Abstract
Objectives
The purpose of this project was to assess the utility and feasibility of a telephone-based systematic clinical assessment service, the Behavioral Health Laboratory (BHL), in the context of primary care. The BHL is a clinical service that provides primary care providers with an assessment and a summary of mental health and substance abuse (MH/SA) symptoms and provides treatment decision support, including triage to specialty MH/SA services. The BHL was implemented to assist in the evaluation of patients who screened positively for depression at an annual clinical appointment or who were identified through routine care.
Methods
Results from systematic screening of primary care patients were extracted during a period of 6 months prior to implementation of the BHL and after implementation of the BHL. Descriptive results of the 580 evaluations conducted during this time were available.
Results
Results suggest an association between the implementation of the BHL and an increase in the proportion of patients screened for depression in primary care. In addition, there was an increase in the proportion of patients who screened positively (2.8% vs 7.0%). The BHL was successful in providing a comprehensive assessment for 78% of those referred. Significant co-occurring mental illness and substance misuse were found among those assessed.
Conclusions
Introducing the BHL into primary care was associated with an apparent change in clinical practice in primary care at the Philadelphia VA Medical Center. Not only were more patients identified, the broad-based approach of the BHL identified significant comorbidity with alcohol misuse, illicit drugs, and suicidal ideation, symptoms likely to have been missed in routine clinical practice. The BHL offers a practical, low-cost method of assessment, monitoring, and treatment planning for patients identified in primary care with MH/SA needs.
Keywords: depression, primary care, adult, elderly
The U.S. Preventive Services Task Force (USPSTF) recently affirmed that routine screening for depressive disorders in primary care settings is an important mechanism for reducing morbidity and mortality.1 However, the USPSTF is clear that screening is valuable only when assessment, treatment, and monitoring are available. Recommendations for screening in primary care acknowledge that depression is common, given that 5% to 9% of patients have a major depressive disorder, and that depression is a disabling illness leading to increased health care utilization and costs of $17 billion in lost workdays each year.1 The recommended focus on assessment recognizes the high rates of co-occurring MH conditions, while monitoring recognizes the consistently low rates of follow-up of patients in whom treatment is initiated. Indeed co-occurring problems in the primary care setting have been recognized as increasing and more relevant to patient management than in the past.2
Much of the contemporary literature on depression in primary care has focused exclusively on the management of patients exhibiting mild-to-moderate severity without complicating factors such as substance misuse or manic symptoms. Numerous studies demonstrate the benefits of a collaborative care model or disease management program for patients with a depressive disorder.3–8 These efforts are in recognition of low rates of treatment and follow-up even in the context of recognition. For instance, in 2002 quality performance measures demonstrated that only 52% of veterans who screened positive for depression had an assessment in the subsequent 6 weeks.9 Despite the efficacy demonstrated in these well-designed trials, there has been limited capacity to implement this type of model. In addition to the difficulty of financing, the research trials provided a substantial infrastructure for screening and assessing patients that is not available in most clinic settings. In these trials, the research team conducted the screening and provided initial comprehensive assessments leading to the exclusion of many patients because of co-occurring conditions such as drug or alcohol dependence or because of mild symptoms. Thus, the lack of formal comprehensive assessment across multiple domains of psychopathology can be an important barrier to implementing collaborative models and in determining the proper level of care such as watchful waiting for subsyndromal symptoms or specialty referral for severe or co-occurring disorders.
Based on experience in conducting research in primary care and at the request of primary care clinicians (PCCs), we developed a clinical service, the Behavioral Health Laboratory (BHL), to assist with providing comprehensive assessments for patients potentially in need of MH care. Additionally, the service was developed to allow ongoing monitoring of patients during the initial phases of depression treatment. The BHL functions much like a clinical radiology laboratory, such that the BHL conducts specific tests when ordered by the PCCs, interprets the results, and reports test results to the PCCs together with recommendations to assist in clinical decision making. In order to maximize generalizability, the BHL completes assessments by telephone. However, other modalities including in-person assessments or use of interactive voice-recording technology are feasible. The purpose of this paper is to describe the initial results of implementing the BHL in several VA outpatient primary care practices and to describe the costs associated with the assessments.
METHODS
Screening and Clinical Referral
Within all VA Medical Centers, screening for alcohol misuse and depression is recommended on an annual basis for all patients. The computerized medical record system tracks screening and prompts providers to complete screening. Beginning in March 2003 at the Philadelphia VAMC and associated community-based outpatient clinics (CBOCs), patients who screened for depression could be referred by their PCCs to the BHL for further assessment. The PCCs referred their patients through the use of a consult request and informed their patients that someone from the BHL would be contacting them for further assessment. The BHL served patients from 4 primary care clinics within the Philadelphia VAMC and 3 suburban CBOCs.
Procedures for Conducting the BHL Assessment
Upon receipt of the consult, the patient was registered and an initial phone call was placed within 48 hours. When the health technician (HT) reached the patient, they explained that the call was being made at the request of the PCC. A minimum of 4 attempts were made for each patient, including evening hours and at least once during a Saturday morning or early evening. After the 4th call attempt, a letter was sent requesting that the patient call to be assessed. Patients not able to be contacted were declared unable to contact (UTC) and the clinician was informed in the electronic medical record (ELM). Interviews not completed because of refusals or communication problems were also documented in the ELM. For all referrals regardless of the outcome, a response was provided to the clinician in the ELM or by fax or password protected e-mail.
Consent
As a clinical service, informed consent was not required for participation in the interviews. The procedures for conducting this review were approved by the Philadelphia VAMC Institutional Review Board (IRB).
Assessments Conducted
The assessments began with basic demographics and the blessed orientation-memory-concentration test (BOMC). The BOMC was administered to patients over the age of 54 to test for cognitive impairment. If a patient made more than 16 errors within the BOMC, the full interview was not completed, as the self-reported information would be considered unreliable.10 In cases of severe cognitive impairment, the clinician was prompted to consider further evaluation of the cognitive impairment. The remainder of the assessments conducted were the MINI International Neuropsychiatric Interview modules for mania, psychosis, panic disorder, generalized anxiety disorder, post-traumatic stress disorder (PTSD), and alcohol abuse/dependence11; the Patient Health Questionnaire-9 (PHQ-9) for depression12; current antidepressant medications; alcohol use using a 7-day time line follow-back method13; use of illicit substances; the 5-item Paykel scale for suicide ideation14 (patients were considered to have significant suicidal ideation if they answered yes to thinking about taking one's life, having made a plan, or having attempted suicide)15; history of past episodes of depression; the Medical Outcomes Study (SF-12)16; and a 4-item patient satisfaction scale.
All assessments were completed by direct entry using software designed for ease of use with simple entry screens. The BHL computer program used a variety of methods to limit input errors, including real-time range checks, limited input options, and error messages for incomplete responses.
Assessment Outcome and Characterization of Cases into Risk Categories
The computer algorithm scored all assessments. For patients who had either no or minor symptoms, the BHL report suggested ongoing monitoring and no change in treatment. For patients with minor depression (with or without current antidepressant treatment), specialty care was not recommended, but follow-up and further treatment planning by the primary care team was suggested. For patients with uncomplicated major depression, an initial course of treatment was recommended within primary care. All patients with a complex set of symptoms, such as suicidal thoughts, mania, psychosis, substance misuse, PTSD, or panic disorder, were recommended for a mental health and substance abuse (MH/SA) clinic referral. The BHL Director reviewed the reports providing an interpretation prior to sending the report to the PCC.
Depression Treatment Monitoring
For patients in whom a new prescription for an antidepressant was initiated, the BHL conducted brief follow-up assessments at 2, 6, and 9 weeks after treatment initiation. Patients identified were enrolled in the monitoring program using the initial examination as the baseline measure of depression. The assessments included the PHQ-9 and self-reporting of adverse effects and medication adherence. Reports were provided to the clinician outlining change in symptoms and recommendations to adjust or change treatment when necessary.
Medical Record Data Abstraction
Results of the depression screening clinical reminder were retrieved from the electronic medical record in an anonymous method. Only summary values for the screenings were obtainable. There was not a method for directly linking the results of the screening to those referred to the BHL; thus, the screening results were an approximation of the referral path.
Method used for Establishing Cost Estimates
For 20 consecutive consults, all activities required to complete the consults were recorded. Additional administrative time such as computer support, data management, and training was estimated by recording all BHL-related activities from the senior staff over the course of 2 weeks (a “time in motion” analysis).
Statistics
Statistical analyses were performed with SPSS Version 11.0 for Windows. Descriptive analyses included means and standard deviations for continuous variables, and frequencies for categorical variables. Unadjusted between-group comparisons of continuous and categorical baseline, and follow-up outcome variables were performed using Student's t-tests and χ2tests, respectively.
RESULTS
During the period between January and June 2004, 17,543 patients were screened using the depression clinical reminder, representing 63.8% of the unique veterans seen in primary care. Of those screened, 3,008 (17.1%) were marked as already receiving MH/SA care, while 1,232 (7.0%) screened positively. During the comparable period in 2002, 11,826 veterans were screened, representing 52.0% of the unique patients seen during that time frame. Thus, there was an 11.8% increase in the number of veterans screened from 2002 to 2004. In addition, there was a significantly greater proportion of patients who screened positive in 2004 (7.0%) compared with 2002 (2.8%) (χ2=895.8, 1 df, P<.001).
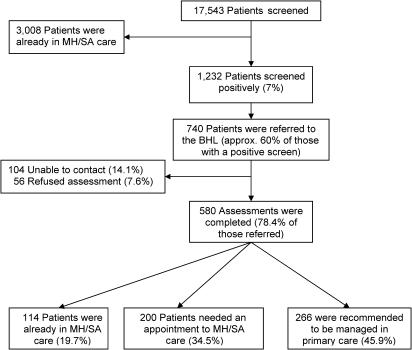
During the 6 months in 2004, 740 referrals were made to the BHL (approximately 60% of those screening positively). Of those referred, 78.4% completed the assessment, with an additional 7.6% refusing assessment and 14.1% being UTC. Older veterans were more likely to refuse assessment, and a greater proportion of younger veterans could not be contacted (F=6.40, 1 df, P<.001).Figure 1 describes the flow of patients from screening to referral.
FIGURE 1.
Patient flow from screening in the primary care clinic to assessment and referral by the Behavioral Health Laboratory.
Table 1 outlines the demographic and clinical characteristics of assessed patients. Complex cases accounted for 44% of all assessed patients. Severe cognitive impairment accounted for 5.2% of those assessed. Minor depression or distress was present in 40.5% of the cases. A self-reported past history of depression (59.5% overall) as well as significant suicidal ideation (12.9% overall) was common. Overall, only 19.7% of patients were in MH/SA care, with the majority being complex cases. However, only 23.9% of the complex group was in MH/SA care. Altogether, 261 patients had significant symptoms warranting specialty MH/SA care either because of significant suicidal ideation or presence of complex symptoms. In terms of the complex cases, 67 met criteria for alcohol dependence (11.6% of the total assessed sample), 44 used illicit drugs other than marijuana (7.6%), 128 met criteria for PTSD (22.1%), 51 had manic symptoms (8.8%), 86 had possible psychotic symptoms (14.8%), and 26 met criteria for current panic disorder (4.5%).
Table 1.
Characteristics of Patients Interviewed by the BHL
| Total,N=580 | Severe Cognitive Impairment (N=30) | Complex (N=255) | MDD Only (N=60) | Minor Depression+Antidepressant (N=28) | Minor Depression no Antidepressant (N=54) | Distressed Only (N=153) | Test Statistic | P | |
|---|---|---|---|---|---|---|---|---|---|
| % of total | 100.0 | 5.2 | 44.0 | 10.3 | 4.8 | 9.3 | 26.4 | ||
| Age | 56.5 (13.2) | 67.9 (9.9) | 53.1 (12.8) | 54.7 (12.8) | 56.3 (16.2) | 57.8 15.1) | 60.3 (15.0) | F=11.86 | <.001 |
| Gender (%male) | 94.8 | 100.0 | 96.5 | 91.7 | 89.3 | 94.4 | 93.5 | χ2=6.61 | .251 |
| Married (%yes) | 35.3 | 33.3 | 33.3 | 43.3 | 17.9 | 39.6 | 37.5 | χ2=6.66 | .247 |
| Race (%White) | 44.4 | 46.4 | 33.8 | 36.8 | 63.0 | 40.0 | 62.6 | χ2=36.23 | <.001 |
| Past Hx depression | 59.5 | N/A | 75.9 | 67.8 | 74.1 | 54.7 | 27.8 | χ2=95.67 | <.001 |
| In MH care (last 12 mo) | 19.7 | 16.7 | 23.9 | 23.3 | 32.1 | 9.3 | 13.1 | χ2=13.05 | .023 |
| On antidepressant | 37.3 | 39.6 | 43.3 | 33.3 | 34.1% overall for minor depression | 32.9 | χ2=3.12 | .373 | |
| PHQ total score | 12.6 (6.7) | N/A | 17.0 (5.4) | 15.4 (2.1) | 10.6 (2.1) | 10.9 (2.4) | 5.1 (3.9) | F=187.34 | <.001 |
| Disability from depression (1 not at all to 4 extremely) | 2.13 (0.89) | N/A | 2.53 (0.83) | 2.40 (0.81) | 2.14 (0.84) | 1.87 (0.67) | 1.44 (0.60) | F=52.27 | <.001 |
| High-risk suicide | 12.9 | N/A | 24.7 | 6.7 | 3.6 | 1.9 | 3.9 | χ2=57.05 | <.001 |
| Smokes | 44.0 | 33.3 | 54.1 | 46.7 | 32.1 | 29.6 | 35.3 | χ2=22.99 | <.001 |
BHL, Behavioral Health Laboratory; MH, mental health; PHQ, Patient Health Questionnaire; MDD, Major depressive disorder.
The depression monitoring program identified 13 patients with newly prescribed antidepressants. Of these patients, 12 completed at least 2 follow-up assessments. Reports were given to the clinician indicating change in depressive symptoms, adverse events, and adherence.
Clinician acceptance was measured using a series of focus groups with each primary care practice, except one which was unavailable to meet. Feedback was invited with discussion for improving the services. In all instances, providers commented on the rapid turnaround in assessment time, the identification of symptoms other than depression, positive comments from patients about the BHL staff, and improved access to behavioral health. Providers have been particularly positive about the depression-monitoring program. Negative comments focused mostly on the formatting of reports, desire for a face-to-face component, and desire to refer more patients to the MH/SA clinic. The success of the program led to the use of the BHL as the single point of entry for outpatient MH/SA care.
Cost estimates were calculated first for bachelor's level HTs. The core baseline assessment takes an average of 30 minutes for the interview, with an additional 30 minutes of scheduling appointments, filing, sending a letter to patients, and sending the report to the provider. Additional depression monitoring assessments take 30 minutes of the HT's time. Time for administrative and quality management activities, including training and supervision, is estimated at 60 minutes/day or 5 hours/week. Vacation/holiday/break time is 7.2 hours/weeks. Thus, there is approximately 27 hours (40 hours −(5+7.2)) available to conduct interviews. An HT salary is $36,092 with benefits or $695/week. Thus, the cost per unit for initial evaluations is $695/27 or $25.74. The cost per unit for depression monitoring assessments is $695/54 or $12.87.
Ongoing staffing for laboratory operations includes 0.20 FTE for the Medical Director, 0.30 FTE for the Behavioral Health Specialist, 0.3 FTE for the HT Coordinator, and 0.1 Full Time Eqivalent (FTE) for IT support. These costs represent the fixed costs for maintaining the laboratory as an entity and are estimated based on the amount of administrative support required for every 5 HTs. Other expenses include computer upgrades, software license, supplies, and a toll free number. These are estimated at $6,250/year or $120/week/HT. In total, the administrative costs translate into $527/week/HT. This corresponds to approximately $19.52/initial assessment or $12.26/follow-up assessment. Thus, the total costs are approximately $45.26/initial assessment and $25.13/follow-up assessment.
DISCUSSION
Recent media and Food and Drug Administration reports underscored the importance of systematic assessments, including assessment of suicidal ideation and co-occurring MH problems during the initiation of depression treatment.17 It is especially important to consider models of care that assist in the delivery of depression care in primary care settings, as nationally, 37.3% of veterans with depression are managed solely in primary care.18 As described in this paper, the BHL offers a practical and face-valid method of providing assessment and monitoring for almost all MH/SA problems and not just for selected patients. Moreover, the use of HTs rather than clinical staff, and telephone rather than face-to-face assessment, led to the relatively low cost of each assessment. The cost of a single BHL assessment is lower than the clinical laboratory evaluation typical of a diabetic patient (lipid profile $18.72, Hemoglobin A1c $18.33, and chemistry profile $19.96—based on Medicare reimbursement). These results also suggest that the BHL can be implemented across geographically distinct primary care practices.
Implementation of the BHL was associated with a significant increase in screening and identification of patients needing MH/SA services. While this association was evident over the 2 years of implementation, other factors may have also contributed to the improvement in screening. Other evidence for the success of this model includes the substantial number of patients with complex MH/SA needs identified and referred for care who were not previously engaged in specialized treatment. Moreover, in providing decision support for those patients with less severe symptoms, the BHL assisted in prioritizing patients for appropriate use of specialty MH/SA services, resulting in a potential reduction in health care costs and patient burden. This finding is consistent with the management of other chronic diseases, such as diabetes or hypertension, which are managed in primary care settings, unless the illness is complex and therefore referred for management in a specialty setting.
The BHL also offers the possibility of ongoing monitoring for those patients requiring treatment. Monitoring patients solely by telephone should not replace face-to-face clinical management; however, telephone monitoring can provide systematic assessments at a relatively low cost and low burden to the patient and highlight special circumstances such as missed appointments, low adherence, and emerging suicidality. This practice increases the efficiency and effectiveness of care consistent with results of face-to-face disease management or quality improvement programs.19 Monitoring can also be an effective mechanism for following patients with subsyndromal depression to distinguish those with ephemeral symptoms (false positive screens) from those with persistent symptoms that may require formal treatment. Moreover, the BHL can easily integrate with care management programs or referral management programs. Indeed the BHL may be ideally suited for determining which patient should be triaged to specialty care and which patient could be sent to care management.
There are several limitations to note in understanding the results. First, the study was conducted in a VA medical center and associated outpatient clinics. The population is different from most community-based primary care practices with a higher prevalence of MH/SA problems. However, this may underestimate the value of the BHL, in the sense that there would be fewer expected false positive screens in a VA setting. Moreover, given the higher prevalence of MH/SA problems, the VA may be the one health care system that can justify the costs of having behavioral health specialists integrated in all primary care practices. Veterans also have access to MH/SA services at no or limited cost. Again, this may underestimate the role of the BHL as non-VA settings may value BHL services more because of limited access to specialty care.
This study was conducted as a clinical demonstration project, not as a randomized effectiveness trial. The use of historical data for screening allows for the possibility that changes in the process of screening are related to unmeasured variance, rather than the introduction of the BHL. Finally, there may be concern that evaluating complex illnesses such as depression, mania, and psychosis cannot be adequately completed by telephone or by nonclinicians. However, several studies have compared telephone assessments with face-to-face interviews and have found that telephone interviews can be equally as effective and valid as face-to-face interviews.20–30 Telephone interviews can be more efficient, in both time and logistically, than face-to-face interviews.
In summary, the initial experience with the BHL appears to provide a platform to address many of the difficulties in managing depression and other MH problems in primary care settings. Specifically, the BHL allows for a rapid and systematic assessment of patients with possible behavioral health needs. Particularly important was the identification of co-occurring problems often missed or excluded in trials that focus specifically on depression. The BHL can also function as an adjunct to managing patients started on treatment in a manner consistent with treatment guidelines. Consequently, the BHL can overcome some of the problems in delivering quality MH care, such as the already heavy demand on clinician time, availability of clinicians to conduct brief but frequent follow-up assessments, and the demand on patients for attending frequent follow-up visits. Given the low burden for implementation and the ease of integration into existing primary care practice, the BHL offers a tool for improving the efficiency of managing depression and other MH problems common in primary care settings.
Acknowledgments
This work was supported, in part, by a grant from the National Institute of Mental Health K08MH01599 & P30 MH66270, National Institute of Alcohol Abuse and Alcoholism R01, Department of Veterans Affairs HSRD Investigator Initiated Research IIR 02-108, and the Mental Illness Research, Education, and Clinical Center (MIRECC) at the Philadelphia VAMC. The success of the BHL would not be possible without the dedication of the primary care staff at the Philadelphia VAMC. The staff clearly values the integration of behavioral health in the daily routine of primary care. We also want to acknowledge the help of Joyce Askew who was invaluable in developing the depression clinical reminder for the electronic record and extracting data from the electronic record.
References
- 1.Agency for Healthcare Research and Quality. U.S. Preventive Services Task Force Now Finds Sufficient Evidence to Recommend Screening Adults for Depression. Rockville, Md: Agency for Healthcare Research and Quality; 2002. [Google Scholar]
- 2.Frisher M, Collins J, Millson D, Crome I, Croft P, et al. Prevalence of comorbid psychiatric illness and substance misuse in primary care in England and Wales. J Epidemiol Community Health. 2004;58:1036–41. doi: 10.1136/jech.2003.017384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruce ML, Ten Have TR, Reynolds CF., III Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–91. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 4.Levkoff SE, Chen H, Coakley E, et al. Design and sample characteristics of the PRISM-E multisite randomized trial to improve behavioral health care for the elderly. J Aging Health. 2004;16:3–27. doi: 10.1177/0898264303260390. [DOI] [PubMed] [Google Scholar]
- 5.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–45. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 6.Simon GE, Korff M, Ludman EJ, et al. Cost-effectiveness of a program to prevent depression relapse in primary care. Med Care. 2002;40:941–50. doi: 10.1097/00005650-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Simon GE, Katon WJ, VonKorff M, et al. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. Am J Psychiatry. 2001;158:1638–44. doi: 10.1176/appi.ajp.158.10.1638. [DOI] [PubMed] [Google Scholar]
- 8.Oslin DW, Sayers S, Ross J, et al. Disease management for depression and at-risk drinking via telephone in an older population of veterans. Psychosom Med. 2003;65:931–7. doi: 10.1097/01.psy.0000097335.35776.fb. [DOI] [PubMed] [Google Scholar]
- 9.Department of Veterans Affairs. FY2002 end of year network performance measure report, 2002. [Google Scholar]
- 10.Blessed G, Tominson BE, Roth M, et al. The association between quantitative measures of dementia and of senile change in the cerebral gray matter. Br J Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- 11.Sheehan DV, Lecrubier Y, Sheehan K, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(suppl 20):22–33. [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JB, et al. The PHQ-9: validity of a brief depression severity measure. J Gen Internal Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sobell L, Sobell M, Gloria L, Cancilla A, et al. Reliability of a timeline method: assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. Br J Addiction. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- 14.Paykel ES, Myers JK, Lindenthal JJ, Tanner J, et al. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124:460–9. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 15.Bartels SJ, Coakley E, Oxman TE, et al. Suicidal and death ideation in older primary care patients with depression, anxiety, and at-risk alcohol use. Am J Geriatric Psychiatry. 2002;10:417–27. [PubMed] [Google Scholar]
- 16.Ware J, Kossinski M, Keller S, et al. How to score the SF-12 (R) pyshical and mental health summary scales. 3rd. Lincoln, RI: QualityMetric Incorporated; 1998. [Google Scholar]
- 17.Food and Drug Administration. 2004. Worsening depression and suicidality in patients being treated with antidepressant medications. [Google Scholar]
- 18.Department of Veterans Affairs. 2004. Unique SSN's with a Dx of depression in FY 2004 followed by primary care and/or mental health clinics. [Google Scholar]
- 19.Wells KB, Sherbourne C, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283:212–20. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- 20.Revicki DA, Tohen M, Gyulai L, et al. Telephone versus in-person clinical and health status assessment interviews in patients with bipolar disorder. Harv Rev Psychiatry. 1997;5:75–81. doi: 10.3109/10673229709034730. [DOI] [PubMed] [Google Scholar]
- 21.Williams S, Crouch R, Dale J, et al. Providing health-care advice by telephone. Prof Nurse. 1995;10:750–2. [PubMed] [Google Scholar]
- 22.Kawas C, Karagiozis H, Resau L, Corrada M, Brookmeyer R, et al. Reliability of the blessed telephone information-memory-concentration test. J Geriatr Psychiatry Neurol. 1995;8:238–42. doi: 10.1177/089198879500800408. [DOI] [PubMed] [Google Scholar]
- 23.Greist JH, Jefferson JW, Wenzel KW, et al. The telephone assessment program: efficient patient monitoring and clinician feedback. MD Comput. 1997;14:382–7. [PubMed] [Google Scholar]
- 24.Sobell LC, Brown J, Leo GI, Sobell MB, et al. The reliability of the alcohol timeline followback when administered by telephone and by computer. Drug Alcohol Depend. 1996;42:49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- 25.Rohde P, Lewinsohn PM, Seeley JR, et al. Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry. 1997;154:1593–8. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- 26.Coon GM, Pena D, Illich PA, et al. Self-efficacy and substance abuse: assessment using a brief phone interview. J Subst Abuse Treat. 1998;15:385–91. doi: 10.1016/s0740-5472(97)00285-7. [DOI] [PubMed] [Google Scholar]
- 27.Simon GE, Revicki D, VonKorff M, et al. Telephone assessment of depression severity. J Psychiatric Res. 1993;27:247–52. doi: 10.1016/0022-3956(93)90035-z. [DOI] [PubMed] [Google Scholar]
- 28.Simpson J, Doze S, Urness D, Hailey D, Jacobs P, et al. Telepsychiatry as a routine service—the perspective of the patient. J Telemed Telecare. 2001;7:155–60. doi: 10.1258/1357633011936318. [DOI] [PubMed] [Google Scholar]
- 29.Pulier ML, Ciccone DS, Castellano C, Marcus K, Schleifer SJ, et al. Medical versus nonmedical mental health referral: clinical decision-making by telephone access center staff. J Behav Health Serv Res. 2003;30:444–51. doi: 10.1007/BF02287431. [DOI] [PubMed] [Google Scholar]
- 30.Gatz M, Reynolds CA, John R, Johansson B, Mortimer JA, Pedersen NL, et al. Telephone screening to identify potential dementia cases in a population-based sample of older adults. Int Psychogeriatr. 2002;14:273–89. doi: 10.1017/s1041610202008475. [DOI] [PubMed] [Google Scholar]