Abstract
Little is known about the opportunities for a community clinical data exchange network to influence patient care. Rates of patient “cross-over” among different institutions can provide one estimate of the additional value such systems have over unconnected, independent institutional electronic medical records. The Indiana Network for Patient Care (INPC) represents such a system, involving a collaboration of central Indiana hospitals to improve patient care. During a one year study period, 288,696 patients made 471,640 Emergency Department (ED) visits within the INPC collaboration -- accounting for 92% of all Indianapolis ED visits. Overall 25% of the patients with more than one visit also visited one of the other five hospital systems, accounting for 19% of all visits. Our results help clarify the expected frequency within one large metropolitan area that ED patients could obtain direct benefit from a community clinical data exchange network.
INTRODUCTION
Most studies have examined the clinical value of electronic medical records (EMRs ) at only single institutions.1 Owing to a lack of working examples, much less is known about what additional value a community clinical data exchange network could provide. The ability to exchange clinical data across multiple distinct institutions is just beginning to be studied. The supplemental value of aggregating data with a community-wide focus, rather than only on an institution-wide basis, would be expected to be directly related to the frequency in which patients visit multiple different institutions.
Little is known regarding the characteristics of Emergency Department (ED) usage. Reason would indicate that as the number of patient visits increases, so would the probability of ED “cross-over”, i.e. a patient from one system being treated in a separate healthcare system. The percentages of a patients “crossing-over” to another system have yet to be shown. To fully understand the potential value for regionalizing the exchange of clinical data, we first need to demonstrate how patients migrate throughout a community healthcare system. Various parameters may reflect the rationale for why patients prefer specific EDs to receive their medical care. Primary care clinic, insurance status, transportation, and medical necessity are just a few reasons mentioned.
The Indiana Network for Patient Care (INPC)2, 3 was established to provide electronic clinical information originating from all the major Indianapolis hospitals to ED physicians at the point of care. ED medical care has specific characteristics that make it particularly likely to benefit from a clinical data exchange network. First, ED patients can present confused or unconscious4. Information on medications, allergies, prior visits and hospitalizations, diagnoses, previous laboratory and radiology data is even more critical when the patient is unable to give a history and “time is of the essence.” Second, given the lack of a formal relationship to a primary care-giver, it is likely that some patients may consider different EDs as interchangeable. Third, mass casualty incidents and increased ambulance diversion will result in patients being treated outside their primary care network. Finally, ED visits represent a major portion of medical care. In 2000, there were 108.8 million visits (39% of the US population) to EDs 5.
The INPC utilizes two variables critical to determining the frequency that individuals living within a large metropolitan area present to unaffiliated EDs: 1) registration messages indicating that individuals are presenting to an ED and 2) identifiers that allow the patient to be uniquely identified. Specifically, as a part of this collaborative project, participating Indianapolis EDs send real-time registration HL7 messages when patients “check-in” to the different EDs. The Regenstrief Medical Record System6 uses the patient identifiers sent in these messages to match patients across institutions. We describe the “cross-over” rates of patients among the various Indianapolis EDs. This information provides one estimate of the opportunities for cross-institutional data to influence medical care.
MATERIALS AND METHODS
The INPC is an operational community clinical data exchange network founded in 1994.2 It was formed as part of a collaborative effort organized by the Regenstrief Institute, with the approval of the Indiana University Institutional Review Board. The network is centered in the greater metropolitan area of Indianapolis, within which over 1.5 million individuals reside.
While the INPC includes 13 hospitals, we examined data from nine hospitals with the highest ED visit volumes. These hospitals represent five autonomous and competing health care systems, which provide the great majority of acute medical care in Indianapolis. Two of the nine facilities are designated level 1 trauma centers and receive major trauma by protocol. The on-going success of the INPC is the result of the underlying clinical need for cooperation among EDs, inter-organizational data sharing agreements, uniform patient consent language, and fierce security measures to ensure the privacy of the data.
We received clinical and demographic data from the participants as real-time HL7 messages. We also acquired ED log data including date of visit, chief complaint, gender, hospital, and hospital medical record number. We developed processes to map each institution's laboratory variable names to a standard set of LOINC codes in order to allow for the merged presentation of data. In addition, patient identifiers were matched across participating institutions. Using a patient registry linkage program, we identified unique patients using demographic data -- name, social security, age, gender, and ethnicity. By such means, a “global patient index” is created, allowing for the cross-institutional linking of patient information.
Data were exported to a Microsoft Access Database (Microsoft Corp., Redmond, WA). SQL queries were performed to determine the annual ED visit census from the selected institutions, the distribution of visits among patients, and the numbers of patients “crossing over” among the hospital systems.
In addition to examining the ED encounters for the one year period, we also extracted data on how many different health systems’ repositories contained data of any kind for these patients. Owing to the evolution of the INPC, the clinical data repositories contain data from 2 to over 30 years.
RESULTS
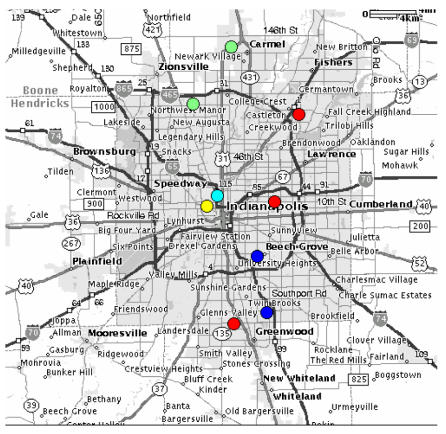
The nine hospitals (figure 1) included in this analysis provided 474,712 episodes of emergency care over a one year period. (September 1, 2001 to August 31, 2002) We excluded 3,072 visits (0.6%) with patient identifiers that were not included in the global patient index file.
Figure 1.
Locations of INPC Participating Hospitals Each circle represents one hospital. Each color represents a separate hospital system.
A total of 288,696 patients accounted for the resultant 471,640 ED visits. These 471,640 visits constituted 92% of all ED visits in Indianapolis during the study period. (Based on self-reported data from the Indianapolis EDs not included in this study).
On average, each patient had 1.6 (range 1–140) ED visits during the one year study period. Thirty-one percent (89,043) of the patients had more than one visit, accounting for 58% (271,987) of the total number of visits.
Table 1 summarizes the characteristics of the hospital systems by unique patients, number of visits and level-1 trauma status.
Table 1.
| Hospital System | Unique Patients | Number of Visits | Level-1 Trauma Center |
|---|---|---|---|
| 1 | 62395 | 110063 | Yes |
| 2 | 62241 | 92307 | Yes |
| 3 | 72995 | 103064 | No |
| 4 | 66335 | 100042 | No |
| 5 | 49549 | 66165 | No |
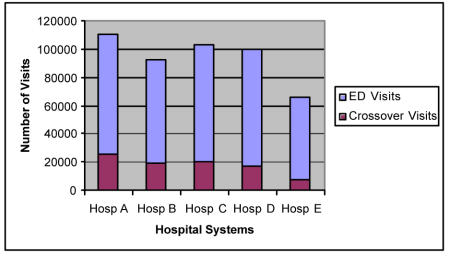
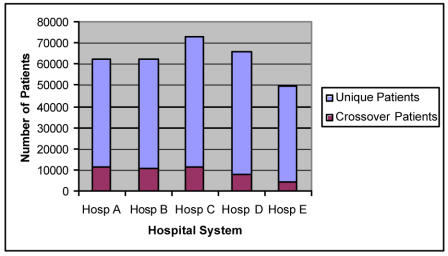
Overall, 7.6% of all ED patients visited more than one of the five hospital systems. Further, 25% (22,007) patients with more than one visit visited more than one hospital system. These patients accounted for 89,257 visits, 33% of the repeat visits, and 19% of the total visits. The distribution of patient crossover for the different hospital systems ranged from 9 to 19%. Figure 2 summarizes the number “cross-over” visits out of total ED visits, while figure 3 summarizes similar information by patient.
Figure 2.
Total Visits by Hospital System
Figure 3.
Total Unique Patients per Hospital System
Aside from ED visits, we also determined the percentage of these patients that had any clinical data in the data repositories of the five different hospital systems. This clinical data spans over the last six years, and in one system, as far back as thirty years. We found that 60% of these patients had data in more than one system. More specifically, forty percent had data in one system, 39% had data in two, 17% in three, 3.7% in four, and less than 1% had data in five.
DISCUSSION
During this brief one year period, we found that 25% of the patients with more than one visit also visited one of the other five hospital systems, accounting for 19% of all visits. Our estimates for the rates of patient flow among different hospital systems are likely fairly reliable given that the INPC “captured” an estimated 92% of all Indianapolis ED visits.
This is the first study to describe the pattern of ED usage in a large community setting. Over this one year period, almost one out of five patient encounters, 19%, had clinical data in another hospital system. Although only 7.6% of the total number of patients sought ED medical care in more than one hospital setting during this one year period, we found that 60% of these same ED patients had clinical data scattered in more than one hospital system over a longer period of time.
We made two decisions that could potentially limit our results. First, we only looked at one year of ED visit data and second, we made the assumption that records from a single healthcare system (with multiple EDs) would be available from within that hospital system. However, even with these limitations, if we were to extrapolate these “crossover” rates nationally, the CDC data suggests 20.6 million ED visits would have clinical information located in another, separate facility.
These results provide a single estimate of the additional clinical value a community clinical data exchange network may play in comparison to the alternative of multiple independent institutional EMRs. Further opportunities exist for a community clinical data exchange network to directly influence ED medical care. Our earlier findings suggest that such a community clinical data exchange network is potentially cost-saving.3 The fully realized value of such a system will be a complex function of crossover rates, the richness of the data available, and the presentation of the data.
We have indirectly evaluated the potential benefits of a community clinical data exchange network to individualized patient care. Such value will likely be ultimately assessed by multiple approaches -- e.g., adherence to standards of care, mortality, and cost savings.
In addition to individualized clinical care, such systems are likely to prove invaluable to epidemiologic and other forms of research. They can also help justify efforts necessary to identify unique patients, standardize messages, merge clinical data, and provide the underlying network necessary to construct and maintain such a network. Insofar as patients only visit a single hospital care system, an institution-wide EMR is completely adequate. Not surprisingly, we found evidence that the proportion of patients with such opportunities increased when we looked at a longer observation period and data generated in multiple care settings.
The Institute of Medicine report suggests regional computer based patient records could result in both time and cost savings for both the patient and physician. A community clinical data exchange network may well reduce diagnostic testing and its attendant discomfort and cost, better prescribing, as well as the epidemiologic research and outcomes management opportunities.7, 8 We are just beginning to realize the full potential of collecting such clinical information. Once these clinical information systems are integrated, data must be transformed into useful information and knowledge to guide clinical decision-making, continuous quality improvement, and reduce the cost of health care delivery.
Acknowledgments
This work was performed at the Regenstrief Institute for Health Care in Indianapolis, Indiana and was supported in part by grants from the National Library of Medicine (T15 LM07117-06) and Contract N01-LM-6-3546
REFERENCES
- 1.IOM Committee on Improving the Patient Record. The Computer-based Patient Record: An Essential Technology for Health Care, Revised Edition. 2nd ed. Washington, D.C: National Academy Press; 1997. [PubMed]
- 2.Overhage JM, Tierney WM, McDonald CJ. Design and implementation of the Indianapolis Network for Patient Care and Research. Bull Med Libr Assoc. 1995;83(1):48–56. [PMC free article] [PubMed] [Google Scholar]
- 3.Overhage JM, Dexter PR, Perkins SM, Cordell WH, McGoff J, McGrath R, et al. A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med. 2002;39(1):14–23. doi: 10.1067/mem.2002.120794. [DOI] [PubMed] [Google Scholar]
- 4.Cordell WH, Overhage JM, Waeckerle JF. Strategies for improving information management in emergency medicine to meet clinical, research, and administrative needs. Information Management Work Group. Acad Emerg Med. 1998;5(2):162–7. doi: 10.1111/j.1553-2712.1998.tb02604.x. [DOI] [PubMed] [Google Scholar]
- 5.McCaig LF, Nyhi L. National Hospital Ambulatory Care Survey: 2000 Emergency Department Summary. In: CDC; 2002.
- 6.McDonald CJ, Overhage JM, Tierney WM, Dexter PR, Martin DK, Suico JG, et al. The Regenstrief Medical Record System: a quarter century experience. Int J Med Inf. 1999;54(3):225–53. doi: 10.1016/s1386-5056(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 7.Dick A, Steen E, (eds). The computer based patient medical record. Washington, DC: National Academy Press; 1991.
- 8.GAO, Systems MA. Automated medical records hold promise to improve patient care; 1991.