Abstract
As the Personal Digital Assistant (PDA) user population continues to expand, there is a need to design more useful devices and applications to facilitate the utilization of PDAs. We conducted a structured interview study to examine PDA usage and non-usage patterns among physicians. The purpose of this descriptive study was to identify the barriers that impede physicians in their PDA use. A data collection tool was developed to record: 1) how physicians use their PDAs, 2) functions and applications used, 3) functions and applications not used, 4) reasons and examples of why physicians don’t use PDAs for those functions, and 5) the recall of specific incidents of PDA usage using Critical Incident Technique (CIT). Interview data were transcribed and analyzed. Study findings and how those barriers can be addressed are discussed.
INTRODUCTION
Sparked by enthusiasm over these types of devices, more than 20 million personal digital assistants (PDAs) have been sold worldwide over last 5 years. These pocket-sized digital companions can store thousands of appointments, contacts, notes, as well as other personal and professional data. Worldwide shipments of PDAs totaled up to 12.1 million units in 2002, according to Dataquest Inc. Currently, most people purchase PDAs to use at work and connect them to applications on desktop computers.1–2
In Healthcare, approximately 26% of U.S. physicians used PDAs in 2001, and it has been documented that approximately 85% of physicians would consider carrying a PDA.3–4 These data suggest that PDAs have become an integral component of many clinicians’ daily routines. PDAs may provide tremendous benefits in assisting physicians and other healthcare providers to access, manage, and share critical medical information at the point of care.
Many efforts have been reported in the literature on physicians’ PDA usage patterns. For example, some of these studies showed that physicians used PDAs to manage personal information using a datebook or address book, to access drug references, and to record data. 5–7 However, no attempts have been made to examine the non-usage patterns. It would be valuable and beneficial to understand the barriers to full utilization of PDAs, so that technical, educational, and organizational or institutional solutions may be proposed to address those barriers.
The goal of our study was to investigate the physicians’ non-usage patterns by conducting a structured interview using the Critical Incident Technique (CIT) with physicians to identify potential barriers to PDA usage in various acute clinical settings.
SETTING & SUBJECTS
Twenty physicians from a major university medical center were recruited and interviewed face to face. Seven were attending physicians, twelve were residents, and one was a fellow. Fifteen of the subjects were males and five were females. The settings where the subjects worked included trauma, general surgery, emergency department, and neonatal intensive care. The average length of PDA ownership was 1.17 years. Seven of the physicians were issued a PDA whereas thirteen purchased the devices themselves. All PDAs run the Palm operating system.
METHOD
Tool design
A data collection tool using the principles of CIT was developed to interview the subjects. Table 1 provides CIT interview questions.
Table 1.
CIT Questions.
| Critical Incident Questions |
|---|
|
Flanagan developed CIT in the early 1950s; the technique was used to improve the selection of pilots and pilot training programs.8 According to Flanagan, the CIT “outlines procedures for collecting observed incidents having special significance and meeting systematically defined criteria.”9 The incidents are defined as any “observable human activity that is sufficiently complete in itself to permit inferences and predictions to be made about the person performing the act.”9 To be critical, “an incident must occur in a situation where the purpose or intent of the act seems fairly clear to the observer and where its consequences are sufficiently definite to leave little doubt concerning its effects.”9
CIT has been found useful to study various research questions in many different types of settings.10–11 In healthcare, for example, Kent et al. used CIT to investigate patient reactions to met and unmet psychological needs.9 Gilbart et al. also reported using CIT to develop and assess a rating form for selection of surgical residents based on criteria for successful performance.11
We use the CIT to explore PDA non-usage patterns and barriers faced by physicians. Data collection in CIT-based studies has been performed using interviews.8 We developed CIT-based questions based on the literature and our preliminary study.12 In addition to the CIT questions, other specific usage pattern questions were included in our data collection tool for use during the interview process.
Data Collection and Analysis
One nurse (JKL, who was in a Masters’ Degree program in Nursing) under the guidance of a senior researcher (YX), conducted the interviews. The interviewer and a nursing PhD student (YCL) were then trained by the senior researcher to analyze the data. The interviewer was blinded to priori hypotheses in order to minimize the interviewer bias. The PhD student, on the other hand, had reviewed related literature and participated in the development of research hypotheses. The interviews were tape recorded and transcribed for analysis. Data recorded from the data collection sheets were also coded and analyzed.
RESULTS
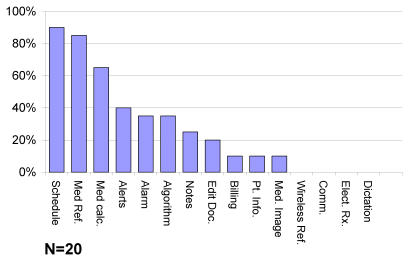
The healthcare PDA functions identified by literature are scheduling, medical references, medication dose calculations, alerts for tasks, alarms clock, reference algorithms, notes, documents editing, billing, access or input of patient information, medical images, wireless medical information referencing, email or instant messaging communication, and electronic prescription. Figure 1 shows the percentages of the studied 20 PDA owners who reported use of specific functions. For example, among the functions identified from the literature, 90% of physicians in our study used PDAs for scheduling, 85 % of them used PDAs for medical reference, and 65% used PDAs for medical calculation.
Figure 1.
Percentages of PDA owners who reported use of specific functions.
We identified four types of barriers from the analysis: 1) organizational barriers (30% of subjects), 2) usability barriers (95%), 3) inadequate technology support or access barriers (85%), and 4) lack of need or motivation (100%).
Organizational barriers include lack of integration and institutional supports, and legal issues. For example, if institutions do not have integrated information systems that allow for real-time access to hospital databases, physicians cannot use their PDAs to access patient data. On the other hand, if the institutions have all the support and technology available, physicians are more likely to use it.
Usability barriers include usability issues such as screen size, hand writing recognition problems, data entry mechanism, short battery life, perceived delicacy of the device, and additional accessories needed to perform functions. One physician indicated that he did not like to go through several screens to pull all the necessary information (such as medication and lab value) together.
Inadequate technology support and access barriers include unavailability of technology support, expired warranty, and unavailable features or applications. For example, some physicians cannot address malfunctions on their PDAs because of inadequate or inaccessible tech support; hence, they cannot use the PDAs or specific applications.
Lack of need or motivation include applications or functions perceived as unnecessary and too general for practice, information integrated into profession, dissatisfaction with previous experience, preference for manual method, function performed by other personnel, and function performed with other hardware or methods.
Those barriers can interact with one another and either enhance or diminish the impact of one another. For instance, a usability barrier could discourage physicians from using PDAs (reduced motivation). On the other hand, if physicians have unlimited institutional or technical support, their motivation might increase. Table 2 provides representative quotes from interviews.
Table 2.
Representative Quotes from Physicians
| Barrier Type | Representative Quotes from physician respondents |
|---|---|
| Organizational Barriers | |
| Lack of Integration and Institutional Support | “It would make a lot of sense to have that capability to have a program that allows you to generate notes, to write a prescription, and to give you alerts and all those kinds of things, that would be useful, but this institution doesn’t lend itself to that kind of concept at least where I work.” – Attending Physician |
| Legal Issues | “On top of the fact that the hospital lawyers have made it almost impossible to drag a note from yesterday to today and start fresh with stuff that has been entered yesterday.” –Attending Physician |
| Usability Barriers | |
| Usability Issues | “There were too many screens and you couldn’t see everything at one time.” –1st Year Resident; “I wish it was smaller, lighter, things like that.” –Attending Physician |
| Not User Friendly/Lack of User Knowledge | “If I figured out how to do it, I might.” –2nd Year Resident |
| Battery Life Issue | “I’d be afraid of chewing up the battery.” –Attending Physician |
| Perceived Delicacy of PDAs | “…a PDA becomes just a burden, keeping track of it, not sitting on it, things like that becomes more of a hassle than the benefit I would get from using it.” –3rd year Resident |
| Additional Accessories Needed | “I guess I could get a mobile charger if I wanna pay 30 bucks but I’m too cheap, so...” –2nd year Resident |
| Inadequate Technology/Support/Access Barriers | |
| Inadequate/Unavailable tech support or expired warranty | “…called whoever the “tech support” is and still couldn’t get it to work.” –3rd Year Resident |
| Unavailable features or applications on PDA | “Not loaded. If it was loaded, I’d use it.” (Diagnostic Algorithms) – Attending Physician |
| Lack of Need/Motivation | |
| Application or function perceived as unnecessary | “Because I remember all my appointments if I look at them in the beginning of the day. If I look at my PDA and it says I have a meeting at 2 o’clock, I don’t need to be reminded at 1:45 (calendar alerts).” – Attending Physician |
| Information integrated into profession | “And so I rarely get the answers I need from any of these things (electronic textbooks) and I use them infrequently because of that.” – Attending Physician |
| Application or function perceived as too general for practice | “If there had been pull down menus that were appropriate for the cases that I was doing, that would have been easier. But the pull down menus didn’t have the cases I was performing. Not specific enough for what I needed it to be.” –Chief Resident |
| Dissatisfied with previous experience | “I was writing down my information for the operative cases and it was just too cumbersome a program to use in an efficient manner. So I quickly abandoned it and went back to writing things down in a conventional manner.” –Chief Resident |
| Manual method preferred | “I’d rather just go up to a book and open it or go into the internet and the computers and read off of that.” –Intern. |
| Function performed by other personnel | “I don’t do billing. Attendings do all the billing.” –2nd Year Resident |
| Function performed with other hardware/methods | “We use this (pointing to PC tablet). ” –Attending Physician |
DISCUSSION
We have identified a number of barriers to using PDAs (lack of integration and institutional support, screen size, graffiti, battery life, inadequate technical support, and perceived delicacy of PDAs). Some of these barriers were consistent with the literature 13–17 However, we found when physicians frequently use a particular PDA application, it is well integrated into the daily workflow. Physicians also tend to use a particular application when the application is easy to access and user-friendly. For example, physicians often use ePocrates from their PDAs to obtain drug information, because they feel that the manual alternative (e.g. go to library and pull out medical reference books) interferes with an efficient workflow. In addition, it is a free application; many of their colleagues are using it.
In contrast, if the functions or applications required additional effort (such as debugging), cost (purchasing accessories or applications), or time (e.g. spending a lot of time to look for or learn the function or application), physicians are less likely to use them.
It is also interesting to note that physicians tended to opt out of an application or PDA function if it did not prove effective after the first attempt. This might result from an individual’s characteristics or the nature of the physician’s busy practice. They usually do not want to waste their scarce time on some nuisances like trouble shooting their PDAs. However, further research is necessary to examine the correlation between negative prior experiences and the decision of not using an application or function.
It is worthy to mention one extreme case in our study: a physician who was issued a PDA but never used it. When asked why his PDA was still in the box, he indicated that there was no incentive for using a PDA since he had easier access to information from unit computers and a pocket pharmacopoeia. From this case, we could see that for this particular physician, lack of need or motivation seems to be the strongest predictor of use or non-use of PDA and functions. However, whether this result can be generalized to other physicians is unknown. Further studies are recommended to investigate the relationship between the motivation/need and non-use patterns.
This study has several limitations. First, only one researcher conducted the interviews; however, the potential for bias was minimized because all researchers had input into the design of the interview questions and two researchers analyzed the data. However, one analyst was not blinded to the priori hypotheses, which could introduce an analysis bias. Second, small sample size and use of convenience samples limited generalization of the findings. Last, other non-usage patterns or factors might be overlooked due to the study design. However, we will address these issues in our future studies.
CONCLUSION
Physicians have regarded PDAs as portable, relatively inexpensive devices for point of care clinical reference and information management. We investigated the barriers that influence physicians’ usage patterns and behaviors. The findings can serve as a user modeling profile for designing hardware, software, and for institutionally supported implementation of a facility-wide mobile computing system. For our next phases of study, we would like to further examine the relationships between the four types of barriers and non-use of PDAs to determine which is the best predictor of PDA non-usage. Further research is recommended to look at the impact of PDA technology on clinical practice.
Acknowledgments
We would like to acknowledge the patience and cooperation of the physicians interviewed for this study and Jake Seagull, PhD for his assistance. This material is based upon work supported by the National Science Foundation (NSF) under Grant Nos. ITR-0081868 and IIS-0121570. Any opinions, findings and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF. Email contact: yxiao@umaryland.edu.
REFERENCES
- 1.The Mercury News. PDA sales slump in 2002 on slack corporate demand. The Mercury News, Jan 27, 2003. Retrieved March 3, 2003 from http://www.siliconvalley.com/mld/siliconvalley/news/editorial/5043972.htm Accessed Feb 24, 2003.
- 2.Tischelle G. PDA Sales Remain Strong. InformationWeek, Feb 7, 2002. Access March 3, 2003 from http://www.informationweek.com/story/IWK20020207S0015
- 3.Criswell DF, Parchman ML. Handheld computer use in U.S. family practice residency programs. Journal of American Informatics Association. 2002;9:80–86. doi: 10.1136/jamia.2002.0090080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ebell MH, Gaspar DL, Khurana S. Family physicians’ preferences for computerized decision support hardware and software. Journal of Family Practice. 1997;45:2:137–141. [PubMed] [Google Scholar]
- 5.d’Hemecourt P. Assistance in the palm of your hand. Healthcare Informatics. 2001:102–103. [PubMed] [Google Scholar]
- 6.Survey shows PDAs are just what the doctor ordered. Retrieved March 3, 2003 from http://www.avantgo.com/news/press/press_archive/2002/release04_11_02.html
- 7.Digital Library. The trends Retrieved March 3, 2003 from http://www.lib.hku.hk/denlib/sep2002/trend.html
- 8.Ölvingson C, Hallberg N, Timpka T, Greenes RA. Using the critical incident technique to define a minimal data set for requirements elicitation in public health. International Journal of Medical Informatics. 2002;68:165–174. doi: 10.1016/s1386-5056(02)00074-6. [DOI] [PubMed] [Google Scholar]
- 9.Flanagan JC. The critical incident technique. Psychological Bulletin. 1954;51:4:327. doi: 10.1037/h0061470. [DOI] [PubMed] [Google Scholar]
- 10.Kent G, Wills G, Faulkner A, Parry G, Whipp M, Coleman R. Patient reactions to met and unmet psychological need: A critical incident analysis. Patient Education And Counseling. 1996;28:187–190. doi: 10.1016/0738-3991(96)00899-3. [DOI] [PubMed] [Google Scholar]
- 11.Gilbart MK, Cusimano MD, Regehr G. Evaluating surgical resident selection procedures. The American Journal of Surgery. 2001;181:221–225. doi: 10.1016/s0002-9610(01)00550-5. [DOI] [PubMed] [Google Scholar]
- 12.Lu, YC, Xiao, Y, Sears, A & Jacko, J. An observational and interview study on personal digital assistant (PDA) uses by clinicians in different contexts. Proceeding HCI International Conference, 2003 (in press).
- 13.Kiél J M, Goldblum O M. Using personal digital assistant to enhance outcomes. Journal of Healthcare Information Management. 2001;15(3):237–250. [PubMed] [Google Scholar]
- 14.Brody J A, Camamo J M, Maloney M E. Implementing a personal digital assistant to document clinical interventions by pharmacy residents. American Journal of Health-System Pharmacy. 2001;58(16):1520–1522. doi: 10.1093/ajhp/58.16.1520. [DOI] [PubMed] [Google Scholar]
- 15.Ammenwerth E, Buchauer A, Bludau B, Haux R. Mobile information and communication tools in the hospital. International Journal of Medical Informatics. 2000;57:21–40. doi: 10.1016/s1386-5056(99)00056-8. [DOI] [PubMed] [Google Scholar]
- 16.Kelly J. Going wireless. Hospitals & Health Networks 2002; 65–68. [PubMed]
- 17.Garvin R, Otto F, McRae D. Using handheld computers to document family practice resident procedure experience. Family Medicine. 2000;32(2):115–118. [PubMed] [Google Scholar]