Abstract
Objective. We sought to determine the frequency and costs of hospitalization and to assess possible racial/ethnic disparities in a large cohort of low-income patients with diabetes who had received primary care at municipal health clinics.
Methods. Administrative data from Philadelphia Health Care Centers were linked with discharge data from Pennsylvania hospitals for March 1993 through December 2001. We tested differences in hospitalization rates and mean hospital charges by age, gender, and race/ethnicity.
Results. A total of 18 800 patients with diabetes experienced 30 528 hospital admissions, for a hospitalization rate of 0.35 per person-year. Rates rose with age and with the interaction of male gender and age. Rates for non-Hispanic Whites were higher than those for African Americans, whereas those for Hispanics, Asian Americans, and “others” were lower. Patients who were hospitalized at least 5 times made up 10.5% of the study population and accounted for 64% of hospital admissions and hospital charges in this cohort.
Conclusions. Hospitalization rates for this low-income cohort with access to primary care and pharmacy services were comparable to those of other diabetic patient populations, suggesting that reducing financial barriers to care may have benefited these patients. A subgroup of patients with multiple hospitalizations accounted for the majority of hospital admissions.
Diabetes is one of the largest and fastest-growing causes of chronic disease mortality, morbidity, and disability in the United States. An estimated 18.2 million Americans had diabetes in 2002.1 The number of diagnosed persons with diabetes has been projected to increase to almost 20 million by 2025.2 The prevalence of diabetes has increased in all population groups, with the largest increases noted in people aged younger than 50 years.1 In the United States, diabetes disproportionately affects African Americans and other racial/ethnic minorities and Americans of lower socioeconomic status regardless of race.1,3–5
Diabetes is a treatable disease, and the benefits of appropriate treatment have been demonstrated in major clinical trials.6–8 Nonetheless, surveys in a variety of populations and health care systems have found that most diabetic patients are not receiving optimal care or achieving recommended levels of glycemic control.9–12
There is abundant evidence that African Americans and other minority patients and patients of lower socioeconomic status receive less intensive and poorer quality care across a number of major conditions13–15 and experience poorer health status and health outcomes. However, we have limited information on possible disparities in outcomes among individuals with diabetes.16–21
Hospitalization is both an adverse health event and a marker for serious health complications, and is often predictive of disability.22 Persons with diabetes are admitted to hospitals substantially more frequently, and experience longer hospital stays, than nondiabetic individuals.12,16 Diabetes is considered an ambulatory care–sensitive condition, and many hospitalizations are potentially preventable.23 We sought to determine the frequency and costs of hospital admission in a large, unselected multiracial cohort of predominantly low-income patients with diabetes who had received primary care at municipal health clinics in Philadelphia over a period of 106 months, and to examine possible racial/ethnic disparities within this cohort.
METHODS
Administrative data from the Philadelphia Health Care Centers were linked with hospital discharge data from the Pennsylvania Health Care Cost Containment Council for a period from 1993 to 2001. The Health Care Center system provides free services to uninsured and underinsured patients—no individual patient is billed for any Health Care Center services, including pharmaceuticals.
Data on outpatient care were extracted from the management information system maintained by the Philadelphia Department of Public Health for the 9 Health Care Centers it operates (8 primary care clinics and 1 central sexually transmitted disease clinic). The data included basic demographic information obtained by clerical staff when patients registered with the Health Care Centers and data from encounter forms filled out by clinical staff at each patient visit. The encounter forms record the date of the visit and up to 4 diagnostic codes. This information system has data on all patient encounters since March 1, 1993. A list of all patients who received a diagnosis of diabetes (International Classification of Disease, Ninth Revision24 code 250) at any time between March 1, 1993, and December 31, 2001, was obtained from the system, with the date of the first visit for which a diabetes diagnosis was recorded. We did not attempt to distinguish between type 1 and type 2 diabetes, as use of the 2 codes was not consistent throughout this period.
Hospital discharge data for these patients were obtained from the Pennsylvania Health Care Cost Containment Council, a state agency mandated to collect data on all admissions to hospitals in Pennsylvania. The data collected included demographic information, the reason for admission, up to 8 diagnostic codes, dates of admission and discharge, and total charges. Because hospitals are required by state law to submit the data and the Pennsylvania Health Care Cost Containment Council undertakes extensive data quality checks, the data were essentially complete for all Pennsylvania hospitals for the period covered in this study.25
Patients identified from the outpatient database were linked to records in the hospital discharge data on the basis of social security number (SSN), gender, and date of birth (DOB). Patients with no SSN recorded were excluded. Records were linked on the basis of 1 of several criteria: SSN, gender, and DOB; SSN, gender, and month and year of birth; SSN, gender, and month and day of birth, with year of birth within 2 years; or gender, DOB, and 8 of 9 digits matched for the SSN. More than 99% of all matches were exact matches on all 3 identifiers.
Patients were also linked to death records maintained by the Philadelphia Department of Public Health for all Philadelphia residents in order to determine length of follow-up time. Records were linked on the basis of either first and last name, gender, and DOB, or first or last name, gender, SSN, and partial DOB match. Race/ethnicity was classified on the basis of the outpatient records because there were extensive missing data on this variable in the hospitalization records. For this study, follow-up time for each patient began with the first outpatient visit with a diagnosis of diabetes within the study period, and ended at December 31, 2001, or date of death, if a death was identified.
Differences in hospitalization rates and mean hospital charges were tested by linear regression in SAS version 9.1 (SAS Institute Inc, Cary, NC), with gender, age, and racial/ethnic groups entered as independent variables and number of hospital admissions and hospital charges per year as the dependent variables. Individual patients were used as the unit of analysis, and results were weighted by follow-up time.
RESULTS
Among the 19437 eligible patients identified from outpatient records, 618 (3.1%) had no SSN recorded and were excluded from the study. An additional 19 patients (0.1%), each of whom had 1 outpatient visit and no hospital admissions recorded, were excluded because we located death records that preceded their outpatient record. The remaining 18800 patients were included in these analyses.
The characteristics of the patient population are shown in Table 1 ▶. Females made up 57% of the group. A majority of patients (73%) were African American, with substantial numbers of non-Hispanic Whites (n=2284 [12%]), Hispanics (n=1828 [10%]), and Asian Americans (n=579 [3%]). The median age at beginning of follow-up was 52.0 years; the age range was from younger than 1 year to older than 100 years. Patients had an average follow-up time of 4.6 years. Income and insurance information were retained in the administrative data only for the 9379 patients with recent visits to the Health Care Centers. Among these patients, the mean income was $8671. Forty-one percent had no insurance, 16% had Medicaid, 27% had Medicare, 8% had private insurance, and 8% were recorded as having some other type of insurance. Deaths during the study period were ascertained for 1794 patients, 9.5% of the cohort.
TABLE 1—
Patient Characteristics, Hospital Admissions, and Hospital Charges for Patients With Diabetes: Philadelphia Health Care Centers, March 1993–December 2001
| Number | Percent of Patients | Total Hospital Admissions | Hospital Admissions per Person Year (SD) | Total Hospital Charges, $ | Hospital Charges per Person Year, $ (SD) | |
| Total | 18 800 | 100 | 30 528 | 0.351 (1.642) | 818 749 563 | 9 414 (63 055) |
| Gender | ||||||
| Female | 10 649 | 57 | 16 254 | 0.323 (1.474) | 431 759 996 | 8 569 (61 938) |
| Male | 8 151 | 43 | 14 274 | 0.390 (1.836) | 386 989 568 | 10 578 (64 409) |
| Race/ethnicity | ||||||
| African American | 13 733 | 73 | 23 127 | 0.363 (1.664) | 630 790 480 | 9 891 (67 447) |
| Non-Hispanic White | 2 284 | 12 | 4 691 | 0.414 (1.804) | 119 944 539 | 10 580 (59 422) |
| Hispanic | 1 828 | 10 | 2 168 | 0.267 (1.422) | 51 458 780 | 6 341 (39 501) |
| Asian | 579 | 3 | 318 | 0.133 (0.996) | 9 048 269 | 3 788 (29 218) |
| Other | 363 | 2 | 212 | 0.163 (1.283) | 7 180 174 | 5 518 (42 411) |
| Unknown | 13 | 0 | 12 | 0.321 (0.761) | 327 321 | 5 994 (38 777) |
| Age at baseline | ||||||
| 0–14 y | 160 | 1 | 120 | 0.038 (0.340) | 1 747 153 | 577 (5908) |
| 15–24 y | 688 | 4 | 950 | 0.290 (1.491) | 14 410 290 | 4 403 (34 552) |
| 25–34 y | 1 707 | 9 | 2 344 | 0.311 (2.125) | 41 023 826 | 5 452 (41 690) |
| 35–44 y | 3 575 | 19 | 4 995 | 0.330 (1.695) | 111 347 512 | 7 361 (50 493) |
| 45–54 y | 4 680 | 25 | 6 623 | 0.328 (1.501) | 183 366 061 | 9 079 (71 439) |
| 55–64 y | 4 826 | 26 | 8 555 | 0.371 (1.609) | 261 361 574 | 11 337 (71 575) |
| 65–74 y | 2 286 | 12 | 5 043 | 0.397 (1.614) | 150 895 734 | 11 892 (63 344) |
| ≥ 75 y | 878 | 5 | 1 898 | 0.400 (1.525) | 54 597 414 | 11 786 (60 748) |
| Number of hospitalizations | ||||||
| 0 | 10 937 | 58 | 0 | 0.000 (0.000) | 0 | 0.000 (0.000) |
| 1–4 | 5 893 | 31 | 11 050 | 0.343 (0.793) | 291 542 630 | 9 049 (70 596) |
| ≥ 5 | 1 970 | 10 | 19 478 | 1.591 (3.413) | 527 206 933 | 43 086 (118 683) |
The study population experienced a total of 30528 hospital admissions during 86967 person-years of follow-up, for a hospitalization rate of 0.35 per person-year (Table 1 ▶). Males were more frequently hospitalized than females (0.39 vs 0.32 admissions per year), and hospital admissions and charges generally increased with age except in the oldest age group (≥ 75 years). Non-Hispanic Whites were the most frequently hospitalized group (0.41 admissions per year), compared with African Americans (0.36), Hispanics (0.27), Asian Americans (0.13), and other racial/ethnic groups (0.16). Total hospital charges were $818749563, or $9414 per person-year of follow-up. The mean charges per hospital admission were $26820. At least 1 hospital admission was identified for 41.8% of the patients. Patients who were hospitalized at least once had an average of 3.9 hospitalizations. Patients who were hospitalized at least 5 times made up 10.5% of the study population and accounted for 64% of all hospital admissions and hospital charges and 36% of the deaths in this patient cohort.
In multivariate models adjusted for race/ethnicity, age, and gender, the associations of hospital admission rates and charges with race/ethnicity were the same as in the crude rates (Table 2 ▶), but a significant interaction between gender and age was detected for both outcomes. This interaction on hospitalization rates is illustrated in Figure 1 ▶, which shows unadjusted hospital rates by age group and gender. Among patients aged younger than 35 years, hospital admissions were higher in female patients than in male patients. Crossover occurred in early adulthood, with men aged 55 to 74 years having a substantial excess rate of hospitalization relative to women of the same age group. Other interactions were not statistically significant and were not included in the final models.
TABLE 2—
Multivariate Predictors of Hospital Admissions and Charges for Patients With Diabetes: Philadelphia Health Care Centers, March 1993–December 2001
| Hospitalizations per Person-Year, Parametera (95% Confidence Interval) | Hospital Charges per Person-Year, Parameterb (95% Confidence Interval) | |
| Race/ethnicity | ||
| African American | Reference | Reference |
| Non-Hispanic White | 0.040 (0.008, 0.073) | $184 (−$1071, $1439) |
| Hispanic | −0.09 (−0.137, −0.061) | −$34 (−$4923, −$2015) |
| Asian | −0.24 (−0.307, −0.173) | −$65 (−$9071, −$3946) |
| Other | −0.20 (−0.298, −0.119) | −$45 (−$8020, −$1133) |
| Unknown | −0.09 (−0.524, 0.344) | −$62 (−$17 275, $16 028) |
| Gender × age interaction | ||
| Female gender | 0.109 (0.030, 0.189) | $261 (−$434, $5654) |
| Age at baseline (per 10 years) | 0.046 (0.035, 0.057) | $222 ($1799, $2643) |
| Female × age interaction (per 10 years) | −0.03 (−0.051, −0.022) | −$10 (−$1589, −$461) |
aAdditional hospitalizations per year relative to reference category, adjusted for other variables shown.
bAdditional hospital charges per year relative to reference category, adjusted for other variables shown.
FIGURE 1—
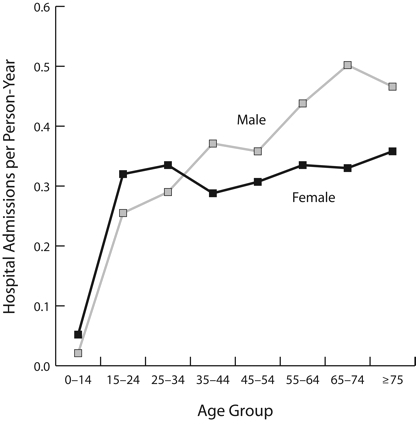
Hospital admissions per person-year, by age and gender for patients with diabetes: Philadelphia Health Care Centers, March 1993–December 2001.
DISCUSSION
We have presented data based on clinical records for a large, racially diverse population of low-income diabetic patients of all ages, with follow-up time up to 106 months. Our findings confirm that individuals with diabetes experience a substantial burden of serious morbidity requiring hospitalization, with an average of 0.35 hospital admissions per person-year. There were differences between racial/ethnic groups in rates of hospitalization, with Hispanic and Asian patients having substantially lower rates than non-Hispanic Whites or African Americans. After early adulthood, hospitalization rates and charges rose with age much more sharply among men than women, so that women had higher rates at younger ages and men at higher ages. The small proportion of patients with 5 or more hospitalizations accounted for 64% of all hospital admissions and charges in this population.
Racial/Ethnic Differences
Hispanics and Asian Americans in this low-income population were hospitalized substantially less frequently than either non-Hispanic Whites or African Americans. The rates for Hispanics were comparable to those reported in other studies.19,26,27 We are unaware of any published data on hospitalization rates among Asian patients with diabetes in the United States. The poorest outcomes in this patient population were experienced by non-Hispanic Whites, who were hospitalized significantly more frequently than any other group. It is possible that this reflects underutilization of appropriate and needed health services by minority patients, as has been documented in other contexts.21,28,29 However, in this patient cohort, non-Hispanic Whites also had higher rates of myocardial infarction and all heart disease than other groups, in spite of lower prevalence of hypertension,30 which would be consistent with more frequent hospitalizations reflecting poorer health status rather than more aggressive treatment.
Gender–Age Interaction
Gender differences in hospitalization rates and charges were age-dependent, reflected in a significant interaction between gender and age. Boys and men aged younger than 35 years had lower rates than girls and women of the same age, whereas men aged older than 45 years had more than 30% higher rates of hospital admissions and charges than women in the same age group. We speculated that reproductive events, which lead to a significant number of hospital admissions in early female adulthood, might explain this pattern. However, excluding hospitalizations associated with reproduction from the calculations of hospitalization rates did not eliminate the interaction between age and gender. Because few studies of hospitalization among diabetic patients have been published, we are not aware of any other research either confirming or contradicting the interaction we detected.
Younger women may have especially high rates of psychosocial stressors impacting their health behaviors and outcomes.31 Depression, which is more common among women than men and among younger rather than older diabetic patients,32 is associated with poorer outcomes for diabetic patients, including increased hospital utilization.33
Interactions of gender and age have been reported in outcomes for patients with coronary heart disease, with younger, but not older, women having poorer outcomes than men. Several possible explanations have been proposed, including gender differentials in referrals for treatment or intensity of treatment.34,35 Younger women with diagnosed diabetes may similarly be a select group with unusually severe disease, which could lead to the interaction we observed. Additional investigations are required to confirm this interaction and to determine its causes and significance for patient care.
Safety-Net Clinics
Patients treated in safety-net clinics such as the Philadelphia Health Care Centers typically have a range of risk factors that put them at increased risk of poor health outcomes. They are far more likely than the general population to be low-income, lack medical insurance, have low educational status, and be members of minority racial/ethnic groups. Other researchers have found low socioeconomic status indicators to be associated with increased rates of hospitalization among diabetic patients.36,37
In spite of these factors, this large cohort of diabetic patients did not have unusually high rates of hospital admissions compared with other patient populations.10,11,19,38–42 It is notable that this was true even though most previous studies have reported either on nationally representative samples or on predominantly White populations, not on low-income patient groups. The reasons for the relatively low rates of hospitalization in this cohort deserve further examination. Use of pharmaceuticals by patients with diabetes has been found to be particularly sensitive to out-of-pocket costs, so it is possible that access to prescription drugs and supplies for self-monitoring blood glucose without financial barriers helped these patients to avoid hospitalizations.43,44
Limitations
There are several limitations to this study. The completeness and accuracy of data collected for administrative purposes are uncertain, and may have varied over time and among centers. It is possible that some patients with diabetes treated in the Health Care Centers for other conditions were not ascertained, as a majority of encounter forms list only 1 or 2 diagnoses.
Admissions to hospitals outside Pennsylvania would not be included in the hospitalizations we tabulated. Similarly, follow-up time was censored for patients who died during the study period, based on death records maintained by the Philadelphia Department of Public Health. Although all deaths to Philadelphia residents should be reported to Philadelphia Department of Public Health and included in these records regardless of place of death, patients who moved out of the city and subsequently died would not be included. Missed hospital admissions and missed death records would both tend to lower reported hospitalization rates. However, the hospitals outside Philadelphia most frequently used by Philadelphia residents are in surrounding counties in Pennsylvania and are included here. Out-of-state hospitalizations are particularly infrequent for low-income and uninsured patients. Hospitalizations for patients who moved out of state and were subsequently hospitalized there would be missed in these data. On the basis of census data on out-of-county and out-of-state moves,45 we estimate that fewer than 5% of this low-income patient cohort would have moved out of the city during the study period, fewer than 2% of them out of state (details available from corresponding author). The missed data were therefore unlikely to substantially affect the reported results.
Conclusions
The patient population described here resembles other populations in that a small proportion of patients experienced a majority of the negative outcomes assessed and incurred a majority of the total costs.46 Although some interventions designed to reduce repeat hospital admissions among diabetic patients have not been successful,47 further efforts must be made to define this high-risk patient population and develop methods to reduce morbidity and repeat hospitalizations. In addition, the possibility that access to primary care and pharmacy services without out-of-pocket costs enabled this predominantly minority, low-income patient population to avoid excess hospitalizations suggests that efforts to improve outcomes for diabetic patients should include efforts to expand such access and to resist policy changes that would create additional financial barriers to care.
Acknowledgments
This research was supported by the National Institute of Diabetes, Digestive, and Kidney Diseases (grant #R21DK06420-11).
The authors wish to acknowledge the advice and support of Neil I. Goldfarb, Barry J. Goldstein, David B. Nash, Etienne Phipps, Warner S. Tillack, Jr., and Viola Vaccarino. Data were collected by the Pennsylvania Health Care Cost Containment Council and the Philadelphia Department of Public Health Division of Ambulatory Health Services.
Human Participant Protection The study protocol was approved by the Philadelphia Department of Public Health institutional review board.
Peer Reviewed
Contributors The authors jointly originated the study. J.M. Robbins obtained the data, designed the study, performed the analyses, and drafted the article. D.A. Webb helped to conceptualize ideas and interpret findings, and revised the article.
References
- 1.Engelgau MM, Geiss LS, Saaddine JB, et al. The evolving diabetes burden in the United States. Ann Intern Med. 2004;140:945–950. [DOI] [PubMed] [Google Scholar]
- 2.Boyle JP, Honeycutt AA, Narayan KM, et al. Projection of diabetes burden through 2050: impact of changing demography and disease prevalence in the US Diabetes Care. 2001;24:1936–1940. [DOI] [PubMed] [Google Scholar]
- 3.Kumanyika SK. Diet and nutrition as influences on the morbidity/mortality gap. Ann Epidemiol. 1993; 3:154–158. [DOI] [PubMed] [Google Scholar]
- 4.Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and type 2 diabetes in African American and non-Hispanic white women and men: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2001;91:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson RN. Deaths: leading causes for 1999. Natl Vital Stat Rep. 2001;49:1–87. [PubMed] [Google Scholar]
- 6.Huang ES, Meigs JB, Singer DE. The effect of interventions to prevent cardiovascular disease in patients with type 2 diabetes mellitus. Am J Med. 2001;111:633–642. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan NM. Management of hypertension in patients with type 2 diabetes mellitus: guidelines based on current evidence. Ann Intern Med. 2001;135:1079–1083. [DOI] [PubMed] [Google Scholar]
- 8.Cooper DS, DeAngelis CD. Diabetes mellitus—a call for papers [editorial]. JAMA. 2001;286:968–969. [DOI] [PubMed] [Google Scholar]
- 9.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–574. [DOI] [PubMed] [Google Scholar]
- 10.Harris MI. Health care and health status and outcomes for patients with type 2 diabetes. Diabetes Care. 2000;23:754–758. [DOI] [PubMed] [Google Scholar]
- 11.Chin MH, Zhang JX, Merrell K. Diabetes in the African-American Medicare population. Morbidity, quality of care, and resource utilization. Diabetes Care. 1998;21:1090–1095. [DOI] [PubMed] [Google Scholar]
- 12.Martin TL, Selby JV, Zhang D. Physician and patient prevention practices in NIDDM in a large urban managed-care organization. Diabetes Care. 1995;18: 1124–1132. [DOI] [PubMed] [Google Scholar]
- 13.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed]
- 14.Fiscella K, Williams DR. Health disparities based on socioeconomic inequities: implications for urban health care. Acad Med. 2004;79:1139–1147. [DOI] [PubMed] [Google Scholar]
- 15.Felix-Aaron K, Moy E, Kang M, Patel M, Chesley FD, Clancy C. Variation in quality of men’s health care by race/ethnicity and social class. Med Care. 2005; 43(3 suppl):I72–I81. [DOI] [PubMed] [Google Scholar]
- 16.Krop JS, Powe NR, Weller WE, Shaffer TJ, Saudek CD, Anderson GF. Patterns of expenditures and use of services among older adults with diabetes. Implications for the transition to capitated managed care. Diabetes Care. 1998;21:747–752. [DOI] [PubMed] [Google Scholar]
- 17.Pennsylvania Department of Health. State Health Improvement Plan: Special Report on the Health Status of Minorities in Pennsylvania. Available at: http://www.dsf.health.state.pa.us/health/cwp/view.asp?a=169&q=231311&PM=1. Accessed July 18, 2005.
- 18.Pappas G, Hadden WC, Kozak LJ, Fisher GF. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997;87:811–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aubert RE, Geiss LS, Ballard DJ, Cocanougher B, Herman WH. Diabetes-related hospitalization and hospital utilization. In: Harris MI, Cowie CC, Stern MP, eds. Diabetes in America. 2nd ed. Washington, DC: US Dept of Health and Human Services, National Institutes of Health; 1995:553–569. DHHS publication NIH 95-1468. Available at: http://diabetes.niddk.nih.gov/dm/pubs/america/pdf/chapter27.pdf. Accessed July 18, 2005.
- 20.Laditka SB, Mastanduno MP, Laditka JN. Health care use of individuals with diabetes in an employer-based insurance population. Arch Intern Med. 2001; 161:1301–1308. [DOI] [PubMed] [Google Scholar]
- 21.Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. Racial disparities in diabetes care processes, outcomes, and treatment intensity. Med Care. 2003;41: 1221–1232. [DOI] [PubMed] [Google Scholar]
- 22.Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and development of disability among older persons. JAMA. 2004;292:2115–2124. [DOI] [PubMed] [Google Scholar]
- 23.Davis SK, Liu Y, Gibbons GH. Disparities in trends of hospitalization for potentially preventable chronic conditions among African Americans during the 1990s: implications and benchmarks. Am J Public Health. 2003;93:447–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization. International Classification of Disease, Ninth Revision. Geneva, Switzerland: World Health Organization; 1977.
- 25.Chung JS, Murphy RX Jr, Reed JF III, Kleinman LC. Quality analysis of bilateral reduction mammaplasty using a state-legislated comparative database and an internal hospital-based system. Ann Plast Surg. 2003;51: 446–449. [DOI] [PubMed] [Google Scholar]
- 26.Bastida E, Cuellar I, Villas P. Prevalence of diabetes mellitus and related conditions in a south Texas Mexican American sample. J Community Health Nurs. 2001;18:75–84. [DOI] [PubMed] [Google Scholar]
- 27.Lipton R, Losey L, Giachello AL, Corral M, Girotti MH, Mendez JJ. Factors affecting diabetes treatment and patient education among Latinos: results of a preliminary study in Chicago. J Med Syst. 1996;20:267–276. [DOI] [PubMed] [Google Scholar]
- 28.Safford M, Eaton L, Hawley G, et al. Disparities in use of lipid-lowering medications among people with type 2 diabetes mellitus. Arch Intern Med. 2003;163: 922–928. [DOI] [PubMed] [Google Scholar]
- 29.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350–1359. [DOI] [PubMed] [Google Scholar]
- 30.Robbins JM, Webb DA, Sciamanna CN. Cardiovascular comorbidities among public health clinic patients with diabetes: the Urban Diabetics Study. BMC Public Health. 2005;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franco-Bronson K, Tamburrino M, McGowan N. Sex differences in long-term mortality after myocardial infarction [letter]. Ann Intern Med. 2001;135: 1089–1090. [DOI] [PubMed] [Google Scholar]
- 32.Katon W, von Korff M, Ciechanowski P, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004; 27:914–920. [DOI] [PubMed] [Google Scholar]
- 33.Husaini BA, Hull PC, Sherkat DE, et al. Diabetes, depression, and healthcare utilization among African Americans in primary care. J Natl Med Assoc. 2004; 96:476–484. [PMC free article] [PubMed] [Google Scholar]
- 34.Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Intern Med. 2001;134:173–181. [DOI] [PubMed] [Google Scholar]
- 35.Vaccarino V, Abramson JL, Veledar E, Weintraub WS. Sex differences in hospital mortality after coronary artery bypass surgery: evidence for a higher mortality in younger women. Circulation. 2002;105:1176–1181. [DOI] [PubMed] [Google Scholar]
- 36.Booth GL, Hux JE. Relationship between avoidable hospitalizations for diabetes mellitus and income level. Arch Intern Med. 2003;163:101–106. [DOI] [PubMed] [Google Scholar]
- 37.Majeed A, Bardsley M, Morgan D, O’Sullivan C, Bindman AB. Cross sectional study of primary care groups in London: association of measures of socioeconomic and health status with hospital admission rates. BMJ. 2000;321:1057–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moss SE, Klein R, Klein BE. Risk factors for hospitalization in people with diabetes. Arch Intern Med. 1999;159:2053–2057. [DOI] [PubMed] [Google Scholar]
- 39.Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults: a 3-year prospective study. Diabetes Care. 1998;21:231–235. [DOI] [PubMed] [Google Scholar]
- 40.Wagner EH, Sandhu N, Newton KM, McCulloch DK, Ramsey SD, Grothaus LC. Effect of improved glycemic control on health care costs and utilization. JAMA. 2001;285:182–189. [DOI] [PubMed] [Google Scholar]
- 41.Pogach LM, Hawley G, Weinstock R, et al. Diabetes prevalence and hospital and pharmacy use in the Veterans Health Administration (1994). Use of an ambulatory care pharmacy-derived database. Diabetes Care. 1998;21:368–373. [DOI] [PubMed] [Google Scholar]
- 42.Maciejewski ML, Maynard C. Diabetes-related utilization and costs for inpatient and outpatient services in the Veterans Administration. Diabetes Care. 2004; 27(suppl 2):B69–B73. [DOI] [PubMed] [Google Scholar]
- 43.Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291:2344–2350. [DOI] [PubMed] [Google Scholar]
- 44.Burge MR. Lack of compliance with home blood glucose monitoring predicts hospitalization in diabetes. Diabetes Care. 2001;24:1502–1503. [DOI] [PubMed] [Google Scholar]
- 45.US Bureau of the Census. Census 2000 County-to-County Migration Flow Files; 2003. Available at: http://www.census.gov/population/www/cen2000/ctytoctyflow.html. Accessed September 21, 2004.
- 46.Garfinkel SA, Riley GF, Iannacchione VG. High-cost users of medical care. Health Care Financ Rev. 1988;9:41–52. [PMC free article] [PubMed] [Google Scholar]
- 47.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334:1441–1447. [DOI] [PubMed] [Google Scholar]


