Abstract
The purpose of this retrospective study was to identify factors associated with quill injury in dogs. A second objective was to determine the risk of complications and any factors that would predict the likelihood of complications. Hospital records of 296 porcupine quill injuries in dogs from 1998 to 2002 were studied. There was an increased occurrence of porcupine encounters in the spring and fall months; Siberian huskies, rottweilers, and German shepherd crosses were significantly overrepresented for quill injuries. There was no association between risk of complications and either number of quills or antimicrobial use. Increasing time between quill injury and presentation was associated with an increased risk of complications. Because of the increased frequency of complication with a longer interval until presentation, clients should be strongly encouraged to bring the dog in as soon as the quill injury is discovered. Patients presented after 24 hours should be monitored closely during the first 3 weeks after injury, as most complications occurred during this time.
Résumé
Blessures par piquants de porcs-épics chez le chien : rétrospective de 296 cas (1998–2002). Le but de cette étude rétrospective était d’identifier les facteurs associés aux blessures par piquants chez les chiens. Un deuxième objectif était de déterminer le risque de complications et tout facteur pouvant aider à prévoir le risque de complications. Les dossiers médicaux de 296 blessures par piquants de porcs-épics chez le chien ont été étudiés entre 1998 et 2002. On a constaté une augmentation de l’éventualité d’une rencontre avec les porcs-épics au printemps et en automne; les Huskies sibériens, Rottweilers et Bergers allemands de races croisées étaient significativement plus à risque d’être blessés par les piquants. Il n’y avait pas d’association entre le risque de complications et le nombre de piquants ou l’utilisation d’antimicrobiens. L’augmentation de la période de temps écoulée entre la blessure par piquants et la présentation était associée à un risque accru de complications. À cause de l’augmentation de la fréquence des complications reliées à l’allongement de l’intervalle entre la blessure et la présentation, les clients devraient être fermement encouragés à apporter leur chien dès qu’ils s’aperçoivent de l’incident. Les chiens présentés après 24 h devraient être étroitement surveillés au cours des 3 semaines suivantes puisque la majorité des complications surviennent à ce moment.
(Traduit par Docteur André Blouin)
Introduction
The porcupine (Erethizon dorsatum) is a nocturnal quill-bearing rodent common throughout North America (1,2). Porcupines are often found in forests and shrubby ravines (3). Quills cover the entire body of the porcupine (3). When threatened a porcupine will face away from its aggressor with erect quills and slash at the attacker with its tail (3). The loosely rooted quills detach from the porcupine on contact (3). The tip of each quill is covered with backward-pointing barbs. Beyond the barbed tips, the shaft is smooth and hollow. A quill embedded in tissue will migrate into deeper tissues rather than back out (1,2). Animals that are involved in a porcupine encounter (coyotes, wolves, dogs) often break quills off at the surface of their skin after the encounter (4).
Encounters between dogs and porcupines, resulting in quill injury, are common in regions where porcupines are endemic, but few papers have described the frequency of and outcomes in dogs receiving quill injuries (5–8). Reported problems include pain, local tissue irritation/trauma, infection of tissues deep to the skin, quill migration into joints or vital organs, and complications associated with penetration of thorax or abdomen (4–9).
Untreated or incompletely removed quills may migrate. Migration of quills, similar to migration of other organic foreign bodies (grass awns, thorns etc.), can lead to significant complications (10–12). Grahn et al (5) described 5 cases of ocular complications due to porcupine quill migration; these cases included intraocular and periorbital migration. Additionally, 3 case reports described discoveries in dogs of migrating quills in the humeroradial joint (6), temporal fossa (7), and brain (8).
In this retrospective study, medical records of porcupine quill injuries presented to the Western College of Veterinary Medicine Veterinary Teaching Hospital (WCVM-VTH) over a 5-year period (1998–2002) were examined to identify factors associated with presentation for quill removal, determine the risk of complications, and search for factors that might predict the occurrence of complications.
Materials and methods
The medical records of dogs examined for porcupine quill injuries at the WCVM-VTH between January 1, 1998, and December 31, 2002, were reviewed. Age, sex, reproductive status, weight, and breed of these dogs were recorded and compared with those of all hospital admissions for that time period. Also examined were date of quill injury, type of visit (emergency/after hours or regular hours), whether WCVM-VTH was the dog’s primary care facility, anatomic locations of quills, number of quills removed, whether quill remnants were suspected, use of antimicrobials, complications associated with quills, and time from quill injury to presentation. Previous or subsequent visits for quill injury outside this time frame were included for those dogs presenting for quill injury during the study time period, because repeat visits were examined for possible association with complications. Multiple quill injury events in a single animal were examined separately, because each episode could have unique circumstances with different results and complications. Repeat visits by dogs receiving quill injuries could be examined in our study during records review. Computerized hospital admission data could not be adjusted reliably for multiple visits by individual animals, so they were based on total hospital visits.
A combination of invoices and admission time was used to determine if a case was seen after hours or during regular appointment hours. Patient records were examined to determine if the WCVM-VTH was the primary care facility for these clients. It was considered the primary care giver if a client had brought his or her dog in for vaccination or for nonemergency nonreferral health problems more than once.
Time from quill injury to presentation was analyzed for all records. The exact time was used when recorded. In cases where it was not recorded, time was estimated, based on the history and time of presentation. For the purposes of analysis, a history of “quilled tonight” and “quilled last night” when the case was presented during normal business hours was classified as < 12 h, a history of “quilled last night” when the case was presented after hours was classified as 12 to 24 h. “Quilled yesterday” or earlier was classified as > 24 h.
Patients were classified as having complications from quill injury if they had been discharged after initial examination and treatment for quill injuries (at WCVM-VTH or other clinic) and subsequently were presented to the WCVM-VTH for secondary problems related to the presence of quill(s).
Exact logistic regression (PROC Log-Xact5 for SAS; Cytel Software Corporation, Cambridge, Massachusetts, USA and SAS version 8.02 for Windows; SAS Institute, Cary, North Carolina, USA) was used to compare the risk of quill injury among the 50 most common breeds being presented to the hospital. Fischer’s exact test was used post hoc to compare the risk of quill injury for individual breeds with that for the hospital population. The value for statistical significance for the comparison of individual breeds with the overall hospital population was set at P < 0.005 to adjust for the potential for type I error due to multiple comparisons. The association between time from quill injury to presentation (categorical variable; < 12 h, 12 to 24 h, > 24 h), the number of quills (categorical variable; < 30 quills, 30 to 50 quills, > 50 quills), and the occurrence of complications were each examined by using Fischer’s exact tests. When the association between antimicrobial use or number of quills and the risk of complications was examined, multilevel mixed models (binomial distribution and logit link function) were used to adjust for multiple quill injury episodes within dog (MlwiN version 2.0; Centre for Multilevel Modelling, London, United Kingdom). Unless otherwise noted, all comparisons were considered statistically significant at P < 0.05.
Results
Two hundred and ninety-six incidents involving dogs with embedded porcupine quills were evaluated. These included 12 incidents occurring outside the study period that represented previous or subsequent quill removal visits from dogs that were part of the study population. Two hundred and forty-two dogs were seen for the 296 encounters. The 284 visits that occurred during the study period accounted for 2.1% of new hospital cases during the study period.
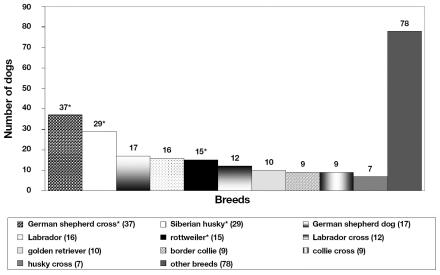
The average age of 215 dogs being presented for their 1st porcupine encounter was 3.27 y (range 0.3 to 12.5 y,); the average age of the hospital population for the same period was 5.36 y. There were 120 females (50.6%) (29% spayed, 20.7% intact) and 119 males (49.4%) (26.6% castrated, 22.8% intact). One dog’s gender was not recorded and 2 female dogs’ reproductive status was unknown. This was similar to all hospital admissions where 52.7% female (30.2% spayed, 22.5% intact) and 47.3% male (25.1% castrated, 22.2% intact) dogs were seen. Hospital visits for quill removal were 5.9 times more frequent in large breeds (> 25 kg) compared with small breeds (< 25 kg) (95% CI, 3.6 to 9.6, P < 0.0001). Large breed dogs accounted for 96% of cases being presented for quill removal, but only 54% of all admissions. A total of 57 individual breeds or crosses were represented in the study population (Figure 1). Repeat visits by individual dogs for quill injury were censored from breed analysis. Compared with total visits by all breeds, Siberian huskies, rottweilers, and German shepherd crosses were significantly over-represented (P < 0.001) for quill removal.
Figure 1.
Breeds presenting for porcupine encounters and quill encounters.
* Over-represented breeds. “Other breeds” includes 43 breeds and crosses
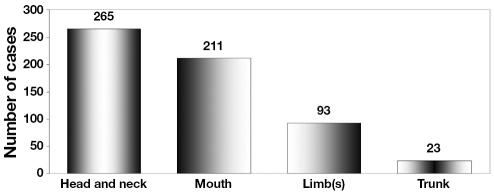
Dogs were treated for quills in every month of the year (Figure 2). There was a higher occurrence in the spring and fall, with 113 (38.2%) cases in September to November, inclusive.
Figure 2.
Distribution of quill injuries with respect to season
Of the 198 incidents of quill injuries that were presented during emergency hours, 43 (21.7%) were considered regular clients of the WCVM-VTH. Of the 98 incidents of quill injuries that were presented during normal business hours, 17 (17.3%) were considered to be regular clients of the WCVM-VTH. After the data had been adjusted for repeat visits, the WCVM-VTH was considered to be the primary care facility for 44 (18.2%) of 242 dogs.
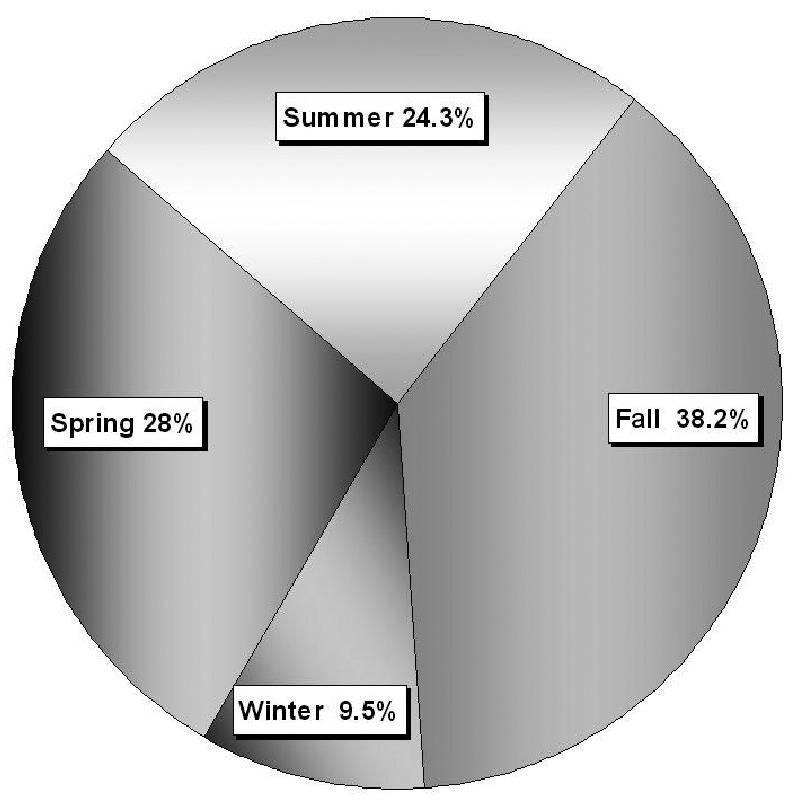
Of the 296 total visits, 288 files recorded the locations of quills on the dog (Figure 3). The most frequent location for quills was the external head and neck region, followed by the oral cavity. Less frequently affected were the limbs and truncal region. The majority of dogs, 223 out of 288 (77.4%), had quills in multiple locations. The average number of quills recovered was 21.8 quills (range 1 to > 100), but in 136 of 296 cases (45.9%), the number of quills removed was not recorded.
Figure 3.
Anatomic distribution of quills.
Of the 296 visits, the attending veterinarian recorded the presence of, or the suspicion of, additional quills remaining after removal in 49 cases (16.5%). The location where quills or suspected quills remained included the hard palate, gingiva, mouth, nose, and face.
Antimicrobials were prescribed after quill removal in 38 (12.8%) of the 296 cases. Duration of administration ranged from 5 to 21 d. Oral antimicrobials included cephalexin, amoxicillin/clavulanic acid, amoxicillin, penicillin, and enrofloxacin. In 4 cases, prophylactic parenteral antimicrobials were given at the time of quill removal. Parenteral antimicrobials included cefazolin in 3 cases, and penicillin G in 1 case. Antimicrobials appeared to be prescribed when the attending clinician performed surgical incisions to retrieve quills, especially if the incision was subsequently sutured.
Thirty-one dogs had more than 1 episode of quill injury. They represented 54 of the 296 visits. A total of 31 dogs accounted for the 54 repeat visits. Seven Siberian husky dogs accounted for 18 (33.3%) of these 54 visits, with 2 huskies accounting for 11 (5 and 6 visits per dog) visits. One weimeraner and 1 bearded collie accounted for 6 repeat visits (3 repeat visits each). The remaining 30 repeat visits were divided among 12 breeds, with most individual dogs having a single repeat visit.
Complications were observed in 32 (10.8%) of 296 cases (Table 1). Eighteen (56.2%) of 32 cases returned within 10 d of the initial quill removal, and 3 (9.4%) of 32 between 10 and 21 d. The remaining 11 cases (34.4%) returned after 21 d, with the longest recorded interval between quill injury and development of complications being 192 d. Twenty-seven (84.4%) of the 32 cases with complications followed the patients’ 1st quill episode. Four dogs developed complications after the 2nd quill episode, 1 had a complication after the 4th quill episode. In 9 (28.1%) of the 32 cases with complications, the WCVM-VTH was considered to be the primary care facility. Because of the small population size, statistical significance between complications and repeated quill injuries could not be determined.
Table 1.
Complications resulting from porcupine quill injury
| Problem at presentation | Number of dogs with clinical signs | Major clinical finding | Number of dogs with major clinical findings | Treatment |
|---|---|---|---|---|
| Lameness | 6 | Intraarticular migration | 2 | Surgical exploration/removal |
| Ocular signs | 4 | Intraocular migration | 2 | Enucleation |
| Localized pain/inflammation/discharge | 22 | Abscess or cellulitis | 28 | Debridement, drainage, and/or antimicrobials |
| Total 32 | Total 32 |
The occurrence of complications did not show any association with the location of the initial quill injury. Of the 32 cases with complications, 26 (81.2%) had quills in the head and neck region. Twenty-six of the complication cases also had quills in the mouth at presentation; these 26 dogs were not necessarily the dogs that had quills in the head and neck region. Fourteen (43.7%) of 32 dogs had quills located in 1 or more limbs at presentation; and 6 (18.7%) of 32 dogs had quills located in the truncal region.
In the 26 dogs with quills in the head and neck region that developed complications, 14 (53.8%) developed complications in that region. Seven (50%) of the 14 dogs with quills in the limbs developed complications in that region. One dog that had had quills in the mouth developed an abscess in the neck region. None of the complications that listed a location occurred in the mouth.
Of the 49 cases where the attending veterinarian recorded or suspected that quills remained, only 5 (10.2%) returned during the study period with a complication.
Seven of 38 (18.4%) cases receiving antimicrobials developed complications. After the data had been adjusted for repeated visits, dogs were 2.8 (95% CI, 0.84 to 5.24; P = 0.11) times more likely to develop complications if they had been sent home with antimicrobials at the time initial quill removal. Twenty-five (9.7%) of the 258 dogs that did not receive antibiotics developed complications. Antimicrobials were prescribed after a complication in 14 (43.7%) of the 32 cases.
The numbers of quills removed, when noted, were not associated with the risk of complications (P > 0.13). The specific number of quills or quill tips removed from a dog with a complication was also not recorded.
Thirty (93.7%) complications were resolved in a single visit. Two cases required 2 and 4 additional visits, respectively, to remove additional quills.
Twenty-two (68.7%) complications were cutaneous abscesses in the respective regions of the previous quill injury (Table 1). These reactions were treated with oral antimicrobials, minor surgical debridement, or drainage of the affected area on an outpatient basis.
Six dogs were presented after a previous quill injury for lameness that required surgical exploration of the painful or swollen area to remove the offending quill(s). Two of these cases were presented 2 to 4 wk after quill removal for effusion of the left carpus. Results from arthrocentesis performed in 1 dog showed neutrophilic inflammation. A quill was located in the palmar aspect of the 4th carpal metacarpal joint and the dorsal region of the carpal metacarpal joint in 2 separate cases; a thickened joint capsule and reactive synovitis was noted in both cases. The remaining 4 dogs were treated for cutaneous cellulitis or abscessation.
Four dogs had periocular complications following quill injury. Quills were retrieved from the medial canthus (1 case), anterior chamber (1 case), and posterior chamber (1 case) of the eye and the eyelids (3 cases). Dogs with ocular involvement had signs and sequelae of intraocular inflammation: panophthalmitis, anterior uveitis, anterior +/− posterior phaecoclastic inflammation, cataract, retinal detachment, or corneal degeneration. In 2 cases with intraocular migration, enucleation was required.
While not considered a complication, because the problem developed after presentation during the original hospital stay, 1 dog developed a suspected quill induced pneumothorax more than 12 hours after presentation. The pneumothorax did not improve after 24 h of medical management. Quills were removed from the cranial mediastinum and cranial lobe of the lung during thoracoscopy. Four additional quills were removed from the axillary and prescapular regions.
Also not considered complications were 3 incidents of porcupine injury that resulted in euthanasia. In all 3 cases, the injuries were not considered life threatening; however, the owners refused further treatment and opted for euthanasia. Two dogs were euthanized during their 1st visit for quill injury; the other dog was euthanized following a 2nd occurrence of quill injury.
In 63 cases (21.3%), the time from receiving quills to presentation was not recorded; 4 (6.3%) of these cases had complications. One hundred and fifty-two cases were presented within 12 h of quill injury; 11 (7.2%) developed complications. Forty-nine cases were presented between 12 and 24 h after quill injury, 4 (8.2%) of these cases had complications. Thirty-two cases were presented more than 24 h after quill injury, 13 (37.5%) had complications. Cases that were presented between 12 and 24 h were no more likely to have complications than were cases presented before 12 h (P = 0.95). The risk, however, did increase with increasing time to presentation. Cases that were presented after 24 h were 5.2 times more likely to have complications than cases presenting before 12 h (P < 0.001).
Discussion
Porcupine quills are unique among migrating foreign bodies that have been reported in the literature, in that an approximate time of acquisition is known and their general location at original presentation is relatively obvious. In previous scientific papers examining foreign body migration, the actual foreign body was discovered after conservative therapy had failed to resolve the initial presenting problem (skin rash/swelling, vomiting, coughing, or limping) and further diagnostic testing or surgical exploration was performed (10–15). In cases involving porcupine quills, the quill is often suspected as the source of the presenting signs because of recent treatment for quill injury.
The overrepresentation of Siberian huskies, rottweilers, and German shepherd crosses may reflect either an increased prey drive in these breeds or that owners of large breed dogs frequent off-leash exercise areas more often than do owners of small breed dogs. Additionally, the study population tended to be younger than the overall hospital population, which may reflect increased activity or decreased obedience among these dogs, increasing the likelihood of a porcupine encounter.
The increased occurrence of quill injuries at certain times of the year is likely due to aspects of dog or owner and porcupine behavior. Porcupines are active year round with peak daily activity occurring in the dusk and dawn hours. Porcupines are more active during the warmer summer months because of foraging or mating behavior (1,2); dog owners are more likely to be active outdoors and to visit off-leash areas with their dogs during the warmer months rather than in winter.
Clinicians did not record details when they were unable to retrieve quills. Speculation based on case descriptions included inability to retrieve a quill because of widespread distribution, depth of penetration, complete or partial removal prior to presentation, breakage, thick hair coat, obesity, or other unknown factors. The number of cases with suspected retained quills that returned with complications may be artificially low, if owners sought further treatment from another clinic or if the quills migrated out of the skin on their own.
That veterinarians attending to complications following quill removal infrequently had information that quills or tips might have remained emphasizes the importance of thorough quill removal, warning owners of potential complications after quill removal, and having quill foreign bodies as a differential when presented with dogs having recent porcupine encounters. The lack of documentation of suspected remaining quills also likely reflects an inherent problem with the retrospective nature of this study.
Deciding that antimicrobials were necessary was not predictive of the ultimate development of complications. Antimicrobials did not appear to affect the complication rate. The empiric use of antimicrobials after initial presentation appeared to reflect extensive surgical exploration or surgical wounds requiring sutures, but it is difficult to speculate how their use affected the complication rate. The level of contamination faced during exploration is also unknown and further complicates the assessment of antimicrobial use.
Most cases had quills in more than 1 location, so, to avoid injury and subsequent complications due to missed quills, a complete physical examination with thorough oral examination is essential.
Several factors may contribute to the significant increase in risk of complication for cases presenting after 24 h. The longer quills remain in a dog, the more time they have to migrate deeper into tissues making them more difficult to find. There is also more potential for breakage and the subsequent difficulty in identification. Owners may delay seeking veterinary care, if they remove quills at home. A higher rate of breakage may be associated with owner removal, but this is unproven. Additionally, quills become less rigid and more friable the longer they remain in tissues, making them more susceptible to breakage during removal.
Patients are generally presented after hours for quill injuries. This may reflect owner behavior and increased porcupine activity at dusk and dawn. Because of the increased frequency of complications with a longer interval until presentation, clients should be strongly encouraged to bring the dog in as soon as the quill injury is discovered.
Fifty-four cases of repeat incidents of porcupine encounters were documented, but other patients may have been treated for additional porcupine encounters elsewhere. Owners should be warned that dogs do not “learn from their mistake” and that repeat quill injury episodes are common.
There are inherent limitations to a retrospective study. In this study, the largest limitations were inconsistent information in medical records and the unknown validity of the complication rate, given the potential for clients to seek medical attention elsewhere. However, the information herein provides a baseline reference to use as a guide for treatment recommendations and prognosis for clients presenting dogs for quill injuries.
Economics or a weak human-animal bond may have played a role in the decision of 3 owners to elect euthanasia rather than pursue treatment for a correctable condition. This further encourages client education as a means of avoiding porcupine encounters. Because porcupine encounters are somewhat seasonal, it may be beneficial to organize public education and awareness programs to decrease the occurrence of the problem. Informational posters on porcupine interaction safety and quill removal guidelines could be displayed at veterinary clinics and popular off-leash parks during peak times. Attending veterinarians could record the geographical location of the porcupine encounter, so that avoidance could be practised where trends are noted. The knowledge that certain breeds are over-represented could be used to educate owners of these large breeds to encourage awareness, specific obedience training, or temporary leashing of dogs in high-risk areas, but any dog may be at risk for having a porcupine encounter. Client education is likely the most powerful means of curbing quill injury. CVJ
References
- 1.Banfield AWF. The Mammals of Canada, Hong Kong: Univ Toronto Pr, 1987:233–235.
- 2.The New Encyclopaedia Britannica, 15th ed., Vol. 9, Chicago: Micropaedia; Peter B. Norton, 1994:614.
- 3.Kavanagh J. Nature Alberta: An Illustrated Guide to Common Plants and Animals Edmonton: Lone Pine Publ, 1991:29.
- 4.Wobeser G. Traumatic, degenerative, and developmental lesions in wolves and coyotes from Saskatchewan. J Wildl Dis. 1992;28:268–275. doi: 10.7589/0090-3558-28.2.268. [DOI] [PubMed] [Google Scholar]
- 5.Grahn BH, Szentimery D, Pharr JW, Farrow CS, Fowler D. Ocular and orbital porcupine quills in the dog: A review and case series. Can Vet J. 1995;36:488–493. [PMC free article] [PubMed] [Google Scholar]
- 6.Brisson BA, Bersenas A, Etue SM. Ultrasonographic diagnosis of septic arthritis secondary to porcupine quill migration in a dog. J Am Vet Med Assoc. 2004;224:1467–1470. doi: 10.2460/javma.2004.224.1467. [DOI] [PubMed] [Google Scholar]
- 7.Mirakhur KK, Khanna AK. Removal of a porcupine quill from the temporal fossa of a dog. Canine Pract. 1983;10:38. [Google Scholar]
- 8.Daoust PY. Porcupine quill in the brain of a dog [letter] Vet Rec. 1991;199:1616. doi: 10.1136/vr.128.18.436-a. [DOI] [PubMed] [Google Scholar]
- 9.Magee AA, Ragle CA, Howlett MR. Use of tenoscopy for management of septic tenosynovitis caused by a penetrating porcupine quill in the synovial sheath surrounding the digital flexor tendons of a horse. J Am Vet Med Assoc. 1997;210:1768–1770. [PubMed] [Google Scholar]
- 10.Houston DM, Eaglesome H. Unusual case of foreign body-induced struvite urolithiasis in a dog. Can Vet J. 1999;40:125–126. [PMC free article] [PubMed] [Google Scholar]
- 11.Brennan KE, Ihrke PJ. Grass awn migration in dogs and cats: A retrospective study of 182 cases. J Am Vet Med Assoc. 1983;182:1201–1204. [PubMed] [Google Scholar]
- 12.Hur DE. Foxtail foreign bodies in dogs and cats. Mod Vet Pract. 1974;55:29–31. [PubMed] [Google Scholar]
- 13.Jackson AH, Degner DA. Cutaneous fistula in a dog caused by migration of a toothpick. J Am Anim Hosp Assoc. 2002;38:545–547. doi: 10.5326/0380545. [DOI] [PubMed] [Google Scholar]
- 14.O’Reilly A, Beck C, Mouatt JG, Stenner VJ. Exophthalmos due to a wooden foreign body in a dog. Aus Vet J. 2002;80:268–271. doi: 10.1111/j.1751-0813.2002.tb10835.x. [DOI] [PubMed] [Google Scholar]
- 15.Morshead D. Submucosal urethral calculus secondary to foxtail awn migration in a dog. J Am Vet Med Assoc. 1983;182:1247–1248. [PubMed] [Google Scholar]
- 16.McGlennon NJ, Platt D, Dunn JK, Chambers JP. Tracheal foreign body in a cat: a case report. J Small Anim Pract. 1986;27:457–461. [Google Scholar]