Abstract
Background
The manner in which fat depot volumes and distributions, particularly the adipose tissue (AT) between the muscles, vary by race is unknown.
Objective
The objective was to quantify a previously unstudied and novel intermuscular AT (IMAT) depot and subcutaneous AT, visceral AT (VAT), and total-body skeletal muscle mass in healthy sedentary African American (AA), Asian, and white adults by whole-body magnetic resonance imaging. IMAT is the AT between muscles and within the boundary of the muscle fascia.
Design
Analyses were conducted on 227 women [AA (n = 79): body mass index (BMI; in kg/m2), 29.0 ± 5.5; age, 45.7 ± 16.9 y; Asian (n = 38): BMI, 21.7 ± 2.9; age, 47.2 ± 19.9 y; whites (n = 110): BMI, 24.9 ± 5.4; age, 43.7 ± 16.2 y]) and 111 men [AA (n = 39): BMI, 25.6 ± 3.2; age, 45.5 ± 18.8 y; Asian (n = 13): BMI, 24.9 ± 2.5; age, 45.6 ± 25.0 y; white (n = 59): BMI, 25.8 ± 3.8; age 44.5 ± 16.3 y].
Results
IMAT depots were not significantly different in size between race groups at low levels of adiposity; however, with increasing adiposity, AAs had a significantly greater increment in the proportion of total AT (TAT) than did the whites and Asians (58, 46, and 44 g IMAT/kg TAT, respectively; P = 0.001). VAT depots were not significantly different in size at low levels of adiposity but, with increasing adiposity, VAT accumulation was greater than IMAT accumulation in the Asians and whites; no significant differences were observed in AAs.
Conclusion
Race differences in AT distribution extend to IMAT, a depot that may influence race-ethnicity differences in dysglycemia.
Keywords: Muscle, adipose tissue, race, aging, body composition, fatness
INTRODUCTION
Adipose tissue (AT) and its distribution are risk factors for metabolic abnormalities (1-3). Whereas obesity is characterized by excess fat mass, the risks associated with excess fatness are thought, in part, to be more a function of where the fat is distributed than of the total amount of fat (1, 2). Greater amounts of visceral AT (VAT) than of subcutaneous AT (SAT) are associated with increased insulin resistance and the metabolic syndrome (3, 4). Given the small quantity of VAT relative to total AT, the associated health risks are striking. Race-ethnicity is known to affect fat and AT distribution (5, 6), and the association of fat distribution with insulin sensitivity varies by ethnicity (7). In Asians, despite their slimness, fat disproportionately accumulates in the abdominal cavity (8, 9), which is thought to increase insulin resistance. For African Americans, however, the data have been contradictory. Despite African Americans having less VAT for a given body mass index (in kg/m2) (5, 6), the prevalence of select risk factors for cardiovascular disease (eg, lower peripheral insulin sensitivity) remains higher than that of other race-ethnicity groups (10, 11). Being African American is an independent risk factor for type 2 diabetes mellitus and for insulin resistance. Bacha et al (11) studied obese white and black adolescents and observed that, whereas differences in fat patterning may help explain the more atherogenic risk profile in whites, the cause of the more diabetogenic insulin sensitivity and secretion profile in blacks remains unknown. A question exists as to whether AT depots other than VAT and SAT might convey metabolic risk.
One less well studied depot is the AT that lies below the SAT fascial plane and not measurable by biopsy or spectroscopy techniques. Two clinical investigations (12) quantified this depot in a single midthigh slice using computed tomography (CT) and found that insulin resistance was associated with increased subfacial AT in obese adults (12) and in thinner older persons (13). Goodpaster et al (12) found that AT located beneath the fascia lata and, therefore, adjacent to skeletal muscle (SM) was significantly negatively correlated with insulin resistance, whereas AT located above the fascia (ie, SAT) and removed from SM was not (12). The former should not be confused with CT-derived lipid within SM, where SM fatty infiltration was identified by the presence of low-density lean tissue (14, 15). Greater low-density muscle or low-attenuation lean tissue in the thigh was associated with lower extremity dysfunction (16) and lower strength, independent of muscle cross-sectional area and body fatness (15) in older persons.
Whole-body magnetic resonance imaging (MRI) protocols allow for the in vivo assessment of body composition, including fat distribution. The primary aim of this study was to describe a novel fat depot called intermuscular AT (IMAT), which is located between muscles with the use of whole-body MRI and to examine its quantity relative to other known fat depots within the body in relation to race. IMAT should not be confused with intramyocellular lipid, which is the lipid within muscle fibers and quantifiable only by using magnetic resonance spectroscopy.
SUBJECTS AND METHODS
Subjects
Subjects were independent, community-dwelling African American, Asian, and white women and men (aged ≥18 y) who had participated in 1 of 5 studies at St Luke's–Roosevelt Hospital's Body Composition Unit between 1996 and 2002. Recruitment occurred through advertisements in newspapers and flyers posted in the local community. Inclusion criteria for all studies required that the subjects be ambulatory, weight stable (±2 kg over the previous 6 mo), nonexercising (based on self-report of no participation in vigorous routine or structured exercise), and nonsmoking. Race was determined by self-report according to the following criteria: all parents and grandparents were required to be of the same race: non-Hispanic African American and non-Hispanic white for African American and white subjects, respectively. The parents and grandparents of the Asians had to be of Eastern Asian origin.
Each subject completed a medical examination and most of the subjects underwent screening blood tests after an overnight fast that included a standard hematology and blood chemistry panel. Subjects with untreated diabetes mellitus, with malignant or catabolic conditions, with a missing limb, with joint replacements, currently taking estrogen replacement therapy, and taking medications that could potentially influence body composition were excluded from the study. Menopausal status was determined by self-report of menses. Women who had not menstruated within the past year were considered postmenopausal. All studies were approved by the Institutional Review Board, and all subjects gave written consent to participate.
Body composition
Subjects reported in the morning in a fasted state to the Body Composition Laboratory. Body weight and height were measured to the nearest 0.1 kg (Weight Tronix, NY, NY) and 0.5 cm (Holtain Stadiometer, Crosswell, Wales), respectively, while the subjects were wearing a hospital gown and foam slippers
Magnetic resonance imaging
Subjects were placed on the 1.5 T scanner (6X Horizon; General Electric, Milwaukee, WI) platform with their arms extended above their heads. The protocol involved the acquisition of ≈40 axial images (10 mm thickness) at 40-mm intervals across the whole body (17). Total-body SM and TAT mass, including total SAT, VAT, and IMAT, were measured from the whole-body multislice MRI.
SliceOmatic 4.2 image analysis software (Tomovision, Montreal, CA) was used to analyze images on a PC workstation (Gateway, Madison, WI). IMAT in our laboratory is defined as IMAT visible between muscle groups and beneath the muscle fascia. To calculate the IMAT within the muscle area, the gray level intensity (threshold value) of the AT in the SAT region is first determined and used as a reference. This threshold value is then reduced by 20% to identify the IMAT threshold (18). MRI-volume estimates were converted to mass by using the assumed density of 1.04 kg/L for SM and 0.92 kg/L for AT (19). All scans were read by the same analyst (PK). The technical errors for 4 repeated readings of the same 4 whole-body scans by the same observer (PK) of MRI-derived SM, SAT, VAT, and IMAT volumes in our laboratory are 1.4%, 1.7%, 2.3%, and 5.9%, respectively.
Data analysis
General linear models were used to investigate the relations among adipose compartment volumes in 3 race groups. Potential differences in IMAT and VAT among race groups were investigated, adjusting for age, height, weight, total adiposity, and SM with those covariates that made significant contributions retained in the model. Potential nonlinear effects of weight and TAT on fat distribution were examined. In women, the independent effects of age and menopausal status on IMAT were also investigated. SM was included as a covariate in some analyses because race differences exist in the quantity of SM mass in which IMAT is located. Sex, race, and the sex-by-race interaction for IMAT and VAT as a percentage of TAT were tested for significance by using the entire sample in an analysis of variance model. In all analyses, a two-tailed α level of 0.05 was used, except when adjustments for multiple comparisons were made.
Data were analyzed by using SPSS version 10.0 (SPSS Institute, Chicago) and SAS version 8.2 (SAS Institute, Cary NC). Results are presented as means ± SDs in the text unless otherwise stated.
RESULTS
Subject characteristics
The descriptive characteristics are summarized in Table 1. Analyses were conducted on 118 African American, 51 Asian, and 169 white men and women with mean ages that were not significantly different. The African American women weighed more and had a higher mean BMI (29.0) than did the white (24.9) and Asian (21.7) women, and most body fat depots reflected the heavier weight. Nevertheless, there was considerable overlap in the distributions. Among men, the African Americans (80.1 ± 11.6 kg) and whites (82.2 ± 12.2 kg) weighed more than did the Asians (72.1 ± 11.3 kg), but BMI did not differ significantly by race. VAT was lowest in the African Americans.
TABLE 1.
Body-composition characteristics of study subjects1
| African American (n = 118) | Asian (n = 51) | White (n = 169) | |
|---|---|---|---|
| Age (y)2 | |||
| Women | 45.7 ± 6.9 (19–87) | 47.2 ± 19.9 (20–83) | 43.7 ± 16.2 (18–88) |
| Men | 45.5 ± 18.8 (20–83) | 45.6 ± 25.0 (21–82) | 44.5 ± 16.3 (19–84) |
| Height (m)3 | |||
| Women | 1.63 ± 0.07 (1.4–1.8) | 1.59 ± 0.06 (1.45–1.7) | 1.63 ± 0.07 (1.5–1.8) |
| Men | 1.77 ± 0.08 (1.5–1.92) | 1.70 ± 0.10 (1.5–1.9) | 1.78 ± 0.07 (160–191) |
| Weight (kg) | |||
| Women | 77.7 ± 16.2a (47.3–107.0) | 54.6 ± 8.9b (40.8–78.0) | 66.2 ± 14.1c (42.3–111.3) |
| Men | 80.1 ± 11.6a (60.5–102) | 72.1 ± 11.3b (57.2–92.7) | 82.2 ± 12.2a,b (54.8–114.0) |
| BMI (kg/m2) | |||
| Women | 29.0 ± 5.5a (17.7–40.9) | 21.7 ± 2.9b (16.9–29.2) | 24.9 ± 5.4c (15.9–39.0) |
| Men | 25.6 ± 3.2a (19.9–31.3) | 24.9 ± 2.5a (20.5–30.4) | 25.8 ± 3.8a (19.9–38.6) |
| Skeletal muscle (kg)4 | |||
| Women | 22.6 ± 3.8 (14.2–31.2) | 16.1 ± 2.4 (11.7–21.1) | 20.1 ± 3.4 (12.3–31.0) |
| Men | 33.3 ± 5.2 (19.7–45.4) | 26.5 ± 5.7 (15.8–35.6) | 32.6 ± 5.2 (20.6–46.1) |
| Total adipose tissue (kg) | |||
| Women | 31.6 ± 11.8a (8.2–55.4) | 18.2 ± 6.9b (9.1–38.5) | 24.4 ± 11.0c (8.6–54.7) |
| Men | 18.7 ± 6.3a (5.6–33.2) | 17.1 ± 5.7a (6.6–26.2) | 20.8 ± 8.4a (9.2–40.5) |
| Subcutaneous adipose tissue (kg) | |||
| Women | 28.5 ± 10.5a (7.7–48.7) | 15.8 ± 5.8b (8.7–17.1) | 22.0 ± 9.7c (8.0–50.8) |
| Men | 16.1 ± 5.3a (5.1–28.8) | 14.1 ± 4.2a (5.6–20.8) | 17.5 ± 6.5a (8.1–31.8) |
| Visceral adipose tissue (kg) | |||
| Women | 1.68 ± 1.1a (0.17–4.82) | 1.63 ± 1.2a (0.21–5.55) | 1.42 ± 1.22a (0.15–5.57) |
| Men | 1.85 ± 1.5a (0.15–5.94) | 2.2 ± 1.7a,b (0.42–5.8) | 2.6 ± 1.9b (0.24–8.5) |
| Intermuscular adipose tissue (kg) | |||
| Women | 1.43 ± 0.76a (0.20–3.68) | 0.81 ± 1.42b (0.16–1.90) | 0.94 ± 0.59b (0.08–3.40) |
| Men | 0.87 ± 0.56a (0.19–2.25) | 0.91 ± 0.46a (0.25–1.73) | 0.74 ± 0.46a (0.08–1.81) |
All values are x̄ ± SD; range in parentheses. For variables with significant race-by-sex interactions, means within the same sex with different superscript letters are significantly different, P < 0.05 (Tukey-Kramer multiple comparison test).
There was no significant race-by-sex interaction and no significant main effect of race or sex.
There was no significant race-by-sex interaction. Men were taller than women. African Americans were not significantly different from whites, and both groups were taller than Asians.
There was no significant race-by-sex interaction. Men had more skeletal muscle than women. African Americans had more muscle than whites, who in turn had more skeletal muscle than Asians.
AT distribution
African Americans had ≈1 kg less TAT than did the other 2 groups after covarying for sex, age, height, and weight (P for trend = 0.072). Race differences in SAT were significant after adjustment for TAT, sex, age, and height (P = 0.001). Adjusted mean (±SD) SAT values were 21.3 ± 1.09 kg for African Americans, 20.4 ± 1.14 kg for Asians, and 21.0 ± 1.04 kg for whites; all pairwise comparisons were significant (P < 0.015, Tukey-Kramer adjusted).
IMAT
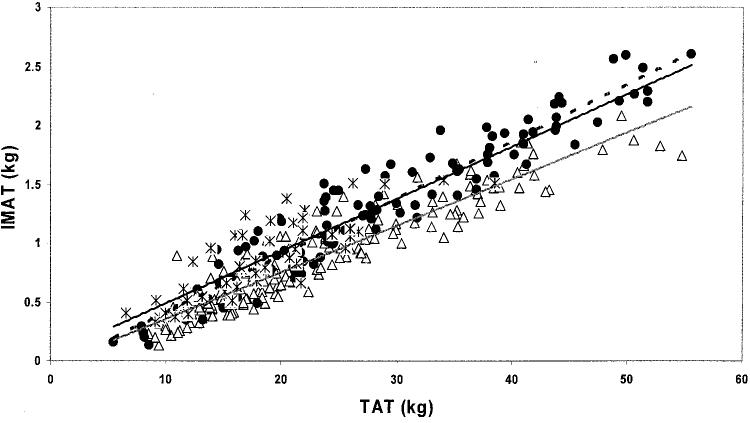
To determine whether IMAT differed by race, the significance of covariates (including age, height, weight, weight squared, TAT, TAT squared, SM, race, sex, and race and sex interactions with TAT) was first tested. The significant variables in the model were age (P < 0.001), weight squared (P = 0.003), TAT (P < 0.001), sex (P = 0.018), and race-by-TAT interaction (P = 0.007) (Table 2). On average, men had ≈0.19 kg more IMAT than did women. The presence of a significant race-by-TAT interaction indicated that the amount of IMAT in relation to TAT depends on race. At low levels of adiposity, African Americans, Asians, and whites had amounts of adjusted IMAT that were not significantly different (Figure 1). According to the regression model, a 70-kg, 45-y-old woman of any race group with ≈10 kg TAT would have ≈0.23-0.35 kg IMAT. However, with increasing adiposity, African Americans had a significantly greater increment in IMAT per kg TAT compared with whites and Asians; IMAT did not differ significantly between whites and Asians (59 g IMAT/kg TAT in African Americans compared with 47 g IMAT/kg TAT in whites and 44 g IMAT/kg TAT in Asians; interaction of slopes, P = 0.001).
TABLE 2.
Regression model coefficients for the relation of intermuscular adipose tissue (AT) to total AT (TAT)1
| Variable | Regression coefficient ± SEE |
|---|---|
| Age (y) | 0.008 ± 0.0012 |
| TAT (kg) | 0.047 ± 0.0052 |
| Race | AA: −0.108 ± 0.111 |
| Asian: 0.158 ± 0.166 | |
| White: 0 | |
| P = 0.291 | |
| Sex | Men: 0.187 ± 0.0793 |
| Women: 0 | |
| Weight2 (kg) | −0.000065 ± 0.0004 |
| Race × TAT | AA: 0.012 ± 0.0044 |
| Asian: −0.0035 ± 0.008 | |
| White: 0 | |
| P = 0.007 | |
| Intercept | −0.306 ± 0.0884 |
| SEE | 0.366 |
| R2 | 0.67 |
n = 338. AA, African American.
P < 0.001.
P < 0.05.
P < 0.01.
FIGURE 1.
Intermuscular adipose tissue (IMAT) predicted from sex, age, weight2, total adipose tissue (TAT), and TAT-by-race interaction, shown in relation to TAT (kg) in African American ([unk]; n = 118), Asian (*; n = 51), and white (△; n = 169) women and men. Linear regression lines are shown for African Americans (- - -), Asians ([unk]), and whites (—). All slopes were significantly different from zero (P < 0.05). All intercepts were significantly different from zero (P < 0.001). The overall SEE = 0.366 kg, as described in the text. African Americans: IMAT =−0.414 + 0.187 (male) + 0.008 (age) + 0.059 (TAT) − 0.00006 (weight2). Asians: IMAT =−0.148 + 0.187 (male) + 0.008 (age) + 0.044 (TAT) − 0.00006 (weight2). Whites: IMAT =−0.306 + 0.187 (male) + 0.008 (age) + 0.047 (TAT) − 0.00006 (weight2).
Age influence on IMAT
IMAT increased with age by ≈9 g/y (P < 0.001) after adjustment for TAT in the total sample, which indicated that the proportion of TAT deposited as IMAT increases with age. The age effect did not differ significantly between race groups. Menopausal status was not significantly related to IMAT after adjustment for age and TAT.
IMAT and VAT in relation to TAT
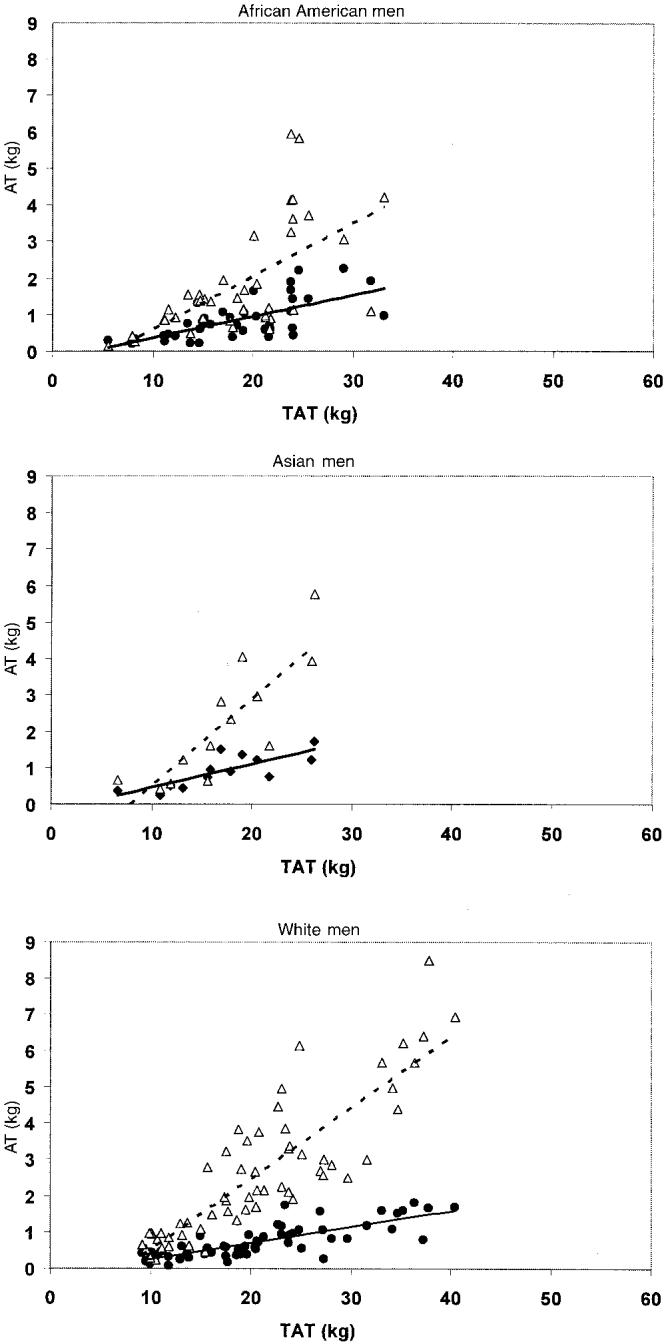
Because VAT is known to increase with age, and it is widely reported that there is more VAT after adjustment for TAT in whites than in African-Americans, we investigated the relation between the amount of IMAT and VAT in each race group (Figures 2 and 3). After VAT was adjusted for the same variables as for IMAT above, the relation between adjusted IMAT and adjusted VAT in relation to TAT differed between African American, Asian, and white groups. According to the regressions, the amounts of IMAT and VAT at low levels of TAT were not significantly different among groups. For example, in a 70-kg, 45-y-old woman with ≈10 kg TAT, there would be ≈0.23-0.35 kg IMAT and ≈0.03-0.45 kg VAT. However, with increasing adiposity, the rate of increase in VAT was greater than that of IMAT in whites (0.087 kg VAT/kg TAT compared with 0.035 kg IMAT/kg TAT) and in Asians (0.113 kg VAT/kg TAT compared with 033 kg IMAT/kg TAT). In African Americans, the rates of increase for VAT and IMAT were parallel and did not differ significantly (0.046 kg VAT/kg TAT compared with 0.046 kg IMAT/kg TAT). According to the regression equation, an African American woman with 35 kg TAT would have 1.71 kg IMAT and 1.94 kg VAT, an Asian woman would have 1.41 kg IMAT and 3.59 kg VAT, and a white woman would have 1.42 kg IMAT and 2.56 kg VAT. Similar relations were observed in the men. The adjusted IMAT and VAT levels, assuming 35 kg TAT in women (Figure 4A) and men (Figure 4B), highlight the greater amounts of IMAT and lesser amounts of VAT seen with increasing adiposity in African Americans than in the other 2 groups.
FIGURE 2.
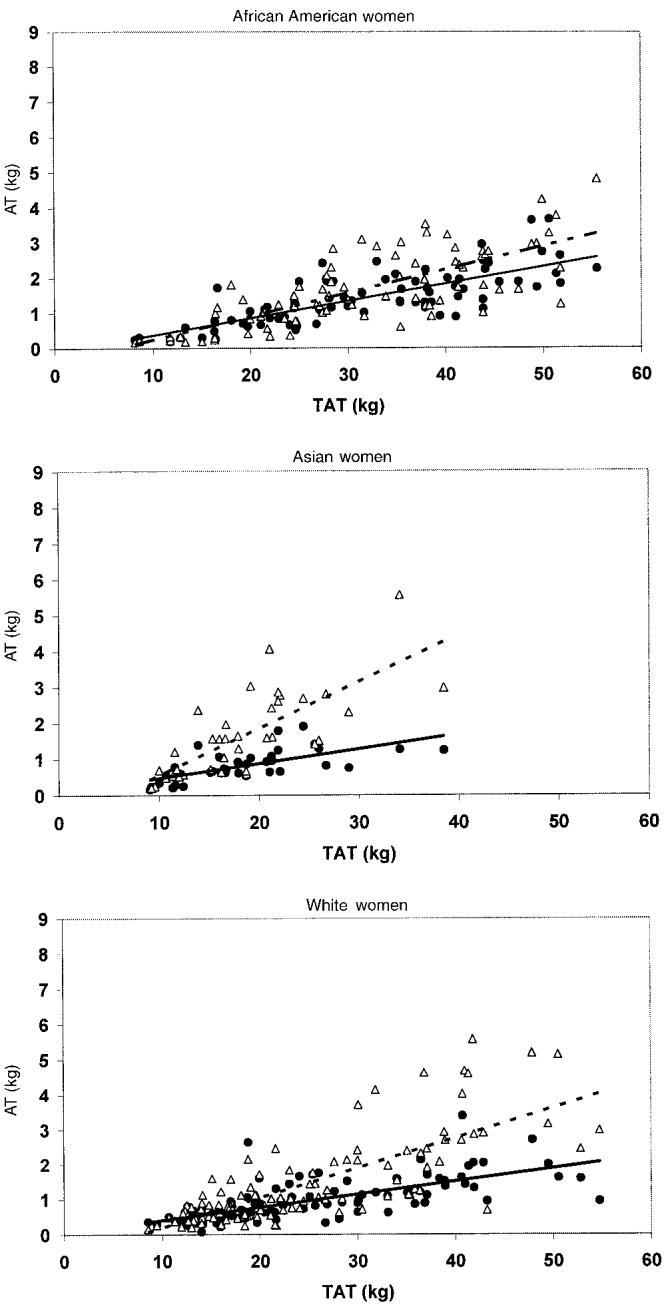
Intermuscular adipose tissue (IMAT; [unk]) and visceral adipose tissue (VAT; △) as a function of total adipose tissue (TAT) in women. Linear regression lines are shown for IMAT ([unk]) and VAT (- - -). All slopes were significantly different from zero (P < 0.001). None of the intercepts were significantly different from zero, except for the regression of VAT in white women (P < 0.001). African American women (n = 79): IMAT = −0.123 + 0.049 × TAT (SEE = 0.495 kg); VAT = −0.423 + 0.067 × TAT (SEE = 0.712 kg). Asian women (n = 38): IMAT = 0.070 + 0.041 × TAT (SEE = 0.322 kg); VAT =−0.729 + 0.129 × TAT (SEE = 0.782 kg). White women (n = 110): IMAT = 0.034 + 0.037 × TAT (SEE = 0.421 kg); VAT =−0.662 + 0.086 × TAT (SEE = 0.782 kg).
FIGURE 3.
Intermuscular adipose tissue (IMAT; [unk]) and visceral adipose tissue (VAT; △) as a function of total adipose tissue (TAT) in men. Linear regression lines are shown for IMAT ([unk]) and VAT (- - -). All slopes were significantly different from zero (P < 0.001). None of the intercepts were significantly different from zero, except for the regression of VAT in white men (P < 0.001). African American men (n = 39): IMAT =−0.217 + 0.058 × TAT (SEE = 0.432 kg); VAT =−0.859 + 0.145 × TAT (SEE = 1.184 kg). Asian men (n = 13): IMAT =−0.179 + 0.064 × TAT (SEE = 0.295 kg); VAT =−1.876 + 0.238 × TAT (SEE = 0.965 kg). White men (n = 59): IMAT = −0.182 + 0.044 × TAT (SEE = 0.276 kg); VAT = −1.425 + 0.195 × TAT (SEE = 0.957 kg).
FIGURE 4.
Mean (±SE) predicted intermuscular adipose tissue (IMAT; ■) and visceral AT (VAT; □) according to the regression equations assuming 35 kg total AT in African Americans (n = 79 women and 39 men), Asians (n = 38 women and 13 men), and whites (n = 110 women and 59 men). Means with different lowercase letters are significantly different, P < 0.05 (adjusted for Tukey-Kramer multiple comparison procedure).
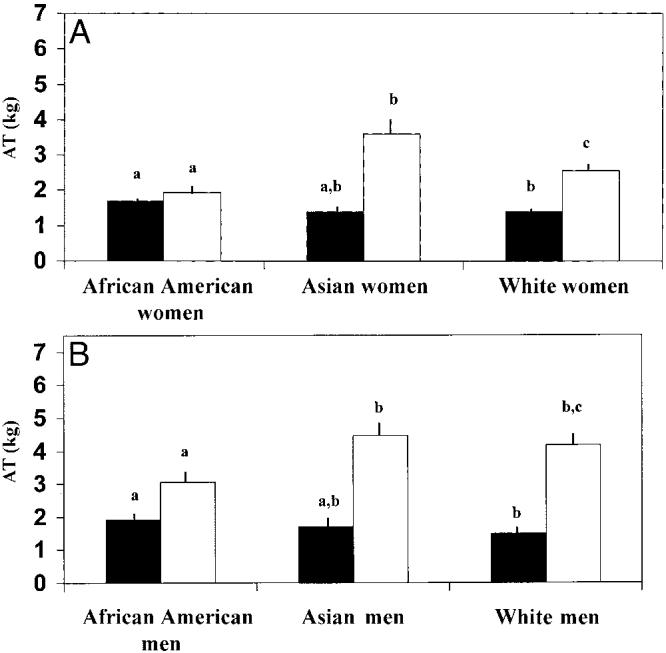
The percentage of TAT in each group that is made up of VAT plus IMAT, unadjusted for other variables, is shown in Figure 5. Within all 3 race groups, IMAT + VAT as a percentage of TAT was greater in men than in women (P < 0.001). IMAT + VAT as a percentage of TAT was not significantly different between African American (9.4 ± 0.4%) and white (9.2 ± 0.4%) women but was greater in Asian women (12.7 ± 0.9%) than in African American (P = 0.001) and white (P = 0.0001) women (Tukey-Kramer adjustment for multiple comparisons). In men, IMAT + VAT as a percentage of TAT was not significantly different between race groups (Tukey-Kramer adjustment for multiple comparisons), although Asians had the largest amounts of TAT (African American: 13.7 ± 1.1%; white: 14.9 ± 0.7%; Asian: 16.9 ± 2.1%).
FIGURE 5.
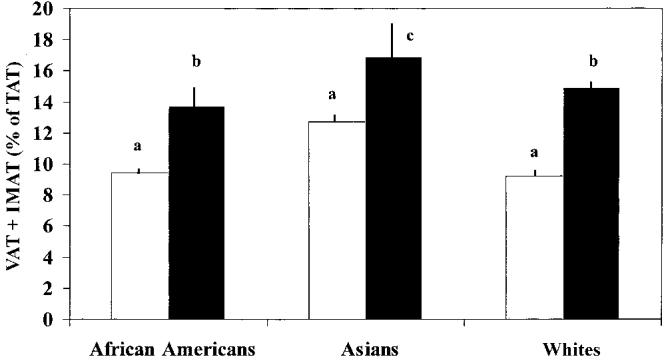
Mean (±SE) amounts of visceral adipose tissue (VAT) plus intermuscular AT (IMAT) as a percentage of total AT (TAT) in African American (n = 118), Asian (n = 51), and white (n = 169) women (□) and men (■). Means with different superscript letters are significantly different, P < 0.001 for race. P values adjusted for Tukey-Kramer multiple comparisons are based on log-transformed (VAT + IMAT) as a percentage of TAT.
DISCUSSION
With increasing adiposity, African American women and men deposit greater quantities of total body IMAT than do whites or Asian women and men, although the difference in the comparison with Asians was not statistically significant because of the small sample size of Asians. This finding contrasts with the reported race differences in VAT, ie, African Americans are reported to have less VAT than do whites. We also found that, at low levels of adiposity, VAT did not differ significantly between African Americans, Asians, and whites. It was only at higher levels of adiposity that VAT was greater in Asians and whites than in African Americans. Asians, who are known to have higher amounts of VAT across all levels of TAT, were shown to have IMAT levels, similar to those of whites. As a result, Asians had the highest proportion of total body fat as IMAT and VAT. Because of the strong association between VAT and well-established risk factors for morbidity and mortality (20) combined with reports that subfacial AT is associated with higher fasting insulin concentrations (13), a more thorough investigation of the clinical implications of IMAT is warranted. This finding also extends our knowledge of race differences in fat distribution and, because of the location of IMAT within an organ (SM) critical to glucose regulation, suggests another potential way that fat distribution could interact with race-ethnicity in metabolic risk.
IMAT
The finding of more IMAT in African Americans was unexpected. Compared with white women, African American women are known to have a higher prevalence of obesity (21), are more predisposed to type 1 (22) and type 2 (23) diabetes, and yet have less VAT, an adipose depot that has been held responsible for much of the association of metabolic and cardiovascular disease risk factors. Our finding of greater IMAT in African Americans and smaller amounts of IMAT in Asians and whites suggests that fat depots other than VAT exist in locations in the body that could contribute to dysglycemia. Others (12) observed that reduced SM attenuation (by CT) was associated with increased SM lipid content (r = 0.43, P < 0.01) and that AT located beneath the fascia lata (ie, IMAT), adjacent to SM, was significantly negatively correlated with insulin sensitivity, whereas AT above the fascia (ie, SAT) and removed from SM was not. In an ongoing study we found that women with type 2 diabetes have more IMAT (P = 0.001) and less SAT (P = 0.02) after adjustment for TAT, age, and SM than do nondiabetic women (24). In adult women (18–69 y), low-density lean tissue within the midthigh muscle correlated with age (r = 0.52, P < 0.005), insulin, (r = 0.34, P < 0.005) triacylglycerol (r = 0.41, P < 0.005), cholesterol (r = 0.50, P < 0.005), and LDL cholesterol (r = 0.53, P < 0.005) (14). Compared with white women, postmenopausal African American women have more CT-derived midthigh low-density lean tissue, have lower glucose utilization, and are less insulin sensitive, despite comparable fitness and relative body fat levels (25).
African Americans are taller, have greater SM mass and bone mass (26), and longer limbs (27) than do Asians and whites, and similar differences have been reported between whites and Asians. Because IMAT is located within the SM area, a large percentage of which is in the limbs, we appropriately adjusted for height and SM mass in the analyses to eliminate their potential confounding effects across race groups. We found that, with increasing adiposity, the size of the IMAT compartment in African Americans grew more rapidly than in whites and Asians and that the difference increased across the range of TAT.
The measurement of whole-body IMAT using MRI differs from the CT technology used in other studies that have reported on SM attenuation or density from a single midthigh CT slice (14, 15). We assessed IMAT between all muscle groups throughout the body and had the advantage that all measurements were conducted by a single analyst, thereby reducing the problem of interreader variability previously described (28). We recently (18) reported increases in whole-body IMAT and VAT in elderly weight-stable AA women over 2 y. Janssen et al (28) reported significant reductions in whole-body IMAT measured by MRI after 16 wk of weight loss in postmenopausal women; however, the IMAT protocol was not described.
VAT
In the current analysis, race differences in VAT, as in IMAT, were found to exist only at higher levels of adiposity and were not statistically evident at lower levels in whites and African Americans; this finding for Asians may be partly an issue of statistical power because Asians did have more VAT throughout the range of TAT. Many studies have reported greater VAT in white than in African American children (29), adolescents (11), and adults (5, 6) and greater VAT in Asians than in white women (8). Studies of race differences in VAT have seldom accounted for TAT, except as a covariate in models (30, 31), and we did not find other investigations of a potential interaction by race in the VAT on TAT association (32). Other studies either have very small sample sizes or have subjects whose BMI is restricted to over-weight or obese rather than spanning the entire range of BMI (5, 6, 32); this would have further limited the ability to detect an interaction of VAT on TAT. Had VAT in the current study been analyzed with the use of a simple t test among overweight (BMI > 25) African Americans compared with whites, we too would have concluded that VAT was significantly lower in African Americans without noting the role of total adiposity. Accounting for the effects of TAT may be an important modifying characteristic that has not been given appropriate attention in earlier analyses.
MRI measurement issues
MRI depends on the density of hydrogen nuclei and the relaxation time of the tissue to separate different tissues of interest. The visual appearances of SM and AT in an image are strikingly different. Because IMAT is often sparsely located throughout the SM area, a problem can arise (where the SM adipose boundary is thin) in identifying where an IMAT depot ends and SM begins (partial volume effects) (33). We adopted a standard protocol that should reduce the partial volume effects. To calculate the IMAT within the muscle area, the gray level intensity (threshold value) of the AT in the SAT region was first determined and used as a reference. This threshold value was reduced by 20% to identify the IMAT threshold (18). Comparisons of MRI with corresponding cadaver analysis of leg and arm sections showed a high correlation (r = 0.92, P < 0.001) for IMAT (34). Use of this protocol, coupled with the advantage of a single reader analyst, reduced the variability in IMAT measurement.
It is important to clarify the difference between IMAT and lipid stored within SM. There are 2 distinct depots of lipid storage within SM: lipids within adipocytes located between muscle fibers, also known as extramyocellular lipids, and lipids located within the muscle fibers in the form of cytosolic triacylglycerols, also known as intramyocellular lipids. IMAT, as described in the current protocol, is attempting to quantify AT located between the muscle bundles.
Study limitations
All components of body composition, including IMAT, are potentially influenced by dietary intake, levels of physical activity or inactivity, and exercise, for which no independent measures were acquired. This study used a convenience sample of urban-dwelling healthy African Americans, Asians, and whites and cannot be considered representative of the general adult population; extrapolation of these findings to females and males of other race-ethnicity groups should be made with caution. The presence of unreported and undiagnosed medical conditions that could affect body composition cannot be ruled out. Race group was determined by self-report, which is reported to be a suitable proxy for genetic ancestry, especially when assessing disease risk (35) but does not take into account degrees of admixture. We had limited power to address differences between Asians and the other 2 groups. We should caution that the use of a regression model in an observational sample to estimate the effect of variation in a single variable, while other variables remain constant, ignores the known natural covariation of these variables. Thus, the relation of IMAT or VAT in relation to TAT, while weight and age are held constant, are for illustrative rather than predictive purposes. It is also possible, given the significant differences in BMI among the ethnic subgroups in our sample, that the variables in our models do not adequately take into account the differences in BMI.
Study strengths
We used a measure of total-body IMAT rather than a single thigh slice as used in previous studies. A substantial number of African Americans and whites had complete measurements and one reader analyzed all scans for IMAT, including a subset that was reread over time to establish intrareader variability. All scans were acquired in one center under high levels of quality control by well-trained examiners skilled in performing a protocol for body-composition measurements.
Conclusions
A novel AT depot within muscle is described in a sedentary population. At higher levels of adiposity, African American women and men have greater quantities of total-body IMAT than do Asians or whites after adjustment for differences in total adiposity and other covariates. This study is the first to report on race differences in whole-body IMAT. In addition, the proportion of IMAT to VAT depots appears to differ between race groups and by level of total adiposity.
Acknowledgments
We acknowledge the contributions of Mark Punyanitya, the Director of Image Reading Center (where the MRI analyses were performed), and Qing He for manuscript editing and formatting.
JA initially put forth the IMAT concept that led to development of the protocol used in this and in our previous study (18). DG developed the whole-body IMAT protocol. TBH and DG were responsible for the study concept (reanalysis of the archived database for IMAT). JA, DG, and SBH provided data. PK was responsible for the MRI analyses. DG and SH were responsible for the analysis and interpretation of data. JA, DG, BG, TBH, SH, and MV critically reviewed the manuscript for intellectual content. SH provided statistical expertise. TBH and DG obtained funding and supervised the study. Each author declared that she or he had no conflict of financial or personal interests in any company or organization sponsoring this study.
Footnotes
From the Department of Medicine, Obesity Research Center, St Luke's–Roosevelt Hospital, New York, NY (DG, SH, JA, and SH); the Institute of Human Nutrition, Columbia University, New York, NY (DG); the Laboratory of Epidemiology, Demography and Biometry, Geriatric Epidemiology Section, National Institute of Aging, Bethesda, MD (PK and TBH); the Department of Medicine, University of Pittsburgh, Pittsburgh, PA (BG); and the EMGO Institute, VU Medical Center, Amsterdam, Netherlands (MV).
Supported by NIH grants AG14715, DK42618, RR00645, and DK40414 and a contract from the National Institute of Aging.
Reprints not available. Address correspondence to D Gallagher, Obesity Research Center, 1090 Amsterdam Avenue, New York, NY 10025. E-mail: dg108@columbia.edu.
REFERENCES
- 1.Rexrode KM, Carey VJ, Hennekens CH, et al. Abdominal adiposity and coronary heart disease in women. JAMA. 1998;280:1843–8. doi: 10.1001/jama.280.21.1843. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Cupples LA, Ramaswami R, Stokes J, III, Kreger BE, Higgins M. Regional obesity and risk of cardiovascular disease; the Framingham Study. J Clin Epidemiol. 1991;44:183–90. doi: 10.1016/0895-4356(91)90265-b. [DOI] [PubMed] [Google Scholar]
- 3.Kissebah AH, Vydelingum N, Murray R, et al. Relation of body fat distribution to metabolic complications of obesity. J Clin Endocrinol Metab. 1982;54:254–60. doi: 10.1210/jcem-54-2-254. [DOI] [PubMed] [Google Scholar]
- 4.Krotkiewski M, Bjorntorp P, Sjostrom L, Smith U. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest. 1983;72:1150–62. doi: 10.1172/JCI111040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conway JM, Yanovski SZ, Avila NA, Hubbard VS. Visceral adipose tissue differences in black and white women. Am J Clin Nutr. 1995;61:765–71. doi: 10.1093/ajcn/61.4.765. [DOI] [PubMed] [Google Scholar]
- 6.Albu JB, Murphy L, Frager DH, Johnson JA, Pi-Sunyer FX. Visceral fat and race-dependent health risks in obese nondiabetic premenopausal women. Diabetes. 1997;46:456–62. doi: 10.2337/diab.46.3.456. [DOI] [PubMed] [Google Scholar]
- 7.Lovejoy JC, de la Bretonne JA, Klemperer M, Tulley R. Abdominal fat distribution and metabolic risk factors: effects of race. Metabolism. 1996;45:1119–24. doi: 10.1016/s0026-0495(96)90011-6. [DOI] [PubMed] [Google Scholar]
- 8.Park YW, Allison D, Heymsfield S, Gallagher D. Larger amounts of visceral adipose tissue in Asian-Americans. Obes Res. 2001;9:381–7. doi: 10.1038/oby.2001.49. [DOI] [PubMed] [Google Scholar]
- 9.Hayashi T, Boyle E, Leonetti D, et al. Visceral adiposity and the prevalence of hypertension in Japanese Americans. Circulation. 2003;108:1718–23. doi: 10.1161/01.CIR.0000087597.59169.8D. [DOI] [PubMed] [Google Scholar]
- 10.Haffner SM, D'Agostino R, Saad MF, et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites. The Insulin Resistance Atherosclerosis Study. Diabetes. 1996;45:742–8. doi: 10.2337/diab.45.6.742. [DOI] [PubMed] [Google Scholar]
- 11.Bacha F, Saad R, Gungor N, Janosky J, Arslanian SA. Obesity, regional fat distribution, and syndrome X in obese black versus white adolescents: race differential in diabetogenic and atherogenic risk factors. J Clin Endocrinol Metab. 2003;88:2534–40. doi: 10.1210/jc.2002-021267. [DOI] [PubMed] [Google Scholar]
- 12.Goodpaster BH, Thaete FL, Kelley DE. Thigh adipose tissue distribution is associated with insulin resistance in obesity and in type 2 diabetes mellitus. Am J Clin Nutr. 2000;71:885–92. doi: 10.1093/ajcn/71.4.885. [DOI] [PubMed] [Google Scholar]
- 13.Goodpaster BH, Krishnaswami S, Resnick H, et al. Association between regional adipose tissue distribution and both type 2 diabetes and impaired glucose tolerance in elderly men and women. Diabetes Care. 2003;26:372–9. doi: 10.2337/diacare.26.2.372. [DOI] [PubMed] [Google Scholar]
- 14.Ryan AS, Nicklas BJ. Age-related changes in fat deposition in mid-thigh muscle in women: relationships with metabolic cardiovascular disease risk factors. Int J Obes Relat Metab Disord. 1999;23:126–32. doi: 10.1038/sj.ijo.0800777. [DOI] [PubMed] [Google Scholar]
- 15.Goodpaster BH, Carlson CL, Visser M, et al. Attenuation of skeletal muscle and strength in the elderly: the Health ABC Study. J Appl Physiol. 2001;90:2157–65. doi: 10.1152/jappl.2001.90.6.2157. [DOI] [PubMed] [Google Scholar]
- 16.Visser M, Kritchevsky SB, Goodpaster BH, et al. Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: the health, aging and body composition study. J Am Geriatr Soc. 2002;50:897–904. doi: 10.1046/j.1532-5415.2002.50217.x. [DOI] [PubMed] [Google Scholar]
- 17.Ross R. Magnetic resonance imaging provides new insights into the characterization of adipose and lean tissue distribution. Can J Clin Pharmacol. 1996;74:778–85. [PubMed] [Google Scholar]
- 18.Song MY, Ruts E, Kim J, Janumala I, Heymsfield S, Gallagher D. Sarcopenia and increased muscle adipose tissue infiltration in elderly African-American women. Am J Clin Nutr. 2004;79:874–80. doi: 10.1093/ajcn/79.5.874. [DOI] [PubMed] [Google Scholar]
- 19.Snyder WS, Cook MJ, Nasset ES, Karhausen LR, Howells GP, Tipton IH. Pergamon Press; Oxford, United Kingdom: 1975. Report of the Task Group on Reference Men. International Commission on radiological protection no. 23. [Google Scholar]
- 20.Pouliot MC, Despres JP, Lemieux S, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73:460–8. doi: 10.1016/0002-9149(94)90676-9. [DOI] [PubMed] [Google Scholar]
- 21.Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults: the National Health and Nutrition Examination Surveys, 1969 to 1991. JAMA. 1995;272:205–11. doi: 10.1001/jama.272.3.205. [DOI] [PubMed] [Google Scholar]
- 22.LaPorte RE, Matsushima M, Chang YF. Prevalence and incidence of insulin-dependent diabetes. In: Harris MI, Cowie CC, Stern MP, editors. Diabetes in America. NIH, NIDDK; Bethesda, MD: 1995. pp. 37–46. (NIH publication no. 95–1468). [Google Scholar]
- 23.Kenny SJ, Aubert RE, Geiss LS. Prevalence and incidence of non-insulin-dependent diabetes. In: Harris MI, Cowie CC, Stern MP, editors. Diabetes in America. NIH, NIDDK; Bethesda, MD: 1995. pp. 47–67. (NIH publication no. 95–1468). [Google Scholar]
- 24.Spence N, Heshka S, Kelley D, et al. Altered adipose tissue distribution in type II diabetic (T2DM) females. FASEB J. 2003;17:772.1. [Google Scholar]
- 25.Ryan AS, Nicklas BJ, Berman DM. Racial differences in insulin resistance and mid-thigh fat deposition in postmenopausal women. Obes Res. 2002;10:336–44. doi: 10.1038/oby.2002.47. [DOI] [PubMed] [Google Scholar]
- 26.Ortiz O, Russell M, Daley TL, et al. Differences in skeletal muscle and bone mineral mass between black and white females and their relevance to estimates of body composition. Am J Clin Nutr. 1992;55:1–6. doi: 10.1093/ajcn/55.1.8. [DOI] [PubMed] [Google Scholar]
- 27.Metheny E. Some differences in bodily proportions between American negro and white male college students as related to athletic performance. Res Q. 1939;10:41–53. [Google Scholar]
- 28.Janssen I, Fortier A, Hudson R, Ross R. Effects of an energy-restrictive diet with or without exercise on abdominal fat, intermuscular fat, and metabolic risk factors in obese women. Diabetes Care. 2002;25:431–8. doi: 10.2337/diacare.25.3.431. [DOI] [PubMed] [Google Scholar]
- 29.Goran MI, Nagy TR, Treuth MS, et al. Visceral fat in white and African American prepubertal children. Am J Clin Nutr. 1997;65:1703–8. doi: 10.1093/ajcn/65.6.1703. [DOI] [PubMed] [Google Scholar]
- 30.Hill JO, Sidney S, Lewis CE, Tolan K, Scherzinger AL, Stamm ER. Racial differences in amounts of visceral adipose tissue in young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Clin Nutr. 1999;69:381–7. doi: 10.1093/ajcn/69.3.381. [DOI] [PubMed] [Google Scholar]
- 31.Lovejoy JC, Smith SR, Rood JC. Comparison of regional fat distribution and health risk factors in middle-aged white and African American women: the Healthy Transitions Study. Obes Res. 2001;9:10–6. doi: 10.1038/oby.2001.2. [DOI] [PubMed] [Google Scholar]
- 32.Perry AC, Applegate EB, Jackson ML, et al. Racial differences in visceral adipose tissue but not anthropometric markers of health-related variables. J Appl Physiol. 2000;89:636–43. doi: 10.1152/jappl.2000.89.2.636. [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez Ballester MA, Zisserman AP, Brady M. Estimation of the partial volume effect in MRI. Med Image Anal. 2002;6:389–405. doi: 10.1016/s1361-8415(02)00061-0. [DOI] [PubMed] [Google Scholar]
- 34.Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol. 1998;85:115–22. doi: 10.1152/jappl.1998.85.1.115. [DOI] [PubMed] [Google Scholar]
- 35.Rosenberg NA, Pritchard JK, Weber JL, et al. Genetic structure of human populations. Science. 2002;298:2381–5. doi: 10.1126/science.1078311. [DOI] [PubMed] [Google Scholar]