Abstract
Psychosocial stress contributes to high blood pressure and subsequent cardiovascular morbidity and mortality. Previous controlled studies have associated decreasing stress with the Transcendental Meditation (TM) program with lower blood pressure. The objective of the present study was to evaluate, over the long term, all-cause and cause-specific mortality in older subjects who had high blood pressure and who participated in randomized controlled trials that included the TM program and other behavioral stress-decreasing interventions. Patient data were pooled from 2 published randomized controlled trials that compared TM, other behavioral interventions, and usual therapy for high blood pressure. There were 202 subjects, including 77 whites (mean age 81 years) and 125 African-American (mean age 66 years) men and women. In these studies, average baseline blood pressure was in the prehypertensive or stage I hypertension range. Follow-up of vital status and cause of death over a maximum of 18.8 years was determined from the National Death Index. Survival analysis was used to compare intervention groups on mortality rates after adjusting for study location. Mean follow-up was 7.6 ± 3.5 years. Compared with combined controls, the TM group showed a 23% decrease in the primary outcome of all-cause mortality after maximum follow-up (relative risk 0.77, p = 0.039). Secondary analyses showed a 30% decrease in the rate of cardiovascular mortality (relative risk 0.70, p = 0.045) and a 49% decrease in the rate of mortality due to cancer (relative risk 0.49, p = 0.16) in the TM group compared with combined controls. These results suggest that a specific stress-decreasing approach used in the prevention and control of high blood pressure, such as the TM program, may contribute to decreased mortality from all causes and cardiovascular disease in older subjects who have systemic hypertension.
Quantitative reviews of previous studies of reduction approaches to stress have either shown negative results or heterogeneity of effects on decreasing blood pressure depending on the experimental design and selection of specific technique.1,2 However, recent meta-analytic reviews have indicated that decreasing stress with the Transcendental Meditation (TM) program may be particularly effective in decreasing high blood pressure, psychosocial stress, morbidity, and mortality.3–5 Two previous randomized controlled trials of behavioral interventions associated the TM program with significantly decreased blood pressure after 3 months in independent samples of older white and African-American subjects.6–8 In addition, preliminary data suggested trends toward decreases in mortality in the TM group compared with active and usual-care controls in these trials.8–10 Therefore, the objective of the present study was to evaluate long-term all-cause and cause-specific mortality in older subjects who had high blood pressure and who participated in randomized controlled trials that included the TM program and other behavioral stress-reducing interventions.
METHODS
Clinical trials: Computerized and manual searches of the literature were used to locate published reports that met the following criteria: (1) randomized controlled trial design, (2) blood pressure as a primary outcome, and (3) studies that compared the effects of the TM program with those of other behavioral control interventions. Two trials met the search criteria and provided data for the present pooled analysis.6–8
The methods of the trial by Alexander et al8 have been described in detail. In brief, the 77 white participants (18% men and 82% women; mean age 81 ± 9.3 years) were residents of homes for the elderly in the Boston area. Baseline systolic blood pressure averaged 138 ± 15.9 mm Hg. Outcome measurements in the original study were cognitive functioning, mental health, and systolic blood pressure after 3 months and mortality rate after 3 years. Subjects were randomized to 4 treatment groups: a TM group (n = 21), a mindfulness training group (n = 23), a mental relaxation group (n = 22), and a usual-care control group (n = 11). In this study, the 3 active interventions (TM, mindfulness training, and mental relaxation) were matched to each other for teaching format, instructional time, home practice requirements (20 minutes 2 times a day), and expectancy of beneficial health outcomes. None of the interventions required other changes in lifestyle or personal beliefs.
The distinctive features of the 3 active treatments were as follows, The TM program was described as the principal mind-body technique of Maharishi Consciousness-Based Health Care, a comprehensive traditional system of natural medicine derived from the ancient Vedic tradition.11,12 The TM program was reported to include a simple, yet precise technique whereby the ordinary thinking process becomes quiescent and a unique psychophysiologic state of “restful alertness” appears to be gained.13 Details of the instructional protocol have been published.14 Mindfulness training, developed by Alexander et al,8 involved learning a guided attention technique to engage participants in novel and creative mental activities.8 The mental relaxation technique was designed to simulate generic features of the TM program, hypothesized by some researchers to be responsible for its relaxation effects.15 The mental relaxation technique required subjects to repeat silently to themselves familiar and brief mental stimuli (e.g., a phrase or verse) during the relaxation period. Home practice compliance rates after 3 months for each of the 3 active treatment groups were 80% for TM subjects who practiced regularly compared with 48% for the mindfulness training group and 47% for the mental relaxation group. Systolic blood pressure was significantly lower in the TM group than in the control group at 3 months.
Methods of the second trial have been published in detail.6,7 Briefly, this was a randomized controlled trial of community-dwelling older African-Americans (43% men and 57% women; mean age 67 ± 7.6 years) who had stage I and II hypertension (stages I and II; baseline blood pressure averaged 147/92 ± 13.2/8.7 mm Hg) and lived in Oakland, California. The 125 subjects were randomized to a TM group (n = 40), a progressive muscle relaxation group (PMR; n = 42), or a health education control group (n = 43). The 2 active interventions (TM and PMR) were matched for expectancy of benefits, teaching format, instructional time, and home practice (20 minutes 2 times a day). The TM program was taught according to the same standardized procedures as in the Alexander et al8 trial. The PMR technique followed previously standardized and validated procedures of Bernstein and Borkovic,16 based on a classic muscle relaxation program by Jacobson.17 This technique involved systematically relaxing the major muscle groups of the body with the goal of physical and mental relaxation. The health education control group received lifestyle modification information consistent with national guidelines.18 The education control intervention was designed to reflect usual-care community practice. Original outcomes in this study included systolic and diastolic blood pressures and other cardiovascular risk factors for cardiovascular disease (diet, exercise, weight, and substance use). The duration of the intervention was 3 months. Home practice regularity rates for TM and PMR after 3 months were 97% and 81%, respectively. There were no significant changes in diet, exercise, or blood pressure medications. Systolic and diastolic blood pressures were significantly lower in the TM group than in the PMR and education control groups.6,7
Determination of mortality: Data from 202 subjects from the 2 clinical trials were pooled.19 Vital status was obtained from the National Death Index (National Center for Health Statistics, Research Triangle Park, North Carolina), which provided an estimated accuracy of 93% to 98% in identifying vital status of patients.20 The database of subjects’ records was searched against the National Death Index database through December 31, 1998, the most recent year available as of autumn 2000. There were 101 mortalities. Causes of deaths were obtained by using the National Death Index Plus service, which provided coded causes of death according to the International Classification of Diseases, Ninth Revision. Cause-specific mortality was based on the underlying cause of death. Codes 401 to 438 were defined as cardiovascular diseases, and codes 140 to 239.9 were defined as cancer.
Statistical analysis: Survival analyses were performed on the pooled individual patient data from the 2 trials. This approach used meta-analysis of individual patient data.19 Survival time was measured starting from the date of randomization in the original studies. The primary outcome was all-cause mortality after completion of maximum follow-up. Secondary outcomes were mortality due to cardiovascular disease and cancer. Maximum follow-up periods were 18.8 years in trial 1 and 9.0 years in trial 2. In addition, secondary analyses were conducted of survival during 3 years (for comparison with the short-term published findings from trial 1) and during 10 years.
Statistical comparisons were made across the following treatment categories: the TM program (used in the 2 trials), “other active behavioral treatments” (mindfulness training and mental relaxation in trial 1 and PMR in trial 2), and the “usual-care” conditions (usual care in trial 1 and education control in trial 2). The usual-care groups constituted minimally controlled conditions for comparison with the 2 active treatment categories. Comparisons of the TM program with the other active behavioral therapies allowed control of nonspecific therapeutic effects, such as motivational factors and generalized effects of relaxation therapies (e.g., effects of sitting with eyes closed and novel deployment of attention). This was feasible because all active therapies were taught and practiced in structurally similar formats.
Survival analyses were performed with the SAS statistical package (SAS Institute, Cary, North Carolina). Data were checked for validity of the proportional hazards assumption.21 This was done using a time-dependent covariate, Z × ln(t), where Z is the indicator variable for TM, and t is the time since randomization, in Cox’s regression analysis of survival times. The time-dependent covariate was highly statistically significant in this analysis (p <0.0001), indicating that there was a significant violation of the proportional hazards assumption. Therefore, survival times of treatment groups were statistically compared using the generalized Wilcoxon’s test that has been recommended for analysis of nonproportional hazards.21 Stratification on study location was used to adjust for demographic differences between studies. The effect of treatment on survival was quantified as relative risk that was estimated from Cox’s regression analysis of survival times. Two-sided p values ≤0.05 were considered statistically significant. Survival analyses were conducted with “intention-to-treat” and “on-trial” principles. Subjects who were randomly allocated and completed post-testing at 3 months were included in the on-trial analyses. Missing data were handled in the intention-to-treat analysis by the method of multiple imputation.22
RESULTS
For all subjects in the pooled study, mean age ± SD was 72.0 ± 10.6 years, 67% were women, and systolic blood pressure was 144 ± 15.6 mm Hg. Mean follow-up times were 8.45 ± 4.83 years in study 1, 7.13 ± 2.15 years in study 2, and 7.63 ± 3.48 years for studies 1 and 2. Table 1 presents the number of all-cause and disease-specific mortality events in each study for the on-trial analysis. Table 2 presents the number of mortality events for the intention-to-treat analysis. Table 3 presents the relative risks and significance levels for the primary and secondary outcomes of cardiovascular disease and cancer mortality for each study and for the 2 studies combined. As presented in Table 3, the relative risk of all-cause mortality for the TM group compared with combined control groups was 0.77 (p = 0.039; Figure 1). For mortality due to cardiovascular disease, the relative risk was 0.70 (p = 0.045); for mortality due to cancer, the relative risk was 0.51 (p = 0.153). The intention-to-treat results showed a similar pattern. That is, for the 2 trials pooled, the relative risks were 0.75 (p = 0.062) for the TM group compared with combined control groups for all-cause mortality, 0.62 (p = 0.025) for cardiovascular mortality, and 0.53 (p = 0.190) for cancer mortality.
TABLE 1.
Numbers of Deaths by Treatment Group in Each Clinical Trial*
| No. of deaths
|
|||||
|---|---|---|---|---|---|
| Clinical Trial | Treatment Group | No. of Subjects | All Causes | Cardiovascular Diseases | Cancers |
| Boston (Alexander et al8) | TM | 20 | 20 | 11 | 1 |
| Mindfulness | 20 | 20 | 10 | 4 | |
| Mental relaxation | 22 | 21 | 12 | 4 | |
| Usual care | 11 | 10 | 4 | 1 | |
| Oakland (Schneider et al6) | TM | 36 | 8 | 1 | 4 |
| PMR | 37 | 12 | 4 | 5 | |
| Health education (control) | 36 | 10 | 6 | 4 | |
For subjects included in on-trial analyses.
TABLE 2.
Numbers of Deaths by Treatment Group in Each Clinical Trial*
| No. of deaths
|
|||||
|---|---|---|---|---|---|
| Clinical Trial | Treatment Group | No. of Subjects | All Causes | Cardiovascular Diseases | Cancers |
| Boston (Alexander et al8) | TM | 21 | 20 | 11 | 1 |
| Mindfulness | 23 | 22 | 12 | 4 | |
| Mental relaxation | 22 | 21 | 12 | 4 | |
| Usual care | 11 | 10 | 4 | 1 | |
| Oakland (Schneider et al6) | TM | 41 | 9 | 1 | 4 |
| PMR | 42 | 12 | 4 | 5 | |
| Health education (control) | 42 | 11 | 7 | 4 | |
For subjects included in intention-to-treat analyses.
TABLE 3.
Effects of Interventions on Mortality in the Pooled Clinical Trials
| Relative Risk
|
|||||
|---|---|---|---|---|---|
| Cause of Death | Statistical Comparison | Boston8 | Oakland6 | 2 Trials | Significance (2 trials) |
| All cause | TM vs usual care | 1.13 | 0.60 | 0.89 | 0.21 |
| TM vs other active therapy | 0.79 | 0.58 | 0.73 | 0.03 | |
| Other active therapy vs usual care | 1.33 | 1.16 | 1.26 | 0.43 | |
| TM vs combined controls | 0.85 | 0.61 | 0.77 | 0.04 | |
| Cardiovascular disease | TM vs usual care | 1.65 | 0.16 | 0.82 | 0.10 |
| TM vs other active therapy | 0.80 | 0.23 | 0.68 | 0.06 | |
| Other active therapy vs usual care | 1.79 | 0.69 | 1.23 | 0.74 | |
| TM vs combined controls | 0.92 | 0.19 | 0.70 | 0.05 | |
| Cancer | TM vs usual care | 0.54 | 0.69 | 0.65 | 0.47 |
| TM vs other active therapy | 0.20 | 0.69 | 0.44 | 0.09 | |
| Other active therapy vs usual care | 2.49 | 1.25 | 1.56 | 0.52 | |
| TM vs combined controls | 0.24 | 0.73 | 0.51 | 0.15 | |
FIGURE 1.
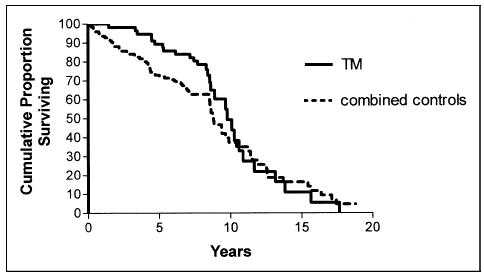
Kaplan-Meier survival curves for all-cause mortality for subjects who completed post-testing in the original studies (relative risk 0.77, p = 0.04).
To further evaluate the effects of stress-decreasing intervention on intermediate time points of survival, analyses were conducted for 3 and 10 years of follow-up. The results of the TM versus combined controls comparison for all-cause mortality showed relative risks of 0.11 (p = 0.013) at 3 years and 0.60 (p = 0.025) at 10 years of follow-up. Intention-to-treat analyses showed similar results, i.e., relative risks were 0.21 (p = 0.046) at 3 years and 0.62 (p = 0.044) at 10 years.
DISCUSSION
The results of this retrospective long-term follow-up of 2 randomized controlled trials of decreasing stress and high blood pressure in older subjects suggest that a selected behavioral approach, the TM program, is associated with significantly lower mortality rates compared with other behavioral interventions and usual care. The decreases in risk were 23% for all-cause mortality and 30% for cardiovascular mortality, and there was a trend for cancer mortality over the 7.6-year mean, 18.8-year maximum follow-up period. The results of intention-to-treat analyses were similar to those of on-trial analyses. There were similar risk decreases for the 2 independent study samples: elderly white subjects who had prehypertension and who resided in Boston, Massachusetts, and older African-Americans who had stage I and II hypertension and lived in Oakland, California.
This is the first pooled analysis of randomized controlled trials on long-term effects of nonpharmacologic interventions for hypertension on mortality. Although the sample of 202 African-American and white men and women in the present study was relatively modest, these preliminary results suggest that an effective stress-reducing intervention may decrease mortality rates for all causes and cardiovascular disease.
A meta-analysis of pooled clinical trials of pharmacologic antihypertensive therapy indicated an average decrease of 12 to 13 mm Hg in systolic blood pressure over 4 years.23 This was associated with a 13% decrease in all-cause mortality and a 25% decrease in cardiovascular mortality.24 The short-term follow-up of blood pressure changes in the 2 trials of decreasing stress included in the present analysis associated the practice of TM with a decrease of 10 to 11 mm Hg in systolic blood pressure. Diastolic blood pressure was measured only in study 2, and there the decrease averaged 6 mm Hg. Whether these or other decreases in blood pressure were maintained during the 7.6 years of average follow-up of survival is unknown, because in the present retrospective analysis only mortality data from national databases were collected. However, the 23% decrease in the primary outcome of all-cause mortality and 30% decrease in cardiovascular mortality may be considered somewhat similar to decreased risks reported with antihypertensive therapy in middle-aged and older adults who have hypertension.23,24 Larger clinical trials that are prospectively designed to assess blood pressure, treatment compliance, mechanistic variables, and mortality over the long-term are required to more definitively evaluate these effects.
Another relevant consideration when comparing the effectiveness and utility of interventions for hypertension is the significant rate of adverse effects associated with antihypertensive drugs.25,26 Previous studies on physiologic outcomes and quality-of-life effects of the TM program reported a range of improvements in physical and psychological health in adults generally and in older subjects specifically.12,27,28 These and the present effects on mortality are consistent with theoretical mechanisms of action of the TM program, which suggest a diverse yet integrated effect on mind–body health.11,29
In conclusion, the present findings suggest that nonpharmacologic decrease of stress with the TM program, in addition to usual care, may be associated with long-term decreases in mortality in older populations that have high blood pressure.
Acknowledgments
The investigators are grateful to William Sheppard, PhD, and Marcelino Aguilar-Cervantes, MS, for technical assistance and editorial consultation.
Footnotes
This study was supported in part by a Specialized Center of Research grant from the National Institutes of Health, Bethesda, Maryland (Grant 1P50AT00082 from the National Center for Complementary and Alternative Medicine).
References
- 1.Eisenberg DM, Delbanco TL, Berkey CS, Kaptchuk TJ, Kupelnick B, Kuhl J, Chalmers T. Cognitive behavioral techniques for hypertension: are they effective? Ann Intern Med. 1993;118:964–972. doi: 10.7326/0003-4819-118-12-199306150-00009. [DOI] [PubMed] [Google Scholar]
- 2.Spence J, Barnett P, Linden W, Ramsden V, Taenzer P. Lifestyle modifications to prevent and control hypertension. 7 Recommendations on stress management. Can Med Assoc J. 1999;160:46–50. [PMC free article] [PubMed] [Google Scholar]
- 3.Orme-Johnson D, Walton K. All approaches to preventing or reversing effects of stress are not the same. Am J Health Promot. 1998;12:297–299. doi: 10.4278/0890-1171-12.5.297. [DOI] [PubMed] [Google Scholar]
- 4.Lin MC, Nahin R, Gershwin ME, Longhurst JC, Wu KK. State of complementary and alternative medicine in cardiovascular, lung, and blood research: executive summary of a workshop. Circulation. 2001;103:2038–2041. doi: 10.1161/01.cir.103.16.2038. [DOI] [PubMed] [Google Scholar]
- 5.Alexander CN, Robinson P, Orme-Johnson DW, Schneider RH, Walton KG. Effects of Transcendental Meditation compared to other methods of relaxation and meditation in reducing risk factors, morbidity and mortality. Homeostasis. 1994;35:243–264. [Google Scholar]
- 6.Schneider RH, Staggers F, Alexander C, Sheppard W, Rainforth M, Kondwani K, Smith S, King CG. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 7.Alexander CN, Schneider R, Staggers F, Sheppard W, Clayborne M, Rainforth M, Salerno J, Kondwani K, Smith S, Walton K, Egan B. A trial of stress reduction for hypertension in older African Americans (part II): sex and risk factor subgroup analysis. Hypertension. 1996;28:228–237. doi: 10.1161/01.hyp.28.2.228. [DOI] [PubMed] [Google Scholar]
- 8.Alexander CN, Langer EJ, Newman RI, Chandler HM, Davies JL. Transcendental Meditation, mindfulness, and longevity: an experimental study with the elderly. J Pers Social Psychol. 1989;57:950–964. doi: 10.1037//0022-3514.57.6.950. [DOI] [PubMed] [Google Scholar]
- 9.Barnes VA, Schneider RH, Alexander CN, Rainforth M, Staggers F, Salerno J. Impact of transcendental meditation on mortality in older African Americans—eight year follow-up. J Social Behav Pers. 2005;17:201–216. [Google Scholar]
- 10.Alexander CN, Barnes VA, Schneider RH, Langer EJ, Newman RI, Chandler HM, Davies JL, Rainforth M. A randomized controlled trial of stress reduction on cardiovascular and all-cause mortality in the elderly: results of 8 and 15 year follow-ups. Circulation. 1996;93:P19. [Google Scholar]
- 11.Nader T. Human Physiology: Expression of Veda and the Vedic Literature. Vlodrop, Holland: Maharishi Vedic University, 2000.
- 12.Schneider RH, Alexander CN, Salerno J, Robinson D, Fields J, Nidich S. Disease prevention and health promotion in the aging with a traditional system of natural medicine: Maharishi Vedic Medicine. J Aging Health. 2002;14:57–78. doi: 10.1177/089826430201400104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jevning R, Wallace RK, Biedebach M. The physiology of meditation: a review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–424. doi: 10.1016/s0149-7634(05)80210-6. [DOI] [PubMed] [Google Scholar]
- 14.Roth R. Maharishi Mahesh Yogi’s Transcendental Meditation. Washington, DC: Primus, 2002:90–102.
- 15.Smith JC. Therapeutic effects of transcendental meditation with controls for expectation of relief and daily sitting. J Consult Clin Psychol. 1976;44:630–637. doi: 10.1037//0022-006x.44.4.630. [DOI] [PubMed] [Google Scholar]
- 16.Bernstein DA, Borkovic TD. Progressive Relaxation Training: A Manual for the Helping Profession. Chicago: Illinois University Press, 1973.
- 17.Jacobson E. Progressive Relaxation. Chicago: University of Chicago Press, 1992:28–100.
- 18.Chobanian A, Bakris G, Black H National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 19.Stewart LA, Clarke M. Practical methodology of meta-analysis using updated individual patient data. Stat Med. 1995;14:2057–2079. doi: 10.1002/sim.4780141902. [DOI] [PubMed] [Google Scholar]
- 20.Edlavitch SA, Baxter J. Comparability of mortality follow-up before and after the National Death Index. Am J Epidemiol. 1988;127:1164–1178. doi: 10.1093/oxfordjournals.aje.a114910. [DOI] [PubMed] [Google Scholar]
- 21.Collett D. Modelling Survival Data in Medical Research. London: Chapman & Hall, 1994.
- 22.Little RJA, Rubin DB. Statistical Analysis With Missing Data. New York: Wiley, 1987.
- 23.Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, Lemaitre RN, Wagner EH, Furberg CD. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA. 1997;277:739–745. [PubMed] [Google Scholar]
- 24.Staessen J, Gasowski J, Wang J, Thijs L, Den Hond E, Boissel JP, Coope J, Ekborm T, Gueyffier F, Liv L, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet. 2000;355:865–872. doi: 10.1016/s0140-6736(99)07330-4. [DOI] [PubMed] [Google Scholar]
- 25.Hansson L, Zanchetti A, Carruthers S. Effects of intensive blood pressure lowering and low-dose aspirin in patients with hypertension: principle results of the Hypertension Optimal Treatment (HOT) randomized trial. HOT study group. Lancet. 1998;351:1755–1762. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 26.Cutler J. Calcium channel blockers for hypertension—uncertainty continues. N Engl J Med. 1998;338:679–680. doi: 10.1056/NEJM199803053381009. [DOI] [PubMed] [Google Scholar]
- 27.Walton KG, Schneider RH, Nidich SI, Salerno JW, Nordstrom CK, Bairey-Merz CN. Psychosocial stress and cardiovascular disease 2: effectiveness of the transcendental meditation technique in treatment and prevention. Behav Med. 2002;28:106–123. doi: 10.1080/08964280209596049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walton K, Schneider R, Nidich S. Review of controlled research on the transcendental meditation program and cardiovascular disease—risk factors, morbidity and mortality. Cardiol Rev. 2004;12:262–266. doi: 10.1097/01.crd.0000113021.96119.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nader T, Rothenberg S, Averbach R, Charles B, Fields JZ, Schneider RH. Improvements in chronic diseases with a comprehensive natural medicine approach: a review and case series. Behav Med. 2000;26:34–46. doi: 10.1080/08964280009595751. [DOI] [PMC free article] [PubMed] [Google Scholar]


