Abstract
Objective
We analysed the integrated planning model adopted by the Italian region Emilia Romagna in year 2000 to cover the entire range of treatment of cardiovascular disease. This model, called “hub and spoke”, provides for the transfer of patient care and treatment from peripheral units (the spokes) to central units (the hubs) once a certain complexity threshold has been reached.
Methods
We examined inter-temporal variations in patients flows for the selection/referral and follow-up phases between cardiac surgery and cardiology units during two periods characterised by different organisational set-ups, in order to reflect on the progress being made in the organisation of the network. The database consisted of regional records of hospital discharges during the 1997–2001 period.
Results
The investigation pointed to the achievement of a good degree of coordination between structures at different levels of specialisation in the case of cardiac surgery, for which six centres were selected already in 1996. On the other hand, the more recent introduction of a hierarchical system for interventional cardiology points to the prevalence of operations on patients previously treated within the same centre, to admissions by direct access, and to follow-up mainly conducted within the hub providing the initial service.
Conclusions
Despite the progress made towards the more effective rationalisation of the health care network, there is still room for improvement in relations between different centres, in particular with regard to the clearer definition of the roles and interdependence of those intermediate-level centres located between the hub centres and basic healthcare facilities.
Keywords: integrated health care networks, cardiac surgery, interventional cardiology, patient flows
Introduction
Economic analysis has recently turned its attention on the importance of cooperative relations between individual organisations within a network, producing among other things a debate over how public sector policy may be implemented through a system of cooperative networks involving service suppliers [1, 2]. However, studies have tended to focus less attention on any analysis of efficiency within the network, while an understanding of this is of critical importance, in particular for local policy makers. This especially concerns situations in which there are a number of different stakeholders [3], and in the case of those health and educational services that are often furnished by private or non-profit-making agencies, the activities of which are more difficult for a public third payer to control. In particular, there is an implicit underlying belief that, when providing a given, complex range of services to a specific community, the creation of interdependent links between two or more individual subjects who decide to cooperate is, a priori, more effective than the separate actions of the same individuals could in fact be. This viewpoint engenders a frequent appeal to the logic of networks as the favoured organisational model for the supply of publicly funded services, albeit without any corresponding doubt being raised about the real validity of such networks. In the case of these services, the coordination of diverse decisional levels within a network is motivated by a legal mandate, and it is the planner's responsibility to guide the network's member organisations in accordance with the pre-established objectives.
Within such a framework, if we wish to evaluate the functioning of an integrated network model for the supply of hospital services, we should simultaneously consider three different aspects.
First, we should consider the contribution made by the network toward satisfying the specific requirements of a given catchment area, creates a series of indicators which aim to evaluate the improvements achieved in the populations state of health, the patients' degree of satisfaction, the equity of access to the services, the efficacy of the treatment provided, etc. [4, 5].
Second, we should consider an analysis of just how resources are acquired and how they are allocated to and within the network, in order to maximise the overall efficiency of the network for the greater benefit of the population involved. To this end, the validity of the network ought to be judged in terms of the objectives set by the central planner, checking that the range of services provided is wide enough—otherwise clients within the catchment area may have to leave the network—but not too wide, as may be the case if there are too many network units. The above is clearly influenced by the entity of the economic and financial ties binding the funding body.
Third, an evaluation of the incentive system the funding body introduces with regard to the individual members of the network on the supply side pays special attention to the nature of the restrictions on participation and on the respective incentives offered to the structures and to those professionals working there. From this point of view, a periodical assessment of the contribution made by the individual productive units towards the overall success of the network allows to identify promptly those situations that are critical from the point of view of the effectiveness or efficiency of the service provided.
Such a wide-ranging study would inevitably extend beyond the space and time allocated to the present work, which goes no further than an initial explorative analysis of those features more closely linked to the structural framework and to the degree in which the various structures share the organisational objectives of regional planning. We focus on an analysis of the integrated planning model adopted by the Emilia Romagna region in Italy for tertiary care. This model, called “hub and spoke”, provides for the transfer of patient care and treatment from peripheral units to central units once a certain complexity threshold has been reached. Cardiac surgery and interventional cardiology were the first chosen areas for the application of this planning model, but the Regional Health Plan 1999–2001 envisages its forthcoming extension to other important medical areas from the regional viewpoint, such as neurosurgery and intensive care.
For the treatment of cardiovascular disease there are important international network experiences that could offer Emilia Romagna interesting organisational advice. The most important is the Cardiac Care Network in Ontario, one of the first integrated systems for the provision of cardiovascular services, set up in 1990, and one of the most highly developed ones (for a detailed description see www.ccn.on.ca). Another interesting example is the Anthem Blue Cross and Blue Shield in the USA. They are the result of the efforts of one of the five largest managed care organisations in the United States to exploit the advantages of an integrated network model for the provision of cardiological services [6]. As far as Europe is concerned, in Scotland a pilot network model has been introduced in 2001 for the treatment of cardiovascular disease [7].
As regards Emilia Romagna, our study aims to identify the system of relations currently existing between peripheral units and complex units in the cardiovascular sector. The study also aims to evaluate changes that have been produced in the selection/referral processes resulting from improvements made in the cardiac surgery network and from the formal introduction of the hub and spoke hierarchical model for interventional cardiology. To this end, we compare the paths taken by a cohort of patients admitted for revascularisation treatment in 1998—thus during the initial stage of the cardiac surgery network and prior to the introduction of the hub and spoke model for interventional cardiology—with these paths taken by a cohort of patients admitted for revascularisation treatment in 2000, immediately after the introduction of the new organisational model that covers the entire range of treatment of cardiovascular disease. An analysis of the selective referral process for these patients will be made with regard to the phases of diagnosis/referral, revascularisation treatment and follow-up.
The integrated network of coronary revascularisation services in Emilia Romagna
In Emilia Romagna, the Regional Health Plan 1999–2001 [8] fell within the new legislative framework defined by Legislative Decree 229/99, whereby potentially competitive factors are subordinate to programming requirements and financial feasibility. The adopted negotiated planning model particular emphasises a centralised scheme for the provision of incentives to cooperation between producers and financers, rather than on any competitive mechanism. Long-term regional objectives aim at the formulation of a network with no duplication of services, on the basis that the rationalisation of supply and its concentration in certain crucial points allows for greater control over the quality and the cost of the assistance provided.
The Regional Health Plan 1999–2001 applies the hub and spoke model for tertiary care, envisaging the concentration of the production of more complex care and treatment in centres of excellence (the hub) and the organisation of referral from peripheral centres (the spoke), whose main task is to select and refer patients to the right centres. The treatment of cardiovascular disease is chosen among those functions for this initial utilisation of the hub and spoke planning model with regard to interventional cardiology and cardiac surgery.
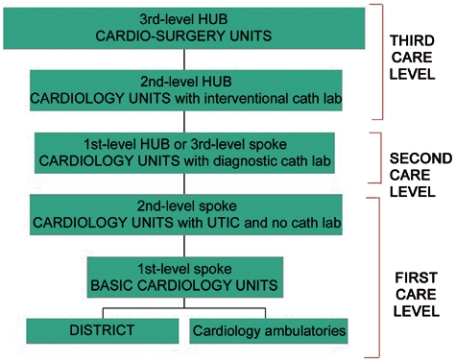
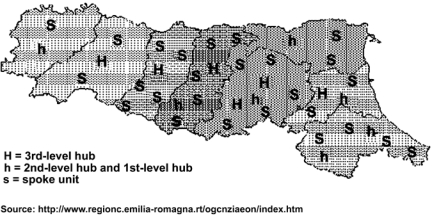
The system provides for the organisation of an integrated network of services classified, according to their degree of complexity, into 1st, 2nd and 3rd level care. See Figure 1 for a graphic representation of the hierarchical referral process introduced by the model and Figure 2 for a map of Emilia Romagna region that shows the territorial location of the acute hospitals defined as hubs and spokes in the integrated network.
Figure 1.
The hierarchical system of relations between cardiology units.
Figure 2.
The hub and spoke model in Emilia Romagna.
The first two levels come within the framework of provincial self-sufficiency. The first level includes 1st and 2nd level spokes that make up the provincial hospital network and intervene during the selection/transfer and subsequent follow-up phases. The second level includes 1st hubs that are spokes for the third level of care: cardiology units equipped with diagnostic cathlab. The third level consists of regional interventional cardiology units (2nd level hub) and of the six cardiac surgery units (3rd level hub)—two public and four private.
Cardiac surgery units were classified in 1996 as the highest hubs of the hospitals network and their work is governed by a regional agreement defining the financial and/or quantitative thresholds assigned to the public and private sectors on the basis of an estimate of the epidemiological needs of the local population [9, 10]. All cardiac surgery centres have been allocated a specific local catchment area for emergency patients. Even in the case of emergency hospitalisation, the cardiology unit that sent the patient is responsible for performing the necessary follow-up once the emergency period is over. For non-emergency operations, each patient has the right to choose a cardiac surgery centre other than his/her local one, even though a high degree of referral from provincial structures to a patient's own local centre would nevertheless be a desirable goal for the regional planner, in the interests of a more balanced growth of the network.
Methods
On the basis of the evaluation framework of a network organisation model mentioned in the introduction—ideally sub-divided into three levels—our empirical analysis focused on a preliminary examination of the internal efficiency of the regional network with regard to certain aspects only of the second and third levels of the proposed framework. In particular, an investigation into the inter-temporal variations in flows between cardiology and cardiac surgery units during two periods characterised by different organisational set-ups, allows us to reflect on the progress made in the organisation of the network, and on the degree of consent expressed by the structures in question with regard to the regional planner's aim of rationalising the treatment of cardiovascular disease.
Hence, we have taken those patients admitted to hospital in 1998 and in 2000 as our reference groups. We have chosen 1998 in order to examine the relationship between hospitals that belong to a system not yet completely organised along hierarchical lines. The comparison with the group of patients in 2000, the year in which the integrated network system for vascular treatment was completed, thus enables us to describe and evaluate those steps already being taken towards building and perfecting the network, by examining the dynamics of the flow of patients between the hubs and the spoke-level regional structures during the selection/referral and follow-up phases.
The database used consists of regional records of hospital discharges during the 1997–2001 period, with the exception of extra-regional patients and of paediatric patients. The hospital admissions taken into consideration were identified using the procedural codes ICD-9-CM, whereby heart valves and coronary artery bypass graft (CABG) operations were chosen in the case of cardiac surgery (coded as: ICD9-CM 361.xx, 352.xx and 353.xx), while angioplasty operations were chosen for interventional cardiology (PTCA, code ICD9-CM 360.xx). The two groups include those patients who, during the two years in question, received their first revascularisation operation. In order to analyse the selection/referral and follow-up processes for each patient, our information about admissions for the operation (the principal admission) was supplemented by other information concerning any prior or subsequent admissions within the same diagnostic category (MDC 5) which may have occurred one year either side of the revascularisation operation.
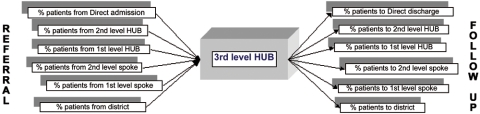
In an attempt to offer a more detailed reading of relations between the centres that make up the regional cardiology network, we examined in detail the territorial selective referral process among centres of different complexity with regard to the phases of diagnosis, referral, operation and follow-up, following the scheme indicated in Figure 3.
Figure 3.
An example of the territorial selective referral process examined.
(The tables containing figures are available on request from the authors.)
At this end, for each regional hub, we assessed the share of patients that got in touch with a spoke structure, performing diagnosis and selection, and were referred to a 2nd level hub for angioplasty or to a 3rd level hub for angioplasty, CABG and valve operations. For these patients we considered also the share of patients that were transferred again from the hub to the spoke for the follow-up phase. Moreover, we compute the share of patients who were granted direct access to the hub structure without any prior admission (direct access), and the share of patients who were not subsequently readmitted to hospital after their operation (direct discharge).
Results
Tables 1 and 2 show a number of indicators for the various catchment areas, respectively for cardiac surgery and angioplasty operations, referred to the number of cases per area and certain variables representative of the patients case-mix (average age, percentage of patients over 70, percentage of women, Charlson's co-morbidity index calculated using the method suggested by Romano et al. 1993 [11]). For the transfer phase, a calculation was made of the number of patients who were admitted in a hub centre within one day of discharge from their previous admission (0–1 day in) in a spoke centre. Similarly, with regard to the follow-up stage, figures show the number of patients who are transferred to a spoke hospital within one day of discharge subsequent to their surgery operation (0–1 day out). Finally, observed and adjusted hospital mortality rates are given, the latter calculated by using a logistic regression model that standardises the case-mix on the basis of gender, age and Charlson's co-morbidity index.
Table 1.
CABG and heart valves procedures, descriptive analysis for catchment area
| No | Age | Case-mix |
Referral | Follow-up | Mortality |
||||
|---|---|---|---|---|---|---|---|---|---|
| >70 (%) |
Women (%) |
Charlson index |
0-1 day in (%) |
0-1 day out (%) |
Obs. (%) |
Exp. (%) |
|||
| 1998 | |||||||||
| Area A | 400 | 66.4 | 37 | 25 | 1.5 | 37 | 23 | 7.3 | 4.6 |
| Area B | 499 | 65.3 | 35 | 22 | 1.4 | 30 | 28 | 4.4 | 4.3 |
| Area C | 348 | 66.1 | 36 | 26 | 1.7 | 20 | 11 | 2.6 | 4.6 |
| Area D | 576 | 67.1 | 39 | 21 | 1.9 | 6 | 26 | 2.8 | 5.0 |
| Area E | 350 | 65.9 | 34 | 21 | 1.4 | 49 | 30 | 6.9 | 4.4 |
| Total | 2173 | 66.2 | 36 | 23 | 1.6 | 26 | 24 | 4.6 | 4.6 |
| 2000 | |||||||||
| Area A | 591 | 67.9 | 42 | 26 | 1.4 | 51 | 24 | 3.9 | 2.9 |
| Area B | 446 | 66.8 | 40 | 23 | 1.4 | 67 | 45 | 3.8 | 3.0 |
| Area C | 594 | 66.7 | 38 | 22 | 1.3 | 53 | 19 | 1.9 | 2.7 |
| Area D | 539 | 67.8 | 44 | 23 | 1.5 | 5 | 39 | 2.4 | 2.9 |
| Area E | 235 | 67.6 | 45 | 23 | 1.3 | 79 | 35 | 2.1 | 2.8 |
| Total | 2405 | 67.4 | 41 | 24 | 1.4 | 47 | 31 | 2.9 | 2.9 |
Table 2.
PTCA treatments, descriptive analysis for province
| No | Age | Case-mix |
Referral | Follow-up | Mortality |
||||
|---|---|---|---|---|---|---|---|---|---|
| >70 (%) |
Women (%) |
Charlson index |
0–1 day in (%) |
0–1 day out (%) |
Obs. (%) |
Exp. (%) |
|||
| 1998 | |||||||||
| Prov 1 | 456 | 63.3 | 28 | 23 | 1.0 | 12 | 23 | 2.0 | 1.2 |
| Prov 2 | 123 | 61.6 | 19 | 24 | 0.7 | 1 | 2 | 1.6 | 0.9 |
| Prov 3 | 85 | 64.4 | 31 | 28 | 1.0 | 2 | 2 | 0.0 | 1.1 |
| Prov 4 | 308 | 62.1 | 21 | 21 | 0.9 | 12 | 33 | 1.3 | 1.1 |
| Prov 5 | 71 | 62.7 | 25 | 20 | 1.2 | 0 | 8 | 2.8 | 1.2 |
| Prov 6 | 99 | 60.1 | 15 | 27 | 1.1 | 7 | 8 | 2.0 | 1.1 |
| Prov 7 | 525 | 62.6 | 24 | 21 | 1.0 | 7 | 16 | 0.0 | 1.1 |
| Prov 8 | 182 | 61.0 | 16 | 22 | 0.8 | 10 | 14 | 0.5 | 0.9 |
| Total | 1849 | 62.4 | 23 | 22 | 1.0 | 8 | 18 | 1.1 | 1.1 |
| 2000 | |||||||||
| Prov 1 | 676 | 64.5 | 33 | 22 | 0.9 | 14 | 19 | 1.9 | 0.9 |
| Prov 2 | 243 | 63.6 | 24 | 25 | 0.9 | 3 | 5 | 0.0 | 0.8 |
| Prov 3 | 96 | 63.6 | 32 | 18 | 1.0 | 0 | 0 | 0.0 | 0.9 |
| Prov 4 | 496 | 63.9 | 30 | 23 | 1.0 | 7 | 22 | 1.2 | 0.9 |
| Prov 5 | 186 | 63.7 | 26 | 23 | 0.8 | 4 | 14 | 0.5 | 0.9 |
| Prov 6 | 359 | 64.4 | 32 | 26 | 0.7 | 5 | 17 | 1.1 | 0.9 |
| Prov 7 | 609 | 63.3 | 26 | 21 | 0.9 | 5 | 13 | 0.0 | 0.8 |
| Prov 8 | 369 | 61.7 | 22 | 20 | 0.7 | 19 | 21 | 1.1 | 0.7 |
| Prov 9 | 220 | 64.1 | 29 | 21 | 0.6 | 2 | 7 | 0.0 | 0.8 |
| Total | 3254 | 63.7 | 28 | 22 | 0.8 | 8 | 16 | 0.9 | 0.9 |
Table 1 shows there was an increase in cardiac surgery treatment of regional patients for the period 1998–2000. Regional distribution of these operations changed noticeably during the course of the observed period: in particular, 1998 represented a treatment high-point for catchment area D—which also showed the highest co-morbidity index for both periods—whereas the year 2000 saw the public cardiac surgery units in catchment areas A and C recovering sharply. The percentage of transfers that took place within one day of discharge rose sharply, pointing to the greater rapidity with which transfers take place between centres of varying levels of complexity. A similar sign of the improvement in the hierarchical organisation of the network was seen in the case of follow-up. The regional mortality rate observed over the three-year period fell by 31%, although certain differences among mortality rates for the various catchment areas remain. Those units that in 1998 saw forecast mortality rates which were lower than the observed mortality rates— that is, gross mortality rates apparently unjustified by the case-mix of treated patients—are the ones situated in catchment areas A and E. In the year 2000, the differences between observed and forecast mortality rates were not as appreciable, although catchment area A continued to feature a gross mortality rate over and above the standardised figure.
Table 2 indicates a 76% increase in angioplasty operations during the three-year period in question for all those provinces taken into account. As far as the case-mix variables are concerned, the average age of treated patients rose, as did the percentage of elderly patients. The comorbidity index fell slightly, as a result of the considerable increase in the number of cases treated, and thus of the broadening of the category of patients subjected to this type of revascularisation operation. Regional percentages for the transfer of patients carried out within a day of discharge remained stationary, whereas during the follow-up phase the percentage of day-hospital transfers doubled and the number of patients transferred within one day fell.
Therefore, an initial examination of the interventional cardiology network shows room for improvement in the transfer of patients from peripheral centres to those third level centres capable of performing angioplasty.
A detailed exam of the territorial selective referral process among centres of different complexity, illustrated by the scheme in Figure 3 (tables are available on request) suggested the following conclusions.
For cardiac surgery, the comparison of the two years, 1998 and 2000, shows there had been significant improvements in the organisation of its network with regard to catchment area A: figures show a fall in the incidence of direct access, accompanied by a clearer perception of the transfer network on the part of the provincial spoke structures, while the cardiac surgical centre's follow-up work declines as discharged patients are sent to the spoke units in province 1. The above-mentioned trend observed for this area, whereby the transfer processes are gradually developing in the right direction, as wished for by the regional planner, can also be seen in the local catchment areas B, C and E. In the case of catchment area D, on the other hand, there are certain trends that go against the previous general framework. Against an increase in the transfers by structures situated in the provinces in question, the cardiac surgery unit continues to perform a significant proportion of post-operative care, despite the fact that the percentage of patients who are re-admitted to the same centre subsequent to their main admission is on the decline.
In the case of PCTA operations, the catchment areas correspond to the provinces. In province 1 there are two cardiac surgery centres operating together with a 2nd level hub. The 3rd level public hub satisfied the majority share of regional residents' demand directed towards that same province, albeit to a lesser degree than at the start of the same period, due to the increased activity of the 2nd level hub. The direct access of patients rose from 32 to 46%. Province 7 possesses a well-structured network of four supply points: one 3rd level hub, one 2nd level hub and two 2nd level spokes. The strengthening of the provincial network is reflected in the reduction of patients treated by the cardiac surgery centre, although it maintained its appeal to those patients from other provinces, whose numbers increased further in 2000. During the course of the same year, the 3rd level hub saw a drastic reduction in the percentage of patients treated subsequent to a previous admission in the same structure, while direct access remained at 11% of total demand in both years. There was still significant follow-up activity within the structure that had previously carried out the revascularisation operation, despite the fact that this was characterised by a definite downward trend. As regards the other areas, Provinces 2, 3 and 9 show a prevalence of operations on patients who have already had treatment in the very same centre, of admissions through direct access, and of follow-up work mainly carried out in the same centre. With the official introduction of hierarchical planning, the three centres in Province 4 managed to circumscribe contacts to those spoke structures within the same area. A strong degree of referentiality is also seen in the case of provinces 5, 6 and 8, each of which have a 2nd level hub centre which all the other structures within the same catchment area refer to. The centres in provinces 6 and 8 increased their activity's with a consequent growth in those centres that have their own intervention centre as a point of reference for referral and follow-up operations.
Conclusion
As regards the Emilia Romagna region's approach to treatment of cardiovascular disease, the investigation carried out points to the achievement of a good degree of coordination between structures at different levels of specialisation in the case of cardiac surgery treatment. In particular, the reduction in the outward flow of patients from their own catchment areas, and the increase in the processes of transfer to and from lower level provincial structures, would seem to point to an increased sense of belonging of local centres to their own hub. This in turn would appear to indicate that those emergency service catchment areas established by the planners are increasingly matching those spontaneously defined by patient choice. Furthermore, the increase in the number of transfers carried out within the space of one day at both the referral and the follow-up stage, the reduction in direct access and discharge by the hub, together with the overall reduction in the regional mortality rate, all indicate quicker transfers and a more appropriate sharing of the various phases of care among the various members of the network.
On the other hand, the regional network for interventional cardiology consists of a number of junctions at diverse hierarchical levels which, even in recent years, has been seen to grow at both the quantitative/territorial level—i.e. in terms of the number and location of the centres—and at the qualitative/organisational level, that is, in terms of the hierarchical level. The more recent introduction of a hierarchical system within this field points to the prevalence of operations on patients who have previously been treated within the same centre, to admissions by direct access, and to follow-up that is mainly conducted in the same centre that provides initial service. Despite the progress made towards more effective rationalisation of the health care network, and above all towards its gradual strengthening in line with the epidemiological needs of the local population, it is clear that there is still room for improvement in relations between different centres, in particular with regard to the clearer definition of the roles and interdependence of those intermediate-level centres located between the hub centres and those structures providing basic healthcare facilities.
In this context, the creation of a network designed to furnish public services is neither spontaneous nor informal, but rather the result of a specific choice, made by the local planner, who manages the network hierarchically. Besides a thorough analysis of the gradual changes in the processes of selection and referral involving centres of differing complexity, which appear to be going in the hoped-for direction, our analysis points to the need for the planner to develop a systematic approach to the evaluation of the network model, whereby each area of interest has its own set of indicators to be measured and analysed on a regular basis. When the coordination of diverse decisional levels within a network is motivated by a legal mandate, it is the planner's responsibility to guide the network's member organisations in accordance with the pre-established objectives but also to verify and evaluate its functioning. In Emilia Romagna policy makers seem to have favoured only the first part of the task so far. On the contrary, the adoption of the network approach to the provision of highly-specialised hospital services should be accompanied always by the implementation of a suitable regional monitoring system designed to control the real capacity of the network to properly satisfy the requirements of demand, to achieve the network's main organisational and financial targets, and to provide the necessary incentives to those individual structures and medical professionals operating on the supply side. From this point of view, a regional planner could also consider the possibility of introducing into the context of Emilia Romagna a number of interesting organisational solutions, which an investigation into certain important international experiences points out. In particular, those solutions pertain to the degree of coordination and the transparency of waiting lists, which characterise other international examples of cardiovascular network. A good example is the Cardiac Care Network in Ontario, Canada, which, within the space of ten years, has been able to gain considerable credibility and favour with both the public, medical professionals and the international scientific community.
Acknowledgments
We are grateful to Gianluca Fiorentini, Francesco Taroni, Matteo Lippi Bruni and Roberto Grilli for their helpful comments. Thanks also go to the Agenzia Sanitaria of Emilia Romagna for kindly providing the databases used in this study.
Contributor Information
Cristina Ugolini, Department of Economics, University of Bologna.
Lucia Nobilio, Agenzia Sanitaria Regionale.
References
- 1.Robinson JC, Casalino LP. Vertical Integration and organizational networks in health care. Health Affairs. 1996;15(1):7–23. doi: 10.1377/hlthaff.15.1.7. [DOI] [PubMed] [Google Scholar]
- 2.Bazzoli GJ, Shortell SM, Dubbs N, Chan C, Kralovee P. A taxonomy of health networks and systems: bringing order out of chaos. Health Services Research. 1999;33(6):1683–718. [PMC free article] [PubMed] [Google Scholar]
- 3.Provan KG, Milward HB. Do Networks really work? A framework for evaluating public-sector organizational networks. Public Administration Review. 2001 Jul [Google Scholar]
- 4.Klazinga N, Stronks K, Delnoij D, Verhoeff A. Indicators without a cause. Reflections on the development and use of indicators in health care from a public health perspective. International Journal for Quality in Health Care. 2001;13(6):433–8. doi: 10.1093/intqhc/13.6.433. [DOI] [PubMed] [Google Scholar]
- 5.NHS. National Service Framework for Coronary Heart Disease. 2000
- 6.Plogman PL, Pine M, Reed DC, Byrwa KJ, Berman JI. Anthem Blue Cross and Blue Shield's coronary services network: a managed care organization's approach to improving the quality of cardiac care for its members. American Journal of Managed Care. 1998;4(12):1679–86. [PubMed] [Google Scholar]
- 7.Woods KJ. The development of integrated health care models in Scotland. International Journal of Integrated Care [serial online] 2001 Jun 1;1 doi: 10.5334/ijic.29. Available from: URL: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emilia Romagna Region. Regional Health Plan 1999–2001 (in Italian) Il patto di solidarietà per la salute in Emilia-Romagna; 1999. [Google Scholar]
- 9.Nobilio L, Ugolini C. Selective referrals in a hub and spoke institutional setting: the case of coronary angioplasty procedures. Health Policy. 2003;63(1):95–107. doi: 10.1016/s0168-8510(02)00080-5. [DOI] [PubMed] [Google Scholar]
- 10.Nobilio L, Ugolini C. Different regional organisational models and quality of health care: the case of coronary artery bypass graft surgery. Journal of Health Services Research & Policy. 2003;8(1):25–32. doi: 10.1177/135581960300800107. [DOI] [PubMed] [Google Scholar]
- 11.Romano P, Roos L, Jollis J. Adapting a clinical comorbidity index for use with ICD-9-CM Administrative Data: differing perspectives. Journal of Clinical Epidemiology. 1993;46(10):1075–9. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]