Abstract
We developed the Home Automated Telemanagement (HAT) system for patients on oral anticoagulation therapy. It consists of a home unit, HAT server, and clinician unit. Patients at home use a palmtop or a laptop connected with a prothrombin time (PT) monitor. Each HAT session consists of self-testing, feedback, and educational components. The symptom data and PT/INR from patient homes are automatically sent to the HAT server and analyzed by the system. Patients who were seen in the Anticoagulation Clinic (N=29) were asked to use HAT in a laboratory setting. Semi-structured, indepth interviews were used for the evaluation of HAT acceptance. 93% claimed that they would use such a tool at home and would advise other patients to use HAT for self-management and disease-specific education. Twelve patients used HAT at home for eight weeks. Compared to baseline, patients completing the home study showed statistically significant improvement in disease-specific quality of life dimensions of general satisfaction, self-efficacy, daily hassles, and distress. The Client Satisfaction Questionnaire demonstrated significant improvement in patient satisfaction with the treatment process. Our results demonstrated high acceptance of the HAT system by patients receiving long term anticoagulation therapy regardless of their previous computer experience or socioeconomic background.
INTRODUCTION
A number of studies of patient self-testing (PST) or patient self-management (PSM) with point-of-care (POC) devices have recently indicated the potential for improved outcomes. 1,2 Successful patient self-management, however, requires a multidisciplinary approach that includes not only regular patient assessment, but also disease-specific education, control of medication adherence, implementation of health behavior change models, and social support both for patients and caregivers.3,4 Existing systems for computer-assisted anticoagulation management do not provide this multidisciplinary patient support and do not address treatment compliance issues. We developed the Home Automated Telemanagement (HAT) system to provide multidisciplinary support for patient self-management and to enhance patient compliance with treatment regimens. This system is currently being used to evaluate the efficacy of home telemanagement of patients with asthma and chronic obstructive pulmonary disease where a high level of acceptance of the system has already been shown in these conditions5–7.
The aims of this project were (1) refinement of the HAT system to provide a multidisciplinary model of anticoagulation therapy, and (2) evaluation of patient acceptance and the feasibility of the HAT system in patients on anticoagulation therapy in a prospective pilot study.
METHODS
Design of the Anticoagulation HAT system
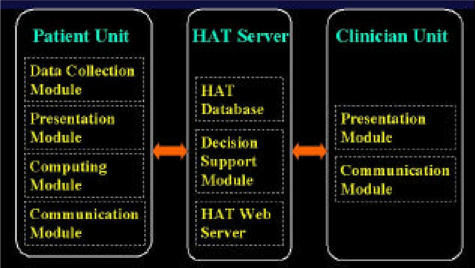
We used the protocol recommended by the User-Centered Design Workshop at the Participatory Design Conference (PDC) in Seattle (November 1998)9. According to this workshop, our design process was grounded on observations of the users’ practices in the real world, and the users became involved in the design process not only at the beginning and/or at the end, but throughout the development period. The existing Home Automated Telemanagement (HAT) system served as a prototype for development of a comprehensive multi-component support for anticoagulation self-care. The HAT system consists of home units (HU), a HAT server, and clinician units (Fig. 1). The home unit, used by the patient at home, consists of a computing device (palmtop, laptop or desktop) connected with a disease-specific sensor. The HU sends patient data to the HAT server. Any Web-enabled device can serve as a clinician unit to review patient results. Patients report their symptoms, medication use, and other self-care information using a HU. Immediately thereafter, the HU sends this information through a landline or wireless connection to the HAT information system. The HAT System is able to automatically monitor patient compliance and analyze self-testing results according to current practice guidelines in real-time. The system also assists patients in carrying out their individual treatment plans. In instances of patient non-compliance with self-testing, medication non-adherence, or failure to follow the individual treatment plan, the system gives feedback to the patient to motivate better compliance, and notifies the patient’s physician and/or nurse. The HAT system provides patients with self-paced interactive multimedia education regarding major aspects of anticoagulation therapy. It can be tailored to patient specific needs and utilizes the main concepts of social cognitive theory. The adaptive algorithm for patient-tailored education has been described previously8.
Figure 1.
Design of the Home Automated Telemanagement (HAT) System
Evaluation of the Anticoagulation HAT system
This study was conducted at Boston Medical Center (BMC) which serves a large number of low-income, inner-city patients. To address issues related to this patient population, we conducted a two-stage assessment of patient acceptance and feasibility of the program.
During the first stage we assessed user acceptance of the HAT interfaces in a laboratory setting. Patients were recruited from the hospital Anticoagulation Clinic, and were asked to use the program and to provide feedback regarding usability of the system and other concerns. The review of HAT components conformed with the principles of usability testing described by Nielsen10. During this stage, each patient completed study forms, was trained to use HAT, used the program for sufficient time to test all major components, completed an attitudinal survey, and underwent a semi-structured qualitative interview aimed to elicit patient attitudes toward HAT and its specific components. The results of the laboratory testing were used to make necessary changes in the system before commencement of evaluation in patient homes.
During the second stage of HAT evaluation patients on oral anticoagulation were recruited to use the system at home. We made every possible effort to ensure socio-demographic diversity of the patients as related to ethnicity, gender, age, income and education. The subjects enrolled in the laboratory pre-trial did not participate in the home trial. To test the system intensively, patients were asked to use the system once a week for eight weeks. The patients completed a disease-specific quality of life questionnaire (QOL)3 and a Client Satisfaction Questionnaire (CSQ-8)11 at the beginning of the study and at the end of the eight-week period. Using the attitudinal survey and semi-structured qualitative interview administered at the end of the follow-up period we identified patient acceptance and potential concerns with specific HAT components.
RESULTS
HAT Redesign
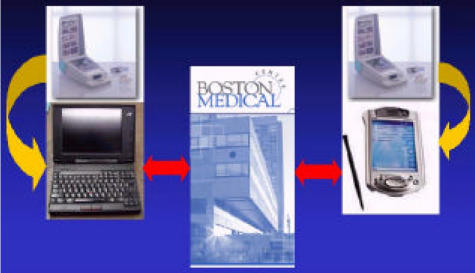
The Home Automated Telemanagement system was successfully implemented and pilot tested at Boston Medical Center (BMC). The system provides automatic capture of patient self-reported parameters (symptoms and medication use) and objective parameters (INR, PT) to evaluate the activity of anticoagulation and to adjust patient therapy. The Protime Microgualation system (International Technidyne Corp., Edison, N.J.) is used as the home blood coagulation monitor. The PT/INR measurements are automatically downloaded into computer memory via a serial port for further interpretation and transmission to BMC (Fig. 2).
Figure 2.
Anticoagulation HAT implemented at Boston Medical Center
Patients can review their results immediately and receive interpretation, counseling, and disease-specific education. The Home Unit allows patients to review their treatment progress (symptoms and PT-INR trends), obtain current warfarin dosage, and receive information about anticoagulation therapy from a knowledge repository implemented in the form of FAQ (frequently asked questions). During the telecommunication sessions, patients receive tailored messages aimed to facilitate their compliance with an individualized treatment plan and to improve patient self-efficacy. When an anticoagulant dose adjustment is updated by hospital staff in response to a patient INR, the new dose calendar is automatically downloaded to the Home Unit. The HAT system can automatically generate alerts each time a patient does not perform self-testing on schedule, does not take medications as prescribed, or does not follow their personal treatment plan. Alerts are checked daily by a nurse case manager. Patients for whom alerts are generated are contacted by the nurse by phone to address clinical issues. The HAT system can generate automatic telephone calls to remind patients about self-testing. All system settings are individualized for each particular patient and can be adjusted by a clinician at the HAT web site. The alerts which cannot be resolved by the HAT nurse are forwarded to patient physicians. The patient physicians receive monthly reports on their patients progress and can access patient self-testing results at any time via the HAT web site.
Laboratory HAT pre-testing
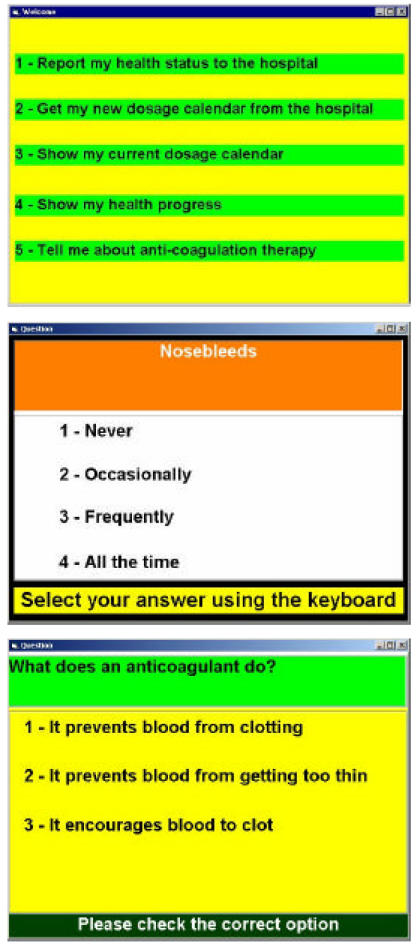
Thirty-one patients were invited to use HAT and 29 patients agreed. Patient age ranged from 34 to 81 years. Just over half of the patients (59%) had no computer experience. All patients were enthusiastic in using HAT. They demonstrated a high level of acceptance of user interface including multimedia content and text font, and 90% stated they did not have difficulties in using HAT. The majority of patients (93%) claimed that they would use such a tool at home and would advise other patients to use HAT for self-management and disease-specific education. In the open-ended section of the interview, patients named the following reasons for high utility of the HAT system: opportunity to save time by reducing number of visits to the Anticoagulation Clinic, knowledge that self-testing results are reviewed by professional staff in a timely manner, and the possibility of having mo re comprehensive disease management. For each HAT component, however, problems in the following areas were identified: (1) content (clarity of messages generated by the system), (2) interface (ease of operation), (3) process (relevance of the component for the user, frequency of use, efficiency of training, etc.). The following recommendations, based on patient feedback, have been introduced to the HAT user interface to improve patient acceptance (Figure 3): text/background contrast, color-coded content, small number of navigation buttons, increased size of navigation buttons, clearer graphics for menu options, large fonts, simple language, friendly encouraging messages, minimizing amount of information per screen (dividing large messages between several screens), patient-tailored navigation tools.
Figure 3.
HAT Home Unit interface
Pilot testing of Anticoagulation HAT in patients’ homes
After refining the HAT system, 14 patients receiving oral anticoagulants were recruited to test the system at their homes. Two patients withdrew and 12 patients completed the study. The following dimensions of QOL resulted in a statistically significant improvement (P<0.05) after eight weeks of using HAT (scores shown at baseline and at the end of follow-up): general satisfaction (2.63, 4.73), self-efficacy (4.49, 5.60), daily hassles (2.40, 1.81), distress (3.15, 2.49). The Client Satisfaction Questionnaire (CSQ-8) scores demonstrated significant improvement (P<0.05) in patient satisfaction with the treatment process (the average score increased from 23.1 to 27.8). In the attitudinal survey 90% of patients expressed their interest in using the HAT system in the future.
DISCUSSION
Chronic oral anticoagulant therapy is the principal means of preventing de novo or secondary recurrence of thromboembolism in patients who are at risk, such as those with atrial fibrillation, prosthetic mechanical heart valves, deep venous thrombosis or pulmonary embolism. There are currently over 2 million individuals on oral anticoagulants in the United States alone, and warfarin sodium is the 15th most prescribed medication in the US based on recent statistics. Oral anticoagulation is also associated with a high rate of adverse events (major hemorrhage), and therapy requires expert dose management to reduce this rate12. Anticoagulation clinics have been developed specifically to address the problems associated with oral anticoagulation, but even with these focused programs, complication rates are still problematic13. With the advent of point-of-care prothrombin time testing, many patients are now able to monitor their own therapy at home, and for selected patients, even adjust their own dose. Such therapy has been shown to improve time-in-therapeutic range for the PT/INR and to reduce adverse events14. However, patient self-monitoring requires patient training and counseling with ongoing education and support to improve compliance and optimize outcomes. Systems currently in place to facilitate patient home monitoring are designed to simply convey the results of an INR test and the recommendations for dose management. No systems are available to provide patient support and education with the goal of enhancing compliance to anticoagulation therapy and improving outcomes. The Anticoagulation HAT is such a program.
In this study we assessed the feasibility of HAT user interfaces and the ability of patients on anticoagulation therapy to adequately process HAT content and control the HAT home unit unassisted. Low socioeconomic status, lack of computer skills, and older age is usually perceived as a barrier towards successful implementation of computer-assisted patient self-care, but this was not the case in our experience. Subsequent analysis of qualitative interviews in a subgroup of patients age 65 and older with no previous computer experience (N=7) identified two groups of factors affecting these patients’ acceptance of the HAT interface: psychological and physical. Older subjects were generally found to be more pragmatic than younger subjects in terms of using new technology. Explaining to older patients how they can benefit from using computer-assisted self-care improved their attitude towards the system. In many older patients acceptance of the HAT system depended on whether we were able to eliminate initial fear of new technology. As soon as the elderly users passed the threshold of being novice, their learning curve and acceptance of the media were not different from other user groups. Other obstacles to successful use of computer interfaces were related to limitations in mobility, vision and cognition. These obstacles could be alleviated by introduction of changes in the user interface accommodating for the user physical limitation (such as use of keyboard instead of mouse, special formatting of text, etc). Based on preferences expressed by the patients we developed different HAT interfaces implementing the same content but tailored to the patients with different preferences: mouse-, keyboard-, and voice-driven interfaces for laptops/desktops and stylus-driven interface for pocketPC. We believe that providing patients with a possibility to choose a user interface tailored to their needs has a potential to significantly facilitate overall acceptance of computer-assisted self-care.
CONCLUSIONS
Our results demonstrated high acceptance of the Home Automated Telemanagement system for patients receiving long term anticoagulation therapy regardless of their previous computer experience or socioeconomic background. Further studies are required to establish the clinical impact and cost-effectiveness of the HAT system in this population.
Acknowledgments
This project was funded in part by an equipment grant from International Technidyne Corp., Edison, N.J.
REFERENCES
- 1.Ansell J, Patel N, Ostrovsky D, Nozzolillo E, Peterson AM, Fish L. Long-term patient self-management of oral anticoagulation. Arch Intern Med. 1995;155:2185–2189. [PubMed] [Google Scholar]
- 2.Koertke H, Minami K, Bairaktaris A, Wagner O, Koerfer R. INR self-management following mechanical heart valve replacement. J Thromb Thrombolys. 2000;9:S41–S45. doi: 10.1023/a:1018712520472. [DOI] [PubMed] [Google Scholar]
- 3.Sawicki PT for the Working Group for the Study of Patient Self-Management of oral Anticoagulation. A structured teaching and self-management program for patients receiving oral anticoagulation: a randomized controlled trial. JAMA. 1999;281:145–150. doi: 10.1001/jama.281.2.145. [DOI] [PubMed] [Google Scholar]
- 4.Ansell JE. Empowering patients to monitor and manage oral anticoagulation therapy. JAMA. 1999;281:182–183. doi: 10.1001/jama.281.2.182. [DOI] [PubMed] [Google Scholar]
- 5.Finkelstein J, Cabrera M, Hripcsak G. Internet-based Home Asthma Telemonitoring: Can patients handle the technology? Chest. 2000;117:148–155. doi: 10.1378/chest.117.1.148. [DOI] [PubMed] [Google Scholar]
- 6.Finkelstein J, O’Connor GT, Friedman RH. Development and implementation of the Home Asthma Telemonitoring system to facilitate asthma self-care. Medinfo. 2001;10(pt 1):810–814. [PubMed] [Google Scholar]
- 7.Finkelstein J, O’Connor GT, Galichina N. Feasibility of Internet-based Home Automated Telemanagement in patients with Chronic Obstructive Pulmonary Disease. Chest. 2001;120(4suppl):253S. [Google Scholar]
- 8.Finkelstein J, Nambu S, Ansell J. Computer-assisted education for patients on anticoagulation therapy. International Journal of Behavioral Medicine. 2002;9(1suppl):87–88. [Google Scholar]
- 9.Gulliksen J, Lantz A, Boivie I. User centered design – problems and possibilities. SIGCHI Bulletin. 1999;31:25–35. [Google Scholar]
- 10.Nielsen J. Usability Engineering. Academic Press. San Diego, CA. 1993.
- 11.Nguyen TD, Attkisson CC, Stegner BL. Assessment of patient satisfaction: Development and refinement of a service evaluation questionnaire. Evaluation and Program Planning. 1983;6:299–313. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- 12.Ansell JE. Anticoagulation management as a risk factor for adverse events: Grounds for improvement. J Thromb Thrombolys. 1998;5(suppl):S13–S18. doi: 10.1023/a:1013276601930. [DOI] [PubMed] [Google Scholar]
- 13.Ansell JE, Hughes R. Evolving models of warfarin management: Anticoagulation clinics, patient self-monitoring and patient self-management. Amer Heart J. 1996;132:1095–1100. doi: 10.1016/s0002-8703(96)90040-x. [DOI] [PubMed] [Google Scholar]
- 14.Ansell J, Hirsh J, Dalen J, Bussey H, Anderson D, Poller L, Jacobson A, Deykin D, Matchar D. Managing oral anticoagulant therapy. Chest. 2001;119:22S–38S. doi: 10.1378/chest.119.1_suppl.22s. [DOI] [PubMed] [Google Scholar]