anxiety disorders and major depressive disorder. J Affect Disord. pp. 105–119. [DOI] [PubMed]
- 13.Wittchen HU, Zhao S, Kessler RC, Eaton WW. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. pp. 355–364. [DOI] [PubMed]
- 14.Maier W, Gänsicke M, Freyberger HJ, Linz M, Heun R, Lecrubier Y. Generalized anxiety disorder (ICD-10) in primary care from a cross-cultural perspective: a valid diagnostic entity? Acta Psychiatr Scand. pp. 29–36. [DOI] [PubMed]
- 15.Wittchen HU, Kessler RC, Beesdo K, Krause P, Höfler M, Hoyer J. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry. pp. 24–34. [PubMed]
- 16.Ansseau M, Dierick M, Buntinkx F, Cnockaert P, De Smedt J, Van Den Haute M, et al. High prevalence of mental disorders in primary care. J Affect Disord. pp. 49–55. [DOI] [PubMed]
- 17.Wittchen HU, Hoyer J. Generalized anxiety disorder: nature and course. J Clin Psychiatry. pp. 15–19. [PubMed]
- 18.Ustünd TB, Sartorius N. Mental illness in general health care: an international study. Chichester, UK: John Wiley & Sons Ltd; 1996. [Google Scholar]
- 19.Culpepper L. Generalized anxiety disorder in primary care: emerging issues in management and treatment. J Clin Psychiatry. pp. 35–42. [PubMed]
- 20.Department of Health and Human Services. Mental health: a report of the Surgeon General. Rockville, Md: Department of Health and Human Services, US Public Health Services; 1999. [Google Scholar]
- 21.Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–569. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- 22.Blais FC, Morin CM, Boisclair A, Grenier V, Guay B. L’insomnie. Prévalence et traitement chez les patients consultant en médecine générale. Can Fam Physician. 2001;47:759–767. [PMC free article] [PubMed] [Google Scholar]
- 23.Dugas MJ, Freeston MH, Provencher MD, Lachance S, Ladouceur R, Gosselin P. Le Questionnaire sur l’inquiétude et l’anxiété. Validation dans des echantillons non cliniques et cliniques. J Ther Comport Cogn. 2001;11:31–36. [Google Scholar]
- 24.Beck AT, Steer RA, Brown GK. Beck depression inventory [manual]. 2nd ed. San Antonio, Tex: The Psychological Corporation; 1996. [Google Scholar]
- 25.Beck AT, Rush JA, Shaw BF, Emery GK. Cognitive therapy of depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- 26.Dozois DJA, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck depression inventory-II. Psychol Assess. pp. 83–89.
- 27.Morin CM. Insomnia. Psychological assessment and management. Treatment manual for practitioners. New York, NY: Guilford Press; 1993. [Google Scholar]
- 28.Blais FC, Gendron L, Mimeault V, Morin CM. Évaluation de l’insomnie: validation de trois questionnaires. Encephale. pp. 447–453. [PubMed]
- 29.Dugas MJ, Gagnon F, Ladouceur R, Freeston MH. Generalized anxiety disorder: a preliminary test of a conceptual model. Behav Res Ther. pp. 215–226. [DOI] [PubMed]
- 30.Rogers MP, Warshaw MG, Goisman RM, Goldenberg I, Rodriguez-Villa F, Mallya G, et al. Comparing primary and secondary generalized anxiety disorder in a long-term naturalistic study of anxiety disorders. Depress Anxiety. pp. 1–7. [PubMed]
- 31.Yonker KA, Warshaw MG, Massion OA, Keller MB. Phenomenology and course of generalised anxiety disorder. Br J Psychiatry. 1996;168:308–313. doi: 10.1192/bjp.168.3.308. [DOI] [PubMed] [Google Scholar]
- 32.Rickels K, Schweizer E. The clinical presentation of generalized anxiety in primary-care settings: practical concepts of classification and management. J Clin Psychiatry. 1997;58(Suppl 11):4–10. [PubMed] [Google Scholar]
- 33.Judd LL, Kessler RC, Paulus MP, Zeller PV, Wittchen HU, Kunovac JL. Comorbidity as a fundamental feature of generalized anxiety disorders: results from the National Comorbidity Study (NCS). Acta Psychiatr Scand Suppl. pp. 6–11. [DOI] [PubMed]
- 34.Bélanger L, Morin CM, Langlois F, Ladouceur R. Insomnia and generalized anxiety disorder: effects of cognitive behavior therapy for GAD on insomnia symptoms. J Anxiety Disord. 2004;18:561–571. doi: 10.1016/S0887-6185(03)00031-8. [DOI] [PubMed] [Google Scholar]
- 35.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment: prevalence and correlates. Arch Gen Psychiatry. pp. 225–232. [DOI] [PubMed]
- 36.Kessler RC, Wittchen HU. Patterns and correlates of generalized anxiety disorders in community samples. J Clin Psychiatry. 2002;63(Suppl 8):4–10. [PubMed] [Google Scholar]