Abstract
Objectives. Homeless individuals experience high rates of physical and mental illness, increased mortality, and frequent hospitalizations. Respite care provides homeless individuals with housing and services allowing more complete recovery from illnesses and stabilization of chronic conditions.
Methods. We investigated respite care’s impact on 225 hospitalized homeless adults consecutively referred from an urban public hospital during a 26-month period. The cohort was separated into 2 groups: (1) patients referred and accepted into the respite center and (2) patients referred but denied admission because beds were unavailable. All patients met the center’s predefined eligibility criteria. Main outcome measures were inpatient days, emergency department visits, and outpatient clinic visits.
Results. The 2 groups had similar demographic characteristics, admitting diagnoses, and patterns of medical care use at baseline. During 12 months of follow-up, the respite care group required fewer hospital days than the usual care group (3.7 vs 8.3 days; P=.002), with no differences in emergency department or outpatient clinic visits. Individuals with HIV/AIDS experienced the greatest reduction in hospital days.
Conclusions. Respite care after hospital discharge reduces homeless patients’ future hospitalizations.
Homeless individuals suffer from high rates of physical and mental illness1–3 and experience mortality rates several times higher than the general population.4–7 Although homeless adults are hospitalized more frequently (and require longer inpatient stays) than a comparable sample of housed adults,8–13 their homelessness may diminish the long-term effectiveness of their hospital care. Back on the streets after hospital discharge, competing priorities (obtaining food, clothing, and shelter) and substance use may divert their attention from compliance with medications, other physician instructions, and follow-up appointments.14,15
Traditional overnight shelters require homeless people to vacate the shelter each morning and live on the street during the day before returning to the shelter at night. In contrast, respite care provides around-the-clock room and board to homeless patients discharged from an emergency room or hospital, encouraging them to comply with posthospital rehabilitation. Many respite services also provide some form of on-site medical care, a range of social services, and transportation assistance to facilitate continuity of care.16 Despite recent growth in respite service in the United States, no published studies have explored the impact of respite services on health outcomes.
METHODS
Our study was conducted between October 1, 1998, and December 31, 2000, at Cook County Hospital, a 700-bed urban public hospital, and Interfaith House, a 64-bed respite care provider in Chicago, Ill. During this period, Interfaith House was the only provider of respite care services in Chicago, and Cook County Hospital was its largest referral source, accounting for 40% of all referrals. Interfaith House, like most respite facilities in the United States, provides its clients with a complex bundle of services. At Interfaith House, these services include interim housing, food, acute care health services by volunteer health providers, facilities to organize medications, substance abuse counseling, case management, and referrals to permanent housing. Skilled nursing is not provided, and referred patients who need these services are not accepted. Interfaith House has been unable to meet the demand for its services (referrals have exceeded bed capacity) since October 1998. This was chosen as the starting date for the study in order to compare health outcomes for patients accepted into respite care with those refused respite care because of lack of available beds.
All homeless adult inpatients at the hospital referred for respite care during the study period were identified by retrospective review of computerized administrative data and medical records. Patients eligible for respite care (according to Interfaith House’s admission criteria) must have an identified acute illness, be able to perform activities of daily living with minimal assistance, and be able to function in a group living environment that is drug- and alcohol-free. Patients who met these eligibility criteria when a respite care bed was available during the study period comprised the respite care group. Patients who met these eligibility criteria when respite care beds were unavailable comprised the usual care group.
Study outcomes included hospital days, emergency department visits, outpatient clinic visits, and mortality during the 1 year following patients’ index hospitalization. Total hospitalizations was a secondary outcome. Hospital days, rather than total hospitalizations, was chosen as the primary outcome for hospitals because it better reflects the economic impact on the public hospital system, where much of the care for homeless patients is not reimbursed. Mortality was assessed by searching the Social Security death index for all study patients, first using the patient’s Social Security number, and then the patient’s name and date of birth. A patient was considered deceased if either the Social Security number or the full name and date of birth matched exactly. Hospital days, emergency department visits, and outpatient clinic visits were measured by analyzing administrative databases of the Cook County Bureau of Health Services, which includes, in addition to Cook County Hospital and its emergency department, the 2 other publicly funded hospitals in Cook County and the Bureau’s 30 community-based primary care clinics (approximately 1 million annual outpatient visits). The accuracy of study patients’ outpatient and emergency department visits recorded in the administrative databases was checked by reviewing patients’ medical records to exclude “visits” where patients registered but left without being seen (because of long waits or other reasons). Patients who receive care within the Cook County Bureau of Health Services may seek care outside its system; however, most rely on the Bureau for all medical services because it is the only institution in the area that provides primary and tertiary health care regardless of patients’ insurance status or ability to pay.
The average cost of respite services during the study period was determined by dividing the total annual budget of the respite center by the total number of patient-days that the center provided per year.
Data Analysis
Baseline characteristics were compared using the t test for normally distributed variables and the χ2 test for categorical variables; the Mann–Whitney test was used for continuous variables that were not normally distributed (health care services in the previous 6 months). We used general linear models to compare groups on mean number of inpatient days, emergency department visits, and outpatient clinic visits during the 12-month follow-up period, while controlling for age, gender, race, reason for index hospitalization, and use of health services during the 6 months before respite care referral. The distributions of the 3 outcome variables were skewed; therefore, the confidence intervals were calculated using 1000 bootstrap simulations. We also tested the prespecified hypothesis that the type of illness prompting respite care referral might modify the effect of respite care, and explored other potential 2-way interactions. P values and confidence intervals were not adjusted for multiple comparisons. All analyses were performed using SPSS, version 10 (SPSS, Inc., Chicago, IL) and Stata, version 8 (Stata Software Corp., College Station, TX).
Members of the respite care group who left the respite facility in the first hours or days after transfer were included in the respite group. People who leave respite early are often those who have difficulty adjusting to the structure or sobriety requirements of the institution. These individuals may be systematically different than those who stay. Some individuals in the usual care group, who were turned away because of a lack of service capacity, would likely have also left early if they had been given the chance to enter the respite center. Our analysis would be biased if “people who leave respite centers early” were excluded from the respite care group but were still included in the usual care group. Because the usual care participants who would have left early if given the opportunity to experience respite care can not be identified and excluded, the most conservative analysis of the data includes all individuals in the group to which they were assigned at the time of referral. This intention-to-treat analysis tends to underestimate the efficacy of respite care.
RESULTS
During the study period, 225 homeless patients who met all the eligibility requirements of the respite center were referred by the Cook County Bureau of Health Services. A total of 161 were accepted into respite care (respite care group), and 64 were denied admission to respite care because of a lack of available beds, and were discharged from the hospital to overnight shelters, other housing arrangements, or the street (usual care group).
There were statistically significant differences between the respite care and usual care groups in terms of race. The usual care group had more Latino patients, and the respite care group had more African American and White patients. The respite care group also had more emergency department visits during the 6 months before referral to respite (1.5 vs 0.9 visits; P = .02). However, there were no significant differences between the respite care and control groups in age, gender, diagnosis, or utilization of inpatient and outpatient health services during a 6-month period before respite care referral (Table 1 ▶). The 3 most common admitting diagnoses were trauma, HIV/AIDS, and non-HIV infections. During the 6 months before the referral to respite, the average patient required 5 inpatient days, 1 emergency department visit, and 2 outpatient clinic appointments, in addition to the hospitalization that lead to the respite care referral.
TABLE 1—
Baseline Demographic and Clinical Characteristics by Group: 1998–2000
| Characteristic | Respite Care Group (n = 161) | Usual Care Groupa (n = 64) | P |
| Mean age, y (SD) | 43 (9) | 44 (10) | .54 |
| Race n (%) | .05 | ||
| African American | 120 (75) | 43 (67) | |
| White | 30 (19) | 10 (16) | |
| Latino | 9 (6) | 10 (16) | |
| Other | 2 (1) | 1 (2) | |
| Female Gender, n (%) | 36 (22) | 12 (19) | .59 |
| Diagnosis, n (%) | .07 | ||
| Trauma | 64 (40) | 15 (23) | |
| HIV44 (27) | 18 (28) | ||
| Non-HIV Infection | 20 (12) | 9 (14) | |
| Other Illness | 33 (21) | 22 (34) | |
| Use of health services during the 6 months before index hospitalization | |||
| Inpatient days, mean, median (25th, 75th percentile) | 5.8, 2 (0, 8) | 5.3, 0 (0, 7) | .23 |
| Emergency department visits, mean, median (25th, 75th percentile) | 1.5, 1 (0, 2) | 0.9, 0 (0, 1) | .02 |
| Outpatient clinic visits, mean, median (25th, 75th percentile) | 1.8, 0 (0, 2) | 1.8, 0 (0, 1) | .42 |
aPatients in the usual care group were eligible and referred for but were denied respite care because beds were not available at the respite care center.
When health service use was analyzed for the 12-month period after hospital discharge, the respite care group utilized 58% fewer inpatient days (3.4 vs 8.1 days; P = .002), and had a 49% reduction in hospital admissions (P = .002) after adjusting for gender, race, age, diagnosis, and previous utilization of health services (Table 2 ▶ and Figure 1 ▶). Overall, 61% of usual care and 28% of respite care members were hospitalized at least once during the following year. There were no statistical differences found between each group’s use of the emergency department and outpatient clinics. There were no deaths found in either group during the first 12 months of follow-up.
TABLE 2—
Number of Inpatient Days, Emergency Department Visits, and Outpatient Clinic Visits by Group During the 12-Month Follow-Up Period After Respite Care Referrala: 1998–2000
| Respite Care Group (n = 161),Mean, 95% CI | Usual Care Groupa (n = 64),Mean, 95% CI | P | |
| Inpatient days | 3.4 (2.3, 4.7) | 8.1 (5.1, 11.9) | .002 |
| Emergency department visits | 1.4 (0.9, 1.8) | 2.2 (1.2, 3.6) | .09 |
| Outpatient clinic visits | 6.7 (5.3, 8.2) | 6.0 (4.1, 8.0) | .60 |
Note. CI = confidence interval. a Patients in the usual care group were referred to but were denied respite care because beds were not available at the respite care center. General linear models were used to adjust for age, race, gender, reason for index hospitalization, and use of health services during the 6 months before referral to respite care.
FIGURE 1—
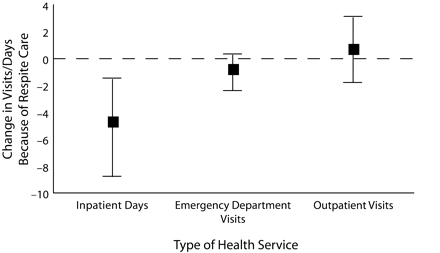
Difference between respite care group and usual care group in mean inpatient days, emergency department visits, and outpatient clinic visits (with 95% confidence intervals) during the 12-month follow-up period.
Note. Differences less than zero indicate fewer days or visits in the respite care group. Confidence intervals were calculated using 1000 bootstrap simulations, because of the non-normal distributions of the outcome variables.
There was a significant interaction between the reason for the index hospitalization and group (respite care and usual care; P = .036). Subsequent subgroup analysis showed that patients in the respite care group whose index admission was for HIV/AIDS had the greatest absolute reduction in inpatient days when compared with those with the same reason for the index admission in the usual care group (6.5 vs 17.8 days; P = .01) (Figure 2 ▶).
FIGURE 2—
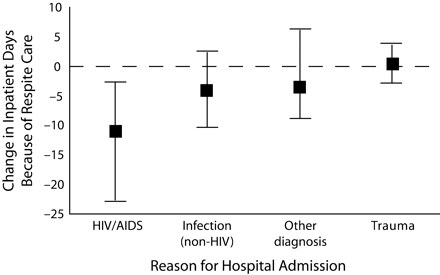
Difference in mean inpatient days between the respite care group and usual care group during the 12-month follow-up period (with 95% confidence intervals), by reason for index hospitalization.
Note. The interaction between group (respite care and usual care) and reason for admission at index hospitalization was significant in the multivariable model (P = .04). Values less than zero indicate fewer inpatient days in the Respite Care group.
The average length of stay in respite for the respite care group was 42 days, and the cost of providing respite services during the study period was $79 per day. Therefore, the average cost of respite per hospital-day avoided was $706.
DISCUSSION
Respite care significantly reduced homeless patients’ utilization of inpatient services when compared with usual care. This suggests that respite care can improve health outcomes and reduce health care costs for a defined subset of homeless people. The $706 average cost of respite care per hospital-day avoided compares favorably with the $1500 per day in hospital costs estimated by the Agency for Healthcare Research and Quality for the United States during this time period.17 Emergency department usage was 36% lower in the respite care group, although the result did not reach statistical significance with the number of participants analyzed. The expected increase in outpatient clinic use among homeless people served by respite may have been diminished by medical services received on site at the respite center.
Further studies are needed to confirm and extend these findings for three reasons. First, our study results cannot be generalized to all homeless people with acute medical illnesses or to all respite care centers. For example, many homeless adults suffer from severe psychiatric symptoms incompatible with a group living situation, or cannot agree to the drug and alcohol requirements of the respite center studied, rendering them ineligible for referral. Even in our selected study population, outcomes varied considerably by the reason for the index hospitalization and improved by the greatest degree for the most vulnerable adults: those with HIV. Larger studies of various types of respite care interventions are needed for different subsets of this population.
Second, the internal validity of our findings can be challenged because we did not measure health care utilization outside the Cook County Bureau of Health Services. Thus, we cannot exclude the possibility that some study patients received care at other institutions. This seems unlikely, because the respite care center in our study requires that each referring hospital provide continuity of care for all referred patients. Indeed, for both of our study groups, visits to our outpatient facilities (emergency department and clinics) increased when compared with the baseline period. Nevertheless, future studies should capture all health care utilization, including data reported by patients themselves.
Finally, a randomized control trial is needed. Although the available demographic data, clinical variables, and baseline utilization data were similar in our respite care and usual care study groups, it is possible that unmeasured variables, including differential rates of substance use or psychiatric illness, may have confounded our results. Some might argue that a randomized trial would be unethical, given the obvious humanitarian virtues of respite care. But a randomized trial would be no less ethical than the current status quo in the United States, where respite care is available only to some, not all, homeless people. Now is the time for such a trial, given the results of the present study, the financial distress of many US hospitals, and the unmet needs of our country’s homeless people.
Acknowledgments
David Buchanan was supported in part by a Physician Advocacy Fellowship from the Open Society Institute during the writing of this article.
The authors acknowledge the contributions of Art Evans, who performed the statistical analyses and revised the manuscript content, and Brendan Reilly, who assisted with revisions.
Human Participant Protection This study was approved by the institutional review board of John Stroger Hospital of Cook County.
Peer Reviewed
Contributors D. Buchanan led the writing. He and B. Doblin originated the study and supervised all aspects of its implementation. T. Sai and P. Garcia assisted with the data collection and reviewed drafts of the article.
References
- 1.Breakey WR, Fischer PJ, Kramer M, et al. Health and mental health problems of homeless men and women in Baltimore. JAMA. 1989;262:1352–1357. [PubMed] [Google Scholar]
- 2.Fischer PJ, Breakey WR. The epidemiology of alcohol, drug, and mental disorders among homeless persons. Am Psychol. 1991;46:1115–1128. [DOI] [PubMed] [Google Scholar]
- 3.Koegel P, Burnam MA, Farr RK. The prevalence of specific psychiatrics disorders among homeless individuals in the inner city of Los Angeles. Arch Gen Psychiatry. 1988;45:1085–1092. [DOI] [PubMed] [Google Scholar]
- 4.Hwang SW. Mortality among men using homeless shelters in, Ontario. JAMA. 2000;283: 2152–2157. [DOI] [PubMed] [Google Scholar]
- 5.Barrow SM, Herman DB, Cordova P, Struening EL. Mortality among homeless shelter residents in New York City. Am J Public Health. 1999;89:529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hibbs JR, Benner L, Klugman L. et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331:304–309. [DOI] [PubMed] [Google Scholar]
- 7.Hwang SW, Lebow JM, Bierer MF, O’Connell JJ, Orav EJ, Brennan TA. Risk factors for death in homeless adults in Boston. Arch Intern Med. 1998;158: 1454–1460. [DOI] [PubMed] [Google Scholar]
- 8.Martell JV, Seitz RS, Harada JK, Kobayashi J, Sasaki VK, Wong C. Hospitalization in an urban homeless population: the Honolulu Urban Homeless Project. Ann Intern Med. 1992;116:299–303. [DOI] [PubMed] [Google Scholar]
- 9.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalizations costs associated with homelessness in New York City. N Engl J Med. 1998;338:1734–1740. [DOI] [PubMed] [Google Scholar]
- 10.Smith MY, Rapkin BD, Winkel G, Springer C, Chhabra R, Feldman IS. Housing status and health care service utilization among low-income persons with HIV/AIDS. J Gen Intern Med. 2000;15:731–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. [DOI] [PubMed] [Google Scholar]
- 12.Han B, Wells BL, Taylor AM. Use of the health care for the homeless program services and other health care services in homeless adults. J Health Care Poor Underserved. 2003;14:87–99. [PubMed] [Google Scholar]
- 13.Han B, Wells B. Inappropriate emergency department visits and use of the health care for the homeless program services by homeless adults in the northeastern United States. J Public Health Manag Pract. 2003;9: 530–537. [DOI] [PubMed] [Google Scholar]
- 14.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87:217–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masson CL, Sorensen JL, Phibbs CS, Okin RL. Predictors of medical service utilization among individuals with co-occuring HIV infection and substance abuse disorders. AIDS Care. 2004;16:217–220. [DOI] [PubMed] [Google Scholar]
- 16.Hanson N. Survey of Homeless Health Care Respite Providers. Paper presented at: the Respite Care Provider National Meeting, Fort Lauderdale, FL; June, 2002.
- 17.Merrill CT, Elixhauser A. Hospitalization in the United States, 2002. Rockville, MD: Agency on Health-care Research and Quality, 2005. HCUP Fact Book No. 6. AHRQ Publication No. 05–0056.


