Abstract
Context
Female sexual pain and dysfunction
Objective
To evaluate the effectiveness of a new site-specific, manual soft-tissue therapy in increasing orgasm and reducing dyspareunia (painful intercourse) in women with histories indicating abdominopelvic adhesion formation.
Design and Intervention
A total of 29 new patients presenting with infertility or abdominopelvic pain-related problems, and also indicating sexual pain or dysfunction, received a series of treatments (mean, 19.5 hours) designed to address biomechanical dysfunction and restricted mobility due to adhesions affecting the reproductive organs and adjacent structures.
Outcome Measures
Primary outcome measures were post-test vs pretest scores on: (1) the Female Sexual Function Index (FSFI) full scale, orgasm domain, and pain domain; and (2) 3 supplemental 10-point rating scales of sexual pain levels. Secondary outcome measures were post-test vs pretest scores in the other 4 FSFI domains (desire, arousal, lubrication, and satisfaction). The Wilcoxon signed-rank test was used for all statistical analyses.
Results
For the 23 patients available for follow-up, the paired FSFI post-test vs pretest scores were significant (P ≤ .003) on all measures. Of the 17 patients who completed the 3 sexual pain scales, the paired post-test vs pretest scores were significant (P ≤ .002)
Conclusions
Many cases of inhibited orgasm, dyspareunia, and other aspects of sexual dysfunction seem to be treatable by a distinctive, noninvasive manual therapy with no risks and few, if any, adverse effects. The therapy should be considered a new adjunct to existing gynecologic and medical treatments.
Introduction
In the course of treating female infertility with a manual physical therapy technique,[1] several of our patients volunteered the fact that they were having "the best sex, the best orgasms ever." To determine the extent of this phenomenon, a question noting changes in orgasm intensity, frequency, and duration was added to the post-therapy outcomes section of the patient follow-up form. The response was sufficient to inspire further investigation.
The purpose of this study was to systematically assess the effectiveness of an innovative, site-specific, manual soft-tissue therapy in increasing orgasm and reducing dyspareunia (painful intercourse) in women with histories indicating abdominopelvic adhesion formation.
Assessing Female Sexual Dysfunction
Relatively recent investigations have found the prevalence of female sexual dysfunction (approximately 40%) to surpass that of males (approximately 30%).[2,3] Despite the higher prevalence, there have been few investigatory studies of female sexual problems and fewer available treatments than for comparable male conditions.[4]
Since the publication of the "Report of the International Consensus Development Conference on Female Sexual Dysfunction: Definitions and Classifications" in 2000, research has advanced. The committee built upon the existing frameworks (ie, the DSM-IV and ICD-10) and expanded its classifications to include both psychogenic and physiologic causes of arousal, desire, orgasm, and sexual pain disorders.[5] Thus, despite the fact that dyspareunia had long been considered to be psychogenic, it is now included in "Sexual Pain Disorders" due to its solid biological base (eg, connective tissue, hormonal, iatrogenic, inflammatory, muscular, neurologic, and vascular causes).[6]
Although there is still a lack of consensus regarding the definition and diagnostic framework for evaluating and treating female sexual dysfunction,[4] it has traditionally included a variety of (overlapping) disorders of desire/libido, arousal, lubrication, pain/discomfort, and inhibited (or total absence of) orgasm.[2] Many experts agree that the most authentic way of evaluating subjective sexual responses is in a naturalistic (ie, at home) setting, using a self-report technique.[4] Although earlier measures were largely unidimensional scales (eg, Hoon, Hoon, Wincze[7]), several newer multidimensional self-administered questionnaires have met the basic psychometric criteria for reliability and validity.[8] The Female Sexual Function Index (FSFI) is one of these.[4,8,9]
The FSFI, a 19-item questionnaire, assesses 6 key dimensions (domains) of sexual function in women, including orgasm and pain. The others are arousal, desire, lubrication, and satisfaction. The FSFI full score is obtained by adding the individual domain scores.
Etiology of Dyspareunia and Inhibited Orgasm
Painful sexual intercourse and inadequate (or absence of) orgasms are among the most common complaints of women seeking gynecologic care.[4,10]
Although psychological and interpersonal factors can contribute to all types of sexual dysfunction, physiologic factors play a large role in dyspareunia and orgasmic dysfunction. The causes of dyspareunia include a variety of organic factors, such as condyloma, ectopic pregnancies, endometriosis, pathologic conditions due to childbirth, pelvic inflammatory disease, postoperative scarring from gynecologic surgery, vaginal atrophy, vaginitis, and vulvar lesions.[10] Other etiologies include adnexal pathology; cystitis and interstitial cystitis; inadequate lubrication; pelvic adhesions, congestion or infections; urethral disorders; vaginismus; and vulvodynia (vulvar vestibulitis).[11]
Genital pain during vaginal intercourse may occur upon initial or deep penetration, or both. Inadequate lubrication [pelvic floor dysfunction], vaginal atrophy, vaginismus, and vulvodynia are associated with painful entry. Deep pelvic pain occurs with the other conditions cited above[11] and may be due to the partner's thrusting, which hits pain-sensitive structures. Myofascial restrictions and trigger points in the pelvic floor muscles can cause pain and may also serve as a trigger for neurogenic inflammation of the bladder wall.[12] We believe that many causes of dyspareunia (eg, clitoral and postsurgical adhesions, endometriosis, episiotomy scars, interstitial cystitis, vaginitis, and vulvodynia) may also affect orgasmic capability and overall sexual response.
Value of the Intervention
Clinically, we have observed that site-specific, manual soft-tissue therapy improves soft-tissue mobility, elasticity, and distensibility. Theoretically, mobilization of the soft tissue appears to break down the collagenous cross-links and adhesions that cause pain and dysfunction,[13] including dyspareunia and inhibited orgasm.
Adhesions and Female Sexual Dysfunction
Adhesions are deposits of fibrous tissue that form as a natural response to tissue injury after infection, inflammation, surgery, or trauma. In essence, they are bands of scar tissue with the potential to bind organs to other structures, which leads to multiple symptoms including organ dysfunction and/or pain. Wherever they occur, adhesions distort the anatomy and can cause decreased mobility and function.[14] The pelvic organs and bowels are both common sites of adhesion formation, and many patients describe their pain as "pulling" or "stabbing."
In addition to being a common outcome of pelvic or abdominal surgery, adhesions are known to accompany related conditions such as bowel obstruction, chronic abdominopelvic pain, endometriosis, pelvic inflammatory disease, pelvic spasms, polyps, and tubal obstruction.[15-17] It is presumed that some of these conditions cause, or are caused by adhesions. It is also presumed that some cases of dyspareunia and orgasmic problems may be due to the formation of pelvic adhesions imposing on pain-sensitive structures or altering pelvic biomechanics, including the positions of the pelvic support structures and viscera.
Adhesion Formation
Adhesions begin with a fibrin matrix that is formed as the body responds to tissue injury. In the first days following injury, multiple cellular elements become encased in this matrix. These are gradually replaced by vascular granulation tissue, containing fibroblasts, macrophages, and giant cells. Four days post-trauma, most of the fibrin is gone and more fibroblasts and collagen are present. From Days 5 to 10, the fibroblasts align within the adhesions. By Day 14, the predominant cells present are fibroblasts. These fibroblasts anchor to adjacent collagen fibers and contract, shrinking the tissue.[18-20]
As the fibroblasts align within the structure, collagen is laid down in a haphazard manner, and cross-links begin to form. The result is the formation of a fibrinous adhesion, which may cause a subsequent adherence of the adjacent serosal surfaces. Tissue shrinkage leads to decreased movement of the area that, in turn, creates more mechanical irritation, thus perpetuating the cycle.[18-20] Four to 8 weeks after tissue damage, the collagen fibrils organize into discrete bundles. Eventually, the adhesion matures into a fibrous band. These mechanical components have been proposed as the underlying mechanism of adhesion-related pain.[21]
Manual Physical Therapy and Female Sexual Dysfunction
A search of the literature revealed a dearth of research in the use of manual physical therapy for treating female sexual dysfunction.[1] Most dyspareunia studies focus on its prevalence; treatment information is generally limited to surgical options and psychosocial components.[10] Thus far, we have found only 1 relevant case report. In this instance, the therapist employed soft-tissue mobilization, myofascial release, muscle energy techniques, biofeedback, strengthening and stabilizing exercises, and an orthotics consult to successfully treat dyspareunia in a 42-year-old woman (who also reported abdominal and low back pain). The patient was seen for a total of 31 hours over 1 year.[10]
Methodology
Subjects
Selection
All clinic patients were required to complete a 6-page standard Patient Intake Questionnaire detailing their pain and medical history. Those patients who indicated dyspareunia and sexual dysfunction on the questionnaire (or during their initial evaluation) were asked if they were willing to participate in a research study. Criteria for inclusion were as follows:
Indication of painful intercourse and/or difficulty or inability to orgasm;
Willingness to complete a pre-and post-treatment questionnaire on sexual pain and dysfunction; and
A history indicating likely adhesions due to infectious or inflammatory processes, miscarriage, abdominal and/or pelvic surgery, or trauma within the abdominopelvic area.
A total of 29 women were selected to receive a series of site-specific, manual physical therapy treatments for abdominopelvic pain or dysfunction. Six patients were lost to follow-up.
Gynecologic History
All 23 patients in this study had proven or clinically well-supported suspicion of adhesions. Medical diagnoses included:
| Infectious/inflammatory processes | (23) | 100.0% |
| Abdominopelvic surgery | (20) | 87.0% |
| Confirmed pelvic adhesions | (16) | 69.6% |
| Endometriosis | (15) | 65.2% |
| Abdominopelvic trauma | (7) | 30.4% |
| Pelvic inflammatory disease | (1) | 4.3% |
Characteristics
Study participants were a multiethnic, primarily white group, ranging in age from 25 to 43 years; mean = 33.8 years. The patients were being treated for various types of abdominopelvic pain or dysfunction, including infertility.
Procedures/Interventions
The primary goals of manual therapy are to decrease pain and restore mobility by improving soft-tissue mobility, elasticity, and distensibility. The intent of the manual physical therapy protocol used in this study was to create microfailure of collagenous cross-links, the "building blocks" of adhesions. These unique soft-tissue techniques were developed after extensive study of current, innovative, manual physical therapy methods.
Theoretically, mobilization of the soft tissue may break down collagenous cross-links and adhesions that can cause pain and dysfunction,[13] including dyspareunia and inhibited or absence of orgasms. Thus, following a thorough medical, gynecologic, surgical history and palpatory assessment of the patient's abdomen and pelvis, specific areas of visceral and myofascial cross-linking were determined to be likely adhesion sites due to their restricted mobility.
Focusing on these areas of decreased mobility, the therapist engaged the soft tissues until cross-links were perceived to release. This release was evidenced by increased mobility at the precise sites of visceral and myofascial restrictions after each therapy session. The changes were further demonstrated by improved alignment, biomechanics, and increased range of motion of osseous and soft-tissue structures (eg, improved pelvic floor musculature tone, decreased pelvic floor spasms).
Our professional staff has developed literally hundreds of techniques to address the various conditions and complaints reported by our patients and/or noted by the therapists. A typical technique, shown in Figure 1, is designed to decrease spasm and adhesions between the uterus and the bladder.
Figure 1.
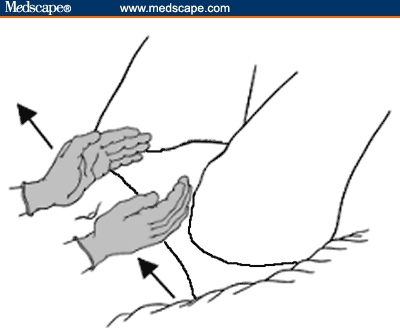
Uterovesical release.
As shown in this example, the therapist engages the uterine fundus and sidewalls and tractions them to the left. To assist and improve the mobility of the soft tissues, the therapist may release the tension of the traction either suddenly or gradually, depending on the desired effect.
In accord with the standards of the American Physical Therapy Association, detailed clinical records were kept of each patient's visit, including treatment dates and duration, symptomatic complaints, areas treated, and treatment techniques performed.[22] Depending on the patient's schedule and geographic location, the frequency and duration of treatment ranged from 2 hours per week for 2+ months to intensive sessions of 2 to 4 hours of treatment daily, performed over 5 days. The standard length of each therapy session was 1 to 2 hours, minus 15 minutes for room preparation and paperwork.
A total of 20/23 (87.0%) patients received the recommended 20 hours of treatment; mean = 19.5 hours. None of the patients received concurrent infertility or pelvic pain therapies during the treatment or 6-week follow-up period.
Data Collection
Study patients were evaluated and treated between October 2002 and January 2004. Since the purpose of this study was to determine the effectiveness of manual soft-tissue therapy in treating female sexual dysfunction -- specifically, increasing orgasm and decreasing dyspareunia -- the data set consisted of the pretreatment and post-treatment scores on 2 assessments of these factors.
1. The Female Sexual Function Index (FSFI), a 19-item questionnaire, was developed in 2000 as a brief, multidimensional self-report instrument for assessing the key factors of sexual function in women. It is easy to administer and psychometrically sound in terms of reliability (test-retest and internal consistency) and construct validity. The FSFI was designed and validated for use in clinical trials or epidemiologic studies. Thus far, it has been validated on clinically diagnosed samples of women with female sexual arousal disorder, female orgasmic disorder, and in women with hypoactive sexual desire disorder.[4,8,9]
The FSFI comprises 6 key dimensions or domains, including orgasm, pain, arousal, desire, lubrication, and satisfaction. The individual domain scores are derived by adding the scores of the individual items constituting the domain and multiplying the sum by the domain factor. The full FSFI score is obtained by adding the 6 individual domain scores.[4]
According to the FSFI authors, "sexual response involves a temporal sequencing and coordination of several phases." Thus, problems in one area may interact with those in another, resulting in a substantial overlap among the diagnostic categories. The FSFI has been designed to assess the relative severity of dysfunction within each domain.[4]
A typical item on the FSFI is Q12:
Over the past 4 weeks, when you had sexual stimulation or intercourse, how difficult was it for you to reach orgasm (climax)?
Response Options:
0 = No sexual activity
1 = Extremely difficult or impossible
2 = Very difficult
3 = Difficult
4 = Slightly difficult
5 = Not difficult
[Note: The complete FSFI questionnaire, instructions and scoring algorithm can be obtained at www.FSFIquestionnaire.com.]
2. Three 10-point scales assessing best, worst, and average pain levels during sexual intercourse were based upon the standard 10-point pain scales used to quantify subjective pain complaints. They were intended to supplement the 3 items representing the pain domain in the FSFI. The worst-best-average nomenclature permitted increased specificity for patients reporting painful intercourse.
The directions for the pain scales (listed as item 20 on the patient pretest and post-test) were simply as follows:
With zero being no pain and ten being the worst pain you could imagine, rate (circle) your own pain levels associated with sexual intercourse over the last four weeks.
My worst pain level during sexual intercourse
1 2 3 4 5 6 7 8 9 10
My best pain level during sexual intercourse
1 2 3 4 5 6 7 8 9 10
My average pain level during sexual intercourse
1 2 3 4 5 6 7 8 9 10
Administration
Since the questionnaire items asked the subjects to rate their responses "over the past 4 weeks...," the pretest was administered at or near the beginning of the actual treatment sessions. The post-test was completed 6 weeks after the last treatment date, thereby allowing 2 weeks post-treatment for the body to assimilate the changes. The post-test was mailed to the patients in a prestamped envelope the previous week. None of the patients had a copy of her pretest responses.
Although all 23 patients completed all 19 items of the FSFI pre-and post-tests, 6 were eliminated from the pain scale analysis due to incomplete data.
Statistical Method
The Wilcoxon signed-rank test[23] was used on the paired difference post-test/pretest for the values where high scores are good (Table 1), and pretest minus post-test where high values are unfavorable (Table 2). Since the questionnaires yielded ordinal (qualitative ranking) data, medians and quartiles are provided in lieu of means and standard deviations.
Table 1.
FSFI Full and Domain Scores (N = 23)
| Domain | Pretreatment Median (Quartiles) |
Post-treatment Median (Quartiles) |
Difference (Post-Pre) Median (Quartiles) |
P Value |
|---|---|---|---|---|
| Full Score* | 19.5 (15.5; 26.7) | 29.1 (23.2; 32.1) | 5.2 (3.1; 12.3) | < .001 |
| Orgasm* | 4.4(2.0; 5.6) | 5.6 (3.2; 6.0) | 0.4 (0.0; 1.2) | < .001 |
| Pain* | 2.4(1.2; 4.0) | 5.2 (4.8; 6.0) | 2.0 (1.6; 4.0) | < .001 |
| Desire | 2.4 (2.4; 3.6) | 3.6 (3.0; 4.2) | 0.6 (0.6; 1.2) | < .001 |
| Arousal | 3.6 (2.4; 4.8) | 4.5 (3.6; 5.4) | 0.6 (0.0; 2.1) | .003 |
| Lubrication | 4.2 (3.0; 5.4) | 5.7 (4.8; 6.0) | 0.9 (0.0; 1.8) | < .001 |
| Satisfaction | 3.2 (2.4; 4.8) | 5.2 (4.0; 6.0) | 1.2 (0.0; 2.0) | < .001 |
Table 2.
10-point Pain Scale Scores* (N = 17)
| Pain Scale | Pretreatment Median (Quartiles) |
Post-treatment Median (Quartiles) |
Difference (Pre-Post) Median (Quartiles) |
P Value |
|---|---|---|---|---|
| Worst | 8 (6; 9) | 3 (1; 5) | 4 (2; 5) | < .001 |
| Best | 2 (1; 4) | 1 (1; 2) | 1 (0; 2) | .002 |
| Average | 5 (3; 6) | 1 (1; 3) | 3 (1; 4) | < .001 |
Results
For purposes of evaluating the effectiveness of site-specific, manual soft-tissue therapy in increasing orgasm and reducing dyspareunia in women with a history indicating probable abdominopelvic adhesions, the primary positive clinical outcomes were defined as improvements on the post-test vs pretest scores on (1) the FSFI full scale, orgasm domain, and pain domain; and (2) the 3 supplemental 10-point scales of sexual pain (worst-best-average).
Although the FSFI was designed to assess the relative degree of dysfunction within each domain, there is a substantial and unavoidable overlap among the diagnostic categories.[4] Thus, secondary positive clinical outcomes were defined as improvements on the post-test vs pretest scores in the other 4 domains of the FSFI (desire, arousal, lubrication, and satisfaction).
In terms of the primary outcome measures, there was a statistically significant improvement on the FSFI full score (P < .001), pain domain (P < .001), and orgasm domain (P < .001) (see Table 1. Indeed, 21 of the 23 patients showed improvement on the FSFI full score. There was also a significant improvement on all 3 pain scales: worst pain (P < .001), best pain (P = .002), and average pain (P < .001) (see Table 2).
In terms of the secondary outcome measures, statistically significant differences in post-test/pretest scores were found on the other 4 FSFI domains: desire (P < .001); arousal (P = .0033); lubrication (P < .001), and satisfaction (P < .001) see Table 1.
[Note: The footnotes to the tables provide the "improved/worsened/tied" data for the 6 FSFI domains and 3 pain scales.]
Discussion
Since the causes of dyspareunia and orgasmic capacity include a number of adhesion-related physiologic factors (eg, inflammation, infection),[10] it is not surprising that a site-specific, manual soft-tissue therapy designed to treat these would prove so effective. Pain and orgasm represent 2 (ie,one-third) of the 6 domains comprising the FSFI; thus, it follows that improvements in these would automatically result in improved overall sexual function, as evidenced on the post-test FSFI full score.
On the other hand (and despite the known overlap in the diagnostic dimensions of female sexual functioning), it was surprising to find that the therapy apparently effected equally significant improvements on all quantifiable domains of this complex phenomenon, including desire, arousal, lubrication, and satisfaction. The unforeseen effectiveness of a manual physical therapy technique upon all 6 FSFI domains clearly supports the view that the "psychobiology of the experience of sexual pain"[6] and orgasm needs to be addressed from a comprehensive perspective.
Future Research
These exceptionally encouraging results raise 2 immediate questions: (1) How would this distinctive protocol compare with a more traditional type of massage therapy (eg, Swedish) in treating women with sexual dysfunction? (2) Could this specific therapy also benefit women lacking strong indications of adhesion formation?
Accordingly, 2 planned studies of sexual dysfunction will have much larger samples of subjects, randomized into experimental (treatment) and control ("standard massage") groups. The studies will test the hypothesis that this distinctive protocol of site-specific, manual soft-tissue treatment is superior to traditional massage therapy in treating sexual dysfunction in women with and without histories of abdominopelvic adhesions.
Subsequent studies will investigate the relative efficacy of the therapy on different types of dyspareunia; ie, painful entry vs deep pain during sexual intercourse.
Conclusion
The results of the present study suggest that many cases of orgasm dysfunction and dyspareunia are treatable by a distinctive site-specific protocol of manual soft-tissue therapy. The treatment also seems to improve other aspects of sexual dysfunction, including desire, arousal, lubrication, and satisfaction. The therapy, designed to maximize function by restoring visceral, osseous, and soft-tissue mobility, is a nonsurgical, noninvasive technique with no risks and few, if any, adverse effects. As such, it should be considered a new adjunct to existing gynecologic and medical treatments of sexual pain and dysfunction.
| FSFI Domain | Improved-Worsened-Tied |
|---|---|
| Full Score | 21–1–1 |
| Orgasm | 13–1–9 |
| Pain | 22–0–1 |
| Desire | 18–3–2 |
| Arousal | 17–5–1 |
| Lubrication | 16–1–6 |
| Satisfaction | 15–4–4 |
| Pain Scales | Improved-Worsened-Tied |
|---|---|
| Worst | 15–1–1 |
| Best | 10–0–7 |
| Average | 15–0–2 |
Acknowledgments
We would like to thank Emily F. Hoon, PhD, and Marvin H. Heuer, MD, for encouraging us in this endeavor. We also thank Cynthia Hodgson, PT, PhD; Kimberley Hornberger, PTA; and Amy B. Hough for their many valuable contributions.
Footnotes
Corresponding Author: L.J. Wurn, Clear Passage Therapies, 3600 NW 43rd Street, Suite A-1, Gainesville, FL 32606. www.clearpassage.com. Email: cptherapy@aol.com.
Contributor Information
C Richard King, Florida Medical and Research Institute, P.A., Gainesville.
Eugenia S Scharf, medical writer/researcher, Gainesville.
Jonathan J Shuster, Department of Statistics, College of Medicine, University of Florida, Gainesville.
References
- 1.Wurn BF, Wurn LJ, King CR, Heuer MA, Roscow AS, Scharf ES, Shuster JJ. Treating female infertility and improving IVF pregnancy rates with a manual physical therapy technique. Medscape General Medicine. 2004;6(2). Available at http://www.medscape.com/viewarticle/480429. [PMC free article] [PubMed]
- 2.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-544. [DOI] [PubMed] [Google Scholar]
- 3.Read S, King M, Watson J. Sexual dysfunction in primary medical care: prevalence, characteristics and detection by the general practitioner. J Public Health Med. 1997;19:387-391. [DOI] [PubMed] [Google Scholar]
- 4.Rosen R, Brown C, Heiman J, et al. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J. Sex Marital Ther. 2000;26:191-208. [DOI] [PubMed] [Google Scholar]
- 5.Basson R, Berman J, Burnett A, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol. 2000;163:888-893. [PubMed] [Google Scholar]
- 6.Graziottin A. Etiology and diagnosis of coital pain. J Endocrinol Invest. 2003;26(3 Suppl):115-121. [PubMed] [Google Scholar]
- 7.Hoon EF, Hoon PW, Wincze JP. An inventory for the measurement of female sexual arousability. Arch Sex Behav. 1976;5:291-300. [PubMed] [Google Scholar]
- 8.Jones le RA. The use of validated questionnaires to assess female sexual dysfunction. World J Urol. 2002;20:89-92. [DOI] [PubMed] [Google Scholar]
- 9.Meston CM. Validation of the female sexual function index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J Sex Marital Ther. 2003;29:39-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holland A. Physical therapy intervention for dyspareunia: a case report. J. of the Section on Women s Health. 2003;27:18-20. [Google Scholar]
- 11.Heim LJ. Evaluation and differential diagnosis of dyspareunia. Am Fam Physician. 2001;63:1535-1544. [PubMed] [Google Scholar]
- 12.Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J. Urol. 2001;166:2226-2231. [DOI] [PubMed] [Google Scholar]
- 13.Threlkeld AJ. The effects of manual therapy on connective tissue. Phys Ther. 1992;72:893-902. [DOI] [PubMed] [Google Scholar]
- 14.Strickler RC. Factors influencing fertility. In: Keye WR, Chang RJ, Rebar RW, Soules MR, eds. Infertility: Evaluation and Treatment. Philadelphia, Pa: W.B. Saunders, 1995: 8-18.
- 15.Drollette CM, Badawy SZ. Pathophysiology of pelvic adhesions. Modern trends in preventing infertility. J Reprod Med. 1992;37:107-122. [PubMed] [Google Scholar]
- 16.Stone K. Adhesions in gynecologic surgery. Curr Opin Obstet Gynecol. 1993;5:322-327. [PubMed] [Google Scholar]
- 17.Steege JF, Stout AL. Resolution of chronic pelvic pain after laparoscopic lysis of adhesions. Am J Gynecol. 1991;165:278-283. [DOI] [PubMed] [Google Scholar]
- 18.Ellis H. The cause and prevention of postoperative intraperitoneal adhesions. Surg Gynecol Obstet. 1971;133:497-511. [PubMed] [Google Scholar]
- 19.Raftery AT. Effect of peritoneal trauma on peritoneal fibrinolytic activity and intraperitoneal adhesion formation. Eur Surg Res. 1981;13:397-401. [DOI] [PubMed] [Google Scholar]
- 20.Holtz G. Prevention and management of peritoneal adhesions. Fertil Steril. 1984;41:497-507. [DOI] [PubMed] [Google Scholar]
- 21.Kresch AJ, Seifer DB, Sachs LB, Barrese I. Laparoscopy in 100 women with chronic pelvic pain. Obstet Gynecol. 1984;64:672-674. [PubMed] [Google Scholar]
- 22.American Physical Therapy Assn. Guide to Physical Therapist Practice, 1st ed. Alexandria, Va: APTA. 1997: Appendix 7-2 7-3. [Google Scholar]
- 23.Lehmann EL. Nonparametric Statistical Methods Based on Ranks. San Francisco, Calif: Prentice-Hall; 1975: 123-132. [Google Scholar]


