Abstract
BACKGROUND
Prior studies found higher hospitalization rates among patients with low literacy, but did not determine the preventability of these admissions or consider other determinants of hospitalization, such as social support. This study evaluated whether low literacy was a predictor for preventability of hospitalization when considered in the context of social support, sociodemographics, health status, and risk behaviors.
METHODS
A convenience sample of 400 patients, admitted to general medicine wards in a university-affiliated Veterans Affairs hospital between August 1, 2001 and April 1, 2003, completed a face-to-face interview to assess literacy, sociodemographics, social support, health status, and risk behaviors. Two Board-certified Internists independently assessed preventability of hospitalization and determined the primary preventable cause through blinded medical chart reviews.
RESULTS
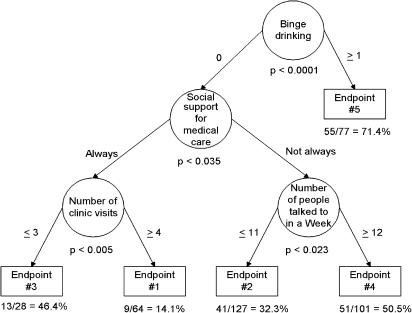
Neither low literacy (<seventh grade) nor very low literacy (<fourth grade) was significantly associated with preventability of hospitalization. In multivariable analysis, significant predictors of having a preventable cause of hospitalization included binge alcohol drinking (P≤.001), lower social support for medical care (P<.04), ≤3 annual clinic visits (P<.005), and ≥12 people talked to weekly (P<.023). Among nonbinge drinkers with lower social support for medical care, larger social networks were predictive of preventability of hospitalization. Among nonbinge drinkers with higher support for medical care, lower outpatient utilization was predictive of the preventability of hospitalization.
CONCLUSIONS
While low literacy was not predictive of admission preventability, the formal assessment of alcohol binge drinking, social support for medical care, social network size, and prior outpatient utilization may enhance our ability to predict the preventability of hospitalizations and develop targeted interventions.
Keywords: health literacy, social support, hospital medicine, veterans, preventable admission
An estimated 90 million American adults have difficulty in understanding and acting upon health information because of limited health literacy.1 Previous studies found that patients with low literacy tend to misunderstand medical instructions,2–5 miss routine physician appointments,6, 7 have worse health status,6, 8 and use more hospital services.9, 10 Health care costs associated with low literacy are estimated at $8 to $12 billion per year, and are primarily attributable to excess hospitalizations.11 Prior research reported that low literacy was associated with higher hospitalization rates,9, 10 but did not assess the preventability of hospitalizations, or consider other possible determinants of hospitalization such as social support.12 Addressing these concerns, we investigated the association between preventability of hospitalization and health literacy, social support, sociodemographics, health status, and risk behaviors.
METHODS
Setting and Patients
The study was conducted at the Jesse Brown Veterans Affairs Medical Center (VAMC), which serves as a major teaching hospital for the University of Illinois and Northwestern University medical schools. The Jesse Brown VAMC has 6 inpatient general medicine wards with 300 to 400 admissions each month. Approximately 95% of inpatients are male, and 80% are African American, 10% are white, and 10% are Latino. The University of Illinois at Chicago Institutional Review Board and the Jesse Brown VAMC Research and Development Committee approved the study.
A convenience sample of general medicine inpatients admitted between August 1, 2001 and April 1, 2003 were enrolled. Patients with severely impaired vision were excluded because the literacy assessment involved a visually administered test. Other exclusion criteria included age <18 years, dementia, deafness, or hearing problems uncorrectable with a hearing aid, having received care at Jesse Brown VAMC for less than 6 months prior to hospitalization, transfers from the intensive care unit or an outside hospital, being admitted as “observation status” for <24 hours, being too ill to participate, and/or English as a second language. Eligible patients were approached during their hospitalization, and informed consent was obtained using both written forms and verbal explanations. Once enrolled, patients were not reinterviewed on subsequent admissions occurring within the study period.
Patient Interviews and Literacy Assessment
During the hospitalization, each patient completed a 45-minute face-to-face interview to assess literacy level, social support, sociodemographics, marital status, health status, health risk behaviors, and health service access and utilization. The rapid estimate of adult literacy in medicine (REALM-66), which has been used previously with hospitalized patients,13 was used to assess literacy. Personnel with minimal training can administer and score the REALM-66 in 3 to 5 minutes with a test-retest reliability of 0.99.14 The REALM-66 has excellent correlations (0.88 to 0.97) with 3 other general reading tests, and scores can be transformed into reading grade levels.14, 15
Patients described their social support structure by reporting the number of people they talk to in a typical week and the number of club and organization memberships.16 Functional social support was evaluated using the medical outcomes study social support questionnaire that includes subscales assessing tangible, affectionate, positive interaction, and emotional/informational support with subscale α's=0.92, 0.91, 0.94, and 0.96, respectively, and test-retest reliability at 1 year ranging from 0.72 to 0.76.17 Patients described social support for medical visits by stating how often someone accompanied them to the hospital or doctor when they have health problems (all, most, some, a little bit, or none of the time).
Patients classified their own race, Hispanic or Latino ethnicity, current marital status, highest level of education completed, and annual household income. Self-rated health status was measured using the 12-item Short Form Health Status Survey (SF-12), providing standardized physical and mental component scores.18
Patients were queried about health habits, alcohol, tobacco, and seatbelt use. The health-promoting lifestyle profile (HPLP) was administered to assess health responsibility, exercise, and nutrition habits with subscale α's=0.81, 0.80, and 0.76, respectively, and a test-retest reliability ranging from 0.81 to 0.91.19 Patients reported the number of binge drinking episodes, defined as 5 or more alcoholic beverages on 1 occasion, in the previous 30 days.
Health care utilization was assessed through patient reports of clinic visits, emergency room visits, and hospitalizations in the previous year, use of non-VA medical care, and timing of most recent routine physical examination. Patients reported satisfaction level with VA medical care, degree of inability to seek care because of cost, presence of a personal doctor, and degree of communication difficulty with physicians and nurses. Medication adherence was assessed by asking patients how often they filled prescriptions in a timely fashion, followed medication instructions, and forgot to take medications.
Preventability of Hospitalization Assessment
Oddone et al.20 developed and validated a medical chart review process to assess the preventability of hospitalizations. Following their protocol, individual charts were compiled from electronic medical records including: (1) all inpatient and outpatient notes from 1 month prior to the current admission; (2) outpatient clinic notes, emergency department notes, and all histories and physicals from the day of admission; and (3) admitting nursing evaluations, admitting orders, and any laboratory or radiology reports available within 24 hours of admission.20 Each chart was blinded to patient name, social security number, and all provider names. Although charts were not blinded for descriptions of patient literacy or education level, a 10% random sample of charts revealed no documented descriptions of patient literacy or education level.
Two Board-certified general Internists (J.R., M.B.) independently reviewed each chart after completing formal training sessions, including a test of 10 sample charts. Chart reviewers were blinded to patient interview results. Using a standardized abstraction form,20 reviewers independently rated the preventability of the hospitalization as definitely not preventable (0%), most likely not preventable (25%), possibly preventable (50%), most likely preventable (75%), or definitely preventable (100%). A priori, we decided against arbitrating potential differences between reviewers because the arbitration process often diminishes the independence of the 2 reviewers unless it is done consistently for all cases. Therefore, reviewers' assessments were averaged, and the hospitalization was classified as “preventable” if the mean percent preventable was ≥50% or as “not preventable” otherwise. For each preventable admission, the reviewers also assessed the primary preventable cause by completing the statement, “this admission could have been prevented if …”
Statistical Analysis
Bivariate associations between measured attributes and preventability of admission were assessed using univariate optimal discriminant analysis, or UniODA,21–24 conducted using Optimal Data Analysis software.24 For nominal data, UniODA is identical to Fisher's exact test. For ordered attributes, UniODA identifies the cutpoint that maximizes classification accuracy in predicting the outcome of interest; regardless of metric an exact permutation P-value is computed. Effect strength for sensitivity (ESS) is used to quantify the strength of association between an attribute and preventability. ESS represents the percent of theoretical improvement in classification accuracy over chance that an attribute provides, and is bounded between 0 (classification accuracy expected by chance) and 100 (perfect, errorless classification). For all analyses, the upper-bound of cross-generalizability was estimated via jack-knife validity analysis.
Hierarchically optimal classification tree analysis (CTA), also conducted using optimal data analysis software, was used to construct a nonlinear “tree” model for predicting preventability.25, 26 While linear models (e.g., logistic regression) can be used to control for potential confounding by other attributes, they do not readily detect potentially complex interactions between attributes. Accordingly, we used nonlinear CTA specifically because it allows different risk factors to classify different patient subgroups, allows a risk factor to be negatively predictive for 1 subgroup and positively predictive for another, and allows attributes to have different cutpoints for different subgroups.23, 25, 26 The CTA model required attributes to be jack-knife–stable in order to promote cross-generalizability, and was pruned to ensure an experiment-wise type I error rate of P<.05 using a sequentially rejective Bonferroni's procedure. Bootstrap validity analysis (10,000 iterations of a 50% resample) was performed on the final CTA model to estimate cross-generalizability to an independent random sample.
RESULTS
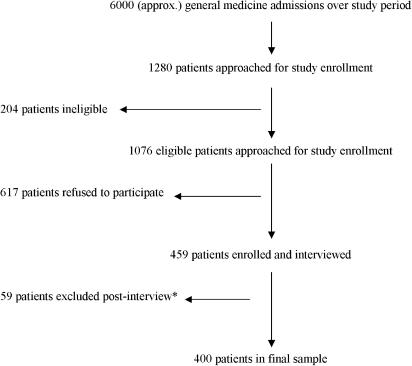
Of the approximately 6,000 admissions occurring within the study period, we approached 1,280 patients, of whom 1,076 were initially eligible, with 459 consenting and completing interviews (Fig. 1). However, postinterview medical chart reviews revealed that 59 of these 459 patients (13%) were ineligible because they were initially admitted to the intensive care unit, surgical service, or were under observation status. Assuming a 13% ineligibility rate among nonparticipants, the 400 patients used in our analyses represent a 43% response rate among eligible patients (400 out of 936 eligible patients). Nonparticipants were significantly older (mean 67 vs 60 years, P<.001) than participants, with no significant differences in gender or race/ethnicity.
FIGURE 1.
Patient recruitment and exclusions. *These 59 patients were excluded because postinterview medical chart reviews revealed that they were initially admitted to intensive care units, surgical services, or as observation status for less than 24 hours.
The mean age of our sample was 60.5 years; 99% were male and 84% were African American. Over half (58%) of the patients had less than ninth-grade literacy, 7% had less than fourth-grade literacy, and 25% did not complete high school. Nearly half (47%) spoke with 12 or more people weekly and 28% always had social support for medical care. One third of the patients had 3 or fewer clinic visits in the previous year, and 19% reported 1 or more recent alcohol binge episodes. Two blinded reviewers found that 43% of admissions were preventable with interrater agreement for preventability of 75% (κ=.48, P<.0001).
Literacy level, regardless of cutpoint, was not significantly associated with preventability of admission (P<.70) (Table 1). For the entire sample, younger age, alcohol binge drinking, cigarette use, forgetting medication, not always following medication instructions, and fewer organizational memberships were significantly associated with higher preventability of admission (P<.05) and were stable in jack-knife validity analysis. Lower SF-12 mental component score, 3 or fewer prior clinic visits, and not always having social support for medical care were also significantly associated with higher preventability of admission, but were unstable in jack-knife validity analysis. The instability suggests that these 3 attributes would be predictive of preventability in independent random samples, but using different cutpoints that were optimized for the new sample. All other measured attributes were not significantly associated (P>.05) with preventability of hospitalization.
Table 1.
Selected Patient Characteristics by Preventable Hospitalization
| Variables | Not Preventable (n=230)† | Preventable (n=170)† | P< | ESS‡ |
|---|---|---|---|---|
| Age | 61.5 (13.6) | 59.2 (12.4) | .05 | 13.0 |
| SF-12 mental component score* (0 to 100) | 51.8 (11.6) | 46.9 (13.1) | .002 | 19.2 |
| Body mass index* (kg/m2) | 27.1 (6.2) | 25.8 (6.3) | .06 | 13.0 |
| Literacy level | .70 | 3.6 | ||
| >Eighth grade | 43.5 | 40.6 | ||
| Seventh to eighth grade | 33.0 | 33.5 | ||
| Fourth to sixth grade | 18.3 | 17.1 | ||
| <Fourth grade | 5.2 | 8.8 | ||
| At least 1 binge drinking episode in past 30 d | 9.6 | 32.4 | .001 | 22.8 |
| Cigarette use | 35.6 | 52.3 | .002 | 16.7 |
| Factors related to health care utilization | ||||
| Greater than 3 clinic visits in past year* | 72.6 | 58.2 | .003 | 16.7 |
| At least 1 person as personal doctor | 47.0 | 37.1 | .053 | 9.9 |
| VA able to serve all medical needs | 91.7 | 85.3 | .052 | 6.4 |
| Factors related to medication adherence | ||||
| Forgot to take medication | .02 | 12.3 | ||
| All, most, or some of the time | 19.7 | 31.0 | ||
| A little or none of the time | 81.3 | 69.0 | ||
| Always follow medication instructions | 82.6 | 71.0 | .007 | 11.6 |
| Factors related to social support | ||||
| Always have social support for medical care* | 33.5 | 20.6 | .02 | 12.9 |
| Club or organizational memberships | 0.7 (1.2) | 0.6 (1.7) | .02 | 11.6 |
| People talked to in typical week | 13.3 (10.6) | 12.8 (11.3) | .18 | 10.0 |
Variables had an ESS that was lower in jack-knife validity analysis compared with training analysis, suggesting that the level of classification accuracy in training may not cross-generalize when it is used to classify an independent random sample using the cutpoints or category assignments reported presently.
Summary values given are percentages or means and standard deviation in parentheses. Data presented as percentages are the number of patients with the characteristic divided by the N for that variable.
ESS, effect strength for sensitivity is a standardized measure of classification accuracy, where 0=accuracy expected by chance, and 100=perfect, errorless classification.
ESS, Effect strength for sensitivity.
Using 4 attributes, CTA analysis identified 5 patient subgroups (model endpoints) that were numbered to reflect an increasing likelihood of preventability (Fig. 2). Among nonbinge drinking patients who reported not always having social support for medical care (n=228, 57% of total sample), those who spoke with ≥12 people weekly were more likely to have a preventable cause of hospitalization than those who spoke with <11 people weekly (51% vs 32%, P<.023). Among nonbinge drinking patients who always had social support for medical care (n=92, 23% of total sample), those with 3 or fewer prior clinic visits had a 3-fold higher likelihood of having a preventable cause of admission compared with patients with 4 or more prior clinic visits (46% vs 14%, P<.005). Literacy level, regardless of cutpoint, was not significantly predictive of preventability of admission for any model endpoint, even when binge drinking was not included in the model.
FIGURE 2.
Schematic illustration of the classification tree analysis model for predicting preventable admission. Circles represent nodes (decision points), ars indicate branches (decision paths), and rectangles represent prediction end points. The generalized type I error is given by the numbers underneath each node. Numbers/words adjacent to ars indicate the value of the cutpoint or category for each node. End points are numbered from 1 to 5 based on increasing proportions of hospitalizations that were preventable (vs nonpreventable). Percentage of total sample classified by each attribute: binge drinking (N=397, 99.3%), social support for medical care (N=320, 80.0%), number of people talked to in a week (N=228, 57.0%), number of prior clinic visits (N=92, 23.0%).
The CTA model classified 397 out of 400 patients (99%) because 3 patients were missing data required on their model branch. The CTA model yielded a moderate effect size of ESS=32.3, indicating that the model provided 32.3% of the classification improvement theoretically possible to achieve beyond chance.24 All model performance indices and endpoint-predictive values were closely approximated in bootstrap validity analysis, suggesting model stability.
For admissions judged to be preventable, chart reviewers found that common preventable reasons included medication nonadherence (30%), alcohol or drug use (25%), and lack of physician assessment and/or change in therapy within 2 weeks of admission (22%) (Table 2). The reviewers attributed 55% of preventable admissions among binge drinking patients (end point 5) to alcohol or drug use and 35% of preventable admissions among nonbinge drinking patients (end points 1 to 4) to medication nonadherence.
Table 2.
Primary Preventable Reasons for Hospital Admission*
| Model End point | Medication Nonadherence (%) | Alcohol or Drug Use (%) | Lack of Recent Assessment or Therapy Change (%) | Outpatient Services not Available (%) | Low Admission Threshold (%) | Lack of Home Support (%) |
|---|---|---|---|---|---|---|
| 1 | 45.5 | 4.5 | 27.3 | 13.6 | 4.5 | 0 |
| 2 | 38.5 | 11.5 | 25.8 | 9.0 | 7.8 | 2.6 |
| 3 | 47.6 | 9.5 | 23.8 | 9.5 | 4.5 | 4.5 |
| 4 | 27.8 | 11.4 | 25.3 | 26.6 | 1.3 | 3.8 |
| 5 | 17.7 | 55.2 | 13.5 | 7.3 | 3.1 | 1.0 |
| Overall | 30.1 | 25.0 | 21.6 | 13.5 | 4.1 | 2.4 |
Medical chart reviewer ratings of the primary reason that could have prevented the hospital admission. Percentages given are the number of reviewer ratings divided by the total number of ratings for that model end point.
DISCUSSION
Prior studies found higher hospitalization rates among patients with inadequate literacy,9, 10 but did not consider whether these hospitalizations were preventable. We found that low literacy, defined as less than fouth-, seventh-, or ninth-grade level, was not directly associated with preventability of hospitalization. One potential explanation for the lack of association in this study is that prior studies did not account for social support resources.12 Prior studies found that social support was an independent predictor of hospital utilization,27–30 including 1 study in which older, socially isolated, male veterans were 4 to 5 times more likely to be re-hospitalized within 1 year.31 Social support resources may also alleviate the adverse effects of low literacy by facilitating health care use, providing health information, and supporting healthy behaviors.12, 30, 32
We found that hospitalizations among patients who always had social support for medical care, defined as having someone accompany them to the hospital or doctor, were 52% less likely to be preventable (31% vs 47%). Furthermore, patients with <seventh-grade literacy were significantly more likely than patients with ≥seventh-grade literacy to report always having social support for medical care (37% vs 25%). These findings suggest that social support for medical care may reduce the stress of dealing with the health care system for some patients with low literacy and may thereby lead to a reduction in preventable hospitalizations.
Although social support is generally considered a positive influence on health care utilization, patients who interacted with 12 or more people weekly were more likely to have a preventable cause of hospitalization. This unexpected relationship was detected by the CTA model among nonbinge drinkers who reported not always having social support for medical care. Patients in this subgroup may rely on advice and support from their larger structural networks in lieu of seeking care in formal health care settings. These results imply that future studies should explore how social support resources are used by individuals and not simply assess the presence or absence of social support.
A second possible explanation for the lack of association between low literacy and preventability is that binge alcohol drinking, a significant risk factor for higher preventability, was less common among patients with <seventh-grade literacy (17% vs 26%). The effect strength of the CTA model decreased from 32.3 (moderate effect) to 12.1 (weak effect) when binge drinking was excluded, implying that it was a critical predictor of having a preventable cause of hospitalization. Higher health care utilization among binge drinkers may be secondary to unintentional injuries, motor vehicle crashes, alcohol poisoning, gastritis, pancreatitis, and poor control of diabetes.33 However, even brief physician advice to reduce alcohol consumption can reduce binge drinking episodes by 40%, leading to lower hospital utilization.34 Our results strongly support efforts to reduce binge drinking through screening and treatment.35–37
A third possible explanation for the lack of association between low literacy and having a preventable cause of hospitalization is that greater outpatient utilization (clinic visits) was associated with a lower likelihood of a hospitalization having been preventable. In contrast to studies relating literacy to inpatient utilization, prior studies found that literacy was not associated with outpatient utilization.7, 38 Therefore, the lack of association with low literacy may reflect the prominent role that prior outpatient utilization plays in preventing hospitalization.
A fourth possible explanation for the lack of association between low literacy and preventability was the relatively small proportion of patients with very low literacy in our sample. Prior studies found that detrimental effects on health care utilization were particularly evident in patients with <fourth-grade literacy.1 Although our sample was comparable with prior studies with nearly 25% of patients with <seventh-grade literacy, only 7% had <fourth-grade literacy. Based on our actual sample size, the statistical power to detect a 14% difference in preventability with α=0.05 was 90% for <ninth-grade literacy, 81% for <seventh-grade literacy, and 40% for <fourth-grade literacy.
There were several limitations to this study, including restricted generalizability of the findings because the sample was from 1 university-affiliated, urban VA hospital. One major advantage of studying preventability of hospitalizations in the “equal-access” VA health care system is that patients have universal insurance coverage for medications, inpatient, and outpatient care. Patients using only VA health care had similar preventability to patients reporting non-VA health care use. Second, our results may not generalize to the high-risk population of patients who use English as their second language. Third, nonparticipants in our study were significantly older than participants. Although older patients were less likely to be hospitalized for preventable reasons in our sample, older nonparticipants may have had lower literacy and lower social support compared with participants. Therefore, nonrespondent bias may have led us to underestimate the impact of low literacy and low social support on preventability of hospitalization in our sample. Fourth, self-reported health habits and prior health care utilization may be susceptible to patient recall bias. We found that the correlation between self-reported utilization and VA administrative records was r=0.55 (P<.001) for hospitalizations, r=0.38 (P<.001) for outpatient visits, and r=0.30 (P<.001) for emergency room visits. Furthermore, blinded chart reviewers rated 55% of preventable admissions among binge drinkers as secondary to alcohol or drug use, and rated the majority of preventable admissions among patients who reported forgetting medications as secondary to medication nonadherence. Finally, although medical charts were blinded to patient name, social security number, and provider names, they were not blinded to education or literacy level. However, reviewing a 10% random sample of charts revealed no documented education or literacy levels.
CONCLUSION
When considered on a population basis, reducing hospitalizations by only 4.7% could save $5.1 billion annually.39 In this study of general medicine inpatients admitted to an urban, university-affiliated VA hospital, low literacy was not independently associated with preventability of hospitalization. However, binge drinking, lower social support for medical care, 3 or fewer annual clinic visits, and talking with 12 or more people weekly were significant predictors of preventability of hospitalization. Our CTA model illustrates how these risk factors interact in predicting preventability of hospitalization. Overall, 77% of preventable admissions were attributed to medication nonadherence (30%), alcohol or drug use (25%), or inadequate outpatient care in the previous 2 weeks (22%). Our results suggest that the size and nature of social support resources, binge alcohol drinking, and outpatient care may be important predictors of preventable hospitalization.
Acknowledgments
Grant Support: This project was supported by a Pfizer Health Literacy Grant. Dr. Arozullah is supported as a Research Associate in the Advanced Career Development Award Program of the Veterans Affairs Health Services Research and Development Service. Dr. Lee's participation in the study was partially supported by a research grant from the Agency for Healthcare Research and Quality (R01 HS13004). The study was investigator-initiated and the funding organizations (Pfizer, Incorporated, The Department of Veterans Affairs, and The Agency for Healthcare Research and Quality) had no role in the design, methods, and analysis of the study, or authorship of the article.
REFERENCES
- 1.Nielsen-Bohlman L, Panzer A, Kindig D. Washington, DC: Institute of Medicine of the National Academies; 2003. Health Literacy: A Prescription to End Confusion. [PubMed] [Google Scholar]
- 2.Davis TC, Arnold C, Berkel H, Nandy I, Jackson R, Glass J. Knowledge and attitude on screening mammography among low-literate, low-income women. Cancer. 1996;78:1912–20. doi: 10.1002/(sici)1097-0142(19961101)78:9<1912::aid-cncr11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 3.Davis TC, Dolan N, Ferreira MR, et al. The role of inadequate health literacy skills in colorectal cancer screening. Cancer Invest. 2001;19:193–201. doi: 10.1081/cnv-100000154. [DOI] [PubMed] [Google Scholar]
- 4.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–15. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 5.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. Arch Int Med. 1998;158:166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 6.Baker DW, Parker RM, Williams MV. Patient reading ability and use of health care services. J Gen Intern Med. 1997;12:50. [Google Scholar]
- 7.Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87:1027–30. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–51. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 9.Baker DW, Gazmararian JA, Williams MV, et al. Functional health literacy and the risk of hospital admission among medicare managed care enrollees. Am J Public Health. 2002;92:1278–83. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker DW, Parker RM, Williams MV, Clark DS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13:791–8. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kefalides P. Illiteracy: the silent barrier to health care. Ann Intern Med. 1999;130:333–6. doi: 10.7326/0003-4819-130-4-199902161-00001. [DOI] [PubMed] [Google Scholar]
- 12.Lee S, Arozullah A, Cho Y. Health literacy, social support, and health: a research agenda. Soc Sci Med. 2004;58:1309–21. doi: 10.1016/S0277-9536(03)00329-0. [DOI] [PubMed] [Google Scholar]
- 13.Brez SM, Taylor M. Assessing literacy for patient teaching: perspectives of adults with low literacy skills. J Adv. Nursing. 1997;25:1040–7. doi: 10.1046/j.1365-2648.1997.19970251040.x. [DOI] [PubMed] [Google Scholar]
- 14.Davis TC, Long S, Jackson R, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 15.Davis TC, Crouch MA, Long SW, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433–5. [PubMed] [Google Scholar]
- 16.Lin N, Ye X, Ensel WM. Social support and depressed mood: a structural analysis. J Health Soc Behav. 1999;40:344–59. [PubMed] [Google Scholar]
- 17.Sherbourne C, Steward A. The medical outcomes study social support survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 18.Ware JJ, Kosinski M, Keller S. A 12-item short form health survey. Medical Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Walker S, Sechrist K, Pender N. The health-promoting lifestyle profile: development and psychometric characteristics. Nursing Res. 1987;36:76–81. [PubMed] [Google Scholar]
- 20.Oddone E, Weinberger M, Horner M, et al. Classifying general medicine readmissions are they preventable? J Gen Intern Med. 1996;11:597–607. doi: 10.1007/BF02599027. [DOI] [PubMed] [Google Scholar]
- 21.Soltysik R, Yarnold P. Univariable optimal discriminant analysis: one-tailed hypotheses. Educ Psychol Meas. 1994;54:646–53. [Google Scholar]
- 22.Yarnold P, Soltysik R. Theoretical distributions of optima for univariate discrimination of random data. Decision Sci. 1991;22:739–52. [Google Scholar]
- 23.Yarnold P, Soltysik R, Bennett CL. Predicting in-hospital mortality of patients with AIDS-related Pneumocystis carinii pneumonia: an example of hierarchically optimal classification tree analysis. Stat. Med. 1997;16:1451–63. doi: 10.1002/(sici)1097-0258(19970715)16:13<1451::aid-sim571>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 24.Yarnold P, Soltysik R. Washington, DC: APA Books; 2005. Optimal Data Analysis: Guidebook with Software for Windows. [Google Scholar]
- 25.Arozullah A, Yarnold P, Weinstein R, et al. A new preadmission staging system for predicting in-patient mortality from HIV-associated Pneumocystis carinii pneumonia in the early-HAART era. Am J Respir Crit Care Med. 2000;161:1081–6. doi: 10.1164/ajrccm.161.4.9906072. [DOI] [PubMed] [Google Scholar]
- 26.Arozullah A, Parada J, Bennett C, et al. A rapid staging system for predicting mortality from HIV-associated community-acquired pneumonia. Chest. 2003;123:1151–60. doi: 10.1378/chest.123.4.1151. [DOI] [PubMed] [Google Scholar]
- 27.Penning M. Health, social support, and the utilization of health services among older adults. J Gerontol Series B, Psychol Sci Soc Sci. 1995;50:S330–9. doi: 10.1093/geronb/50b.5.s330. [DOI] [PubMed] [Google Scholar]
- 28.Chin MH, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. Am J Cardiol. 1997;79:1640–4. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- 29.Grant R, Charlebois E, Wachter RM. Risk factors for early hospital readmission in patients with AIDS and pneumonia. J Gen Intern Med. 1999;14:531–6. doi: 10.1046/j.1525-1497.1999.08157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mor-Barak M, Miller L, Syme L. Social networks, life events, and health of poor, frail elderly: a longitudinal study of the buffering versus direct effect. Fam Community Health. 1991;12:1–13. [Google Scholar]
- 31.Mistry R, Rosansky J, McGuire J, McDermott C, Jarvik L. Social isolation predicts re-hospitalization in a group of older American veterans enrolled in the UPBEAT program. Int J Geriatric Psychiatry. 2001;16:950–9. doi: 10.1002/gps.447. [DOI] [PubMed] [Google Scholar]
- 32.Andersen R. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 33.Naimi T, Brewer R, Mokdad A, Denny C, Sedula M, Marks J. Binge drinking among US adults. JAMA. 2003;289:70–5. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- 34.Fleming M, Barry K, Manwell L, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–45. [PubMed] [Google Scholar]
- 35.Maisto S, Saitz R. Alcohol use disorders: screening and diagnosis. Am J Addict. 2003;12:S12–25. doi: 10.1111/j.1521-0391.2003.tb00493.x. [DOI] [PubMed] [Google Scholar]
- 36.Healthy People. Washington, DC: U.S. Department of Health and Human Services; 2000. 2010: With Understanding and Improving Health and Objectives for Improving Health. [Google Scholar]
- 37.McCaul M, Petry N. The role of psychosocial treatments in pharmacotherapy for alcoholism. Am J Addict. 2003;12:S41–52. doi: 10.1111/j.1521-0391.2003.tb00495.x. [DOI] [PubMed] [Google Scholar]
- 38.Baker D, Gazmararian J, Williams M, et al. Health literacy and use of outpatient physician services by Medicare managed care enrollees. J Gen Intern Med. 2004;19:215–20. doi: 10.1111/j.1525-1497.2004.21130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Payne S. Identifying and managing inappropriate hospital utilization: a policy synthesis. Health Services Res. 1987;22:712–69. [PMC free article] [PubMed] [Google Scholar]