Abstract
OBJECTIVE
The study's objectives were to determine (1) the rate at which department of medicine faculty in the United States are promoted, (2) if clinician-educators (CEs) are promoted to Associate Professor at the same rate as clinician-investigators (CIs), and (3) the variables that predict promotion.
METHODS
The Prospective Study of Promotion in Academia was a part-retrospective, part-prospective (from 2000 to 2003) cohort study. Six-hundred and four Internal Medicine junior faculty across the United States who had been registered as new appointees with the Association of American Medical Colleges in 1995 were invited to participate. Twenty-one percent of these had already left their institution when the study began. One hundred and eighty-three Internal Medicine faculty from 87 institutions in 35 states enrolled. The main outcome measure was the time from appointment as Assistant Professor to promotion to Associate Professor.
RESULTS
Follow-up was complete for all 183 faculty. Among the faculty that achieved promotion, the estimated median time to promotion was 6.0 years (95% Conf. Int.=5.8 to 6.2). The unadjusted sixth-year promotion rate for CEs was 16%, while for CIs it was 26% (P=.002). Independent negative predictors of promotion included low amount of research time (Hazard Ratio [HR] =0.3, 95% Conf. Int.=0.2 to 0.5), having a manuscript review service (HR=0.4, 95% Conf. Int.=0.2 to 0.7), never meeting with Chairman/Chief about promotion (HR=0.4, 95% Conf. Int.=0.2 to 0.7), low job satisfaction (HR=0.5, 95% Conf. Int.=0.3 to 0.9), and working in the Northeast (HR=0.6, 95% Conf. Int.=0.4 to 1.1). Positive predictors included making between $130 and $149,000 per year (HR=1.9, 95% Conf. Int.=1.1 to 3.4), working more than 60 h/wk (HR=1.9, 95% Conf. Int.=1.1 to 3.0), having a career mentor available (HR=1.8, 95% Conf. Int.=1.1 to 2.9), and having access to a grant office (HR=1.6, 95% Conf. Int.=1.0 to 2.6).
CONCLUSION
CEs and CIs appear to be promoted at different rates. The characteristics that are independently associated with earlier promotion may be helpful for institutions and individual faculty that are committed to achieving promotion efficiently.
Keywords: promotion, motivation, academic medicine
In a 1997 survey by Jones and Gold from the Association of American Medical Colleges (AAMC), nearly three quarters of medical school deans reported that their schools had a separate track for faculty who predominantly worked in patient care and education, commonly known as clinician-educators (CEs).1 These tracks developed as clinical revenue played an increasingly important role in funding academic medical centers, growing from approximately 3% in the 1960s to nearly 45% of their revenue today.2 Not only do CEs fulfill the ever increasing clinical demands at academic medical centers, often they are the education specialists and program directors.
CEs are concerned that their contributions to the academic centers have not been recognized by their departments and promotion committees.3 Academic promotions are based predominantly upon academic productivity as measured by the number and quality of peer-reviewed publications in a faculty member's portfolio.4 When we surveyed the promotion chairs in the United States and Canada in 1996, they claimed that promotion committees valued teaching skills and clinical skills as the most important contributions of CEs job performance. By and large, the committees expected about half the number of peer-reviewed publication from CEs (mean 5.7 papers) as compared with clinician-investigators (CIs) (10.6) for promotion to Associate Professor.5 Our second study of department of medicine chairs in 1997 demonstrated that they had different expectations and views toward the promotion of CEs as compared with the promotion committee chairs.6
As Levinson and Rubenstein have stated, “Just as researchers excel at the discovery of new knowledge but have little time for teaching and clinical care, clinician-educators excel at teaching and clinical care but have little time to conduct research. Accordingly, one would expect institutions to recognize clinician-educators for achieving the highest standards related to their principal responsibilities and consistent with their institution's mission. But is that the case?”7 This study attempts to answer that question.
The Prospective Study of Promotion in Academia (PSPA) is a part-retrospective, part-prospective cohort study, designed to determine (1) the rate at which department of medicine clinical faculty in the United States are promoted, (2) if CEs are promoted to Associate Professor at the same rate as CIs, and (3) the variables (demographics, job characteristics, prior training, and motivation) associated with promotion of CEs.
METHODOLOGY
The methodology used to solicit participants, develop the entry and follow-up questionnaires, recode variables, and validate our measurement instruments has been comprehensively described in our previous papers.8, 9 Relevant highlights are reiterated below.
In November 1999, we used the AAMC Faculty Roster System Database to identify a population of academic faculty that joined departments of medicine at the Assistant Professor level from June to December 1995. As we intended to follow participants until 2003, this design allowed us to collect data about participant characteristics prospectively, thereby decreasing recall bias. Also, because Assistant Professor medical school faculty are frequently reviewed for promotion after approximately 6 years at that rank, we identified the study population 3 years before the primary end point, promotion to Associate Professor, would be attained, thereby avoiding unnecessary prolongation of the study period.
Study Participants
In November 1999, the AAMC database contained 90,101 active, full-time faculty members. Of those faculty members, 604 had medical doctorate degrees, held primary appointments in Departments of Medicine, and had been appointed Assistant Professor between June and December 1995. We mailed an invitation and a baseline questionnaire to these faculty in February 2000 when they were on average 4.7 years into their appointments as Assistant Professors. For those who did not respond, 2 other invitation letters as well as a postcard reminder followed the initial mailing at monthly intervals. One hundred and twenty-nine of the questionnaires (21%) were returned to us without forwarding addresses, labeled “Return to Sender,” Inquiry into one quarter of these demonstrated that these faculty had already changed jobs. Two hundred and ninety-two faculty (48%) did not respond to repeated invitations, thereby choosing not to participate. One hundred and eighty-three faculty agreed to enroll in the study (participation rate=enrollees/(invitees−return to senders=38%).
Questionnaire Development and Data Collection
A review of the literature revealed several variables that have been associated with promotion in previous studies: gender,10 race,11 fellowship training,12 specialization,13 membership in Alpha Omega Alpha during medical school,14 class rank at graduation,14 and research experience during medical school.14 These variables were included in the baseline questionnaire along with other demographics, job characteristics, promotion-related attitudes and beliefs, a global job satisfaction measure,15 and the availability and utilization of 12 facilitators of success in academia (e.g., secretarial support, mentors, faculty development programs, and protected scholarly work time).
At an interim follow-up survey 1 year after enrollment, we used a 13-item modified “Rosenberg Occupational Value” scale to assess what motivated participants in their work. Factor analysis demonstrated 3 factors as being motivating: self-expression, helping others, and extrinsic rewards. Respondents also indicated the number of peer-reviewed, first-author publications in their portfolio at that time.9
We assured the respondents that their information would be kept confidential and that data would be reported in aggregate. The St. Luke's Hospital Institutional Review Board (Kansas City, Mo) approved the study.
Additional Characteristics
We used the U.S. Census Bureau's assignment of states to particular regions: Northeast, South, Midwest, and West.16 The rankings for the amount of National Institute of Health (NIH) funding awarded to Departments of Medicine in 2002 were obtained from the NIH website.17 Assessments from the U.S. News and World Report website were obtained for the medical school rankings.18 The size of faculty at U.S. medical schools was obtained from the AAMC Faculty Roster from December 31, 2002.19
FOLLOW-UP
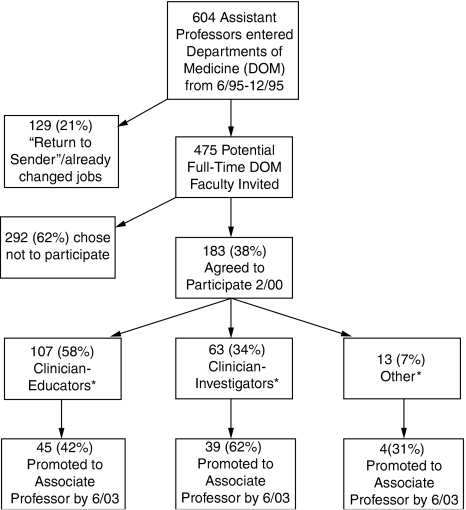
From February to June 2003, we contacted all 183 (follow-up was complete) of the study participants either by postcard, e-mail, or phone in order to determine (1) whether they had been promoted to Associate Professor, and (2) the month and year of their promotion. Eighty-eight participants (48%) had been promoted (Fig. 1).
FIGURE 1.
Flow diagram of faculty recruitment into Prospective Study of Promotion in Academia study and follow-up.
Data Analysis
For the continuous variables, we examined frequency distributions and descriptive statistics for evidence of skewness, outliers, and nonnormality. Continuous variables were recoded generally into tertiles in order to facilitate the presentation of the bivariate and multivariable analyses. Several categorical variables were recoded based on sparseness in certain categories.
Three different criteria were used to classify appropriately participants as either CEs or CIs. First, we gave the participants operational definitions for CE and CI (adapted from the literature20) and asked them to indicate into which category they fell (criteria 1). Components of these definitions were that CIs spend “more than 50% time in research,” and CEs spend “more than 50% time in teaching-related activities.” By this procedure, 72 physicians described themselves as CEs and 56 faculty members considered themselves CIs. Fifty-two participants categorizing themselves as “clinician” or “other” were assigned at the time of enrollment to CE or CI by the authors independently based upon cut points in the amount of research time (30% cut point—criteria 2) and clinical work in the presence of a learner (15% cut point—criteria 3) in which they were involved, as suggested by Zakowski.21 In 9 of the 52 cases, the authors disagreed on the assignments and discussions about the discrepancies and the rationales were undertaken in order to arrive at a consensus about the categorizations of these physicians at the time of enrollment in 2000. Thirteen participants did not choose a category, did not provide work time information, and thus could not be categorized by the investigators. These 13 participants were labeled as “Other” and were included in all analyses.
We used the Cox proportional hazards procedure to generate crude hazard ratios (HRs) between the characteristics and the time to promotion. Six-year promotion rates were determined by the Kaplan-Meier method. We looked at the promotion rate at the sixth year given that it was a reasonable length of time to expect promotion, and because, looking at the distributions, it allowed for the most robust analyses. Nine (5%) of the 183 participants reported they had “left academic medicine.” These 9 participants were treated as “not promoted” in the survival analyses, but were left uncensored to the end of the study period. The reason for this decision is because (1) the exact date they left academia was unknown for several subjects, (2) many people leave academia when it becomes apparent that they will not succeed (achieve promotion), and (3) leaving these few subjects uncensored had negligible effects on the results.
We used multivariable Cox proportional hazard modeling to find characteristics that were independently associated with the time to promotion. Starting from the most significant variables in the univariate analyses, we used the likelihood ratio test to determine whether inclusion of a new variable improved the fit of the multivariable model. Probability for entry into the model was .05 and for exclusion was .1 or greater. We also examined variables of interest not significant in the univariate analysis. Finally, using the variables derived from this Cox proportional hazard model, we adjusted all the crude HRs.
The sample size of 183 participants provided 80% power to detect a 20% absolute difference in promotion between 2 equal groups, with a 5% false-positive rate (2-sided tests). We used SPSS version 12.0 and S-plus version 6.2 for all data analyses. Because of the multiple comparisons and models considered, we were cautious with our findings. Any P values between .1 and .01 we describe as a trend, and reserve the wording “significant” only for those P values less than .01.
RESULTS
One hundred and eighty-three faculty from 35 different states and 87 different academic centers in the United States agreed to participate in the study. The AAMC provided aggregate data on the enrollees as well as for those who chose not to participate. There was no significant difference between enrollees and nonparticipants in age (mean=40, SD=3.9), years since graduation, and the proportion in a tenure track (all P>.05). A higher proportion of enrollees than nonparticipants were female (35% vs 26%, P=.03). More enrollees than nonparticipants were white (80% vs 63%, P=.002).
Having entered the study on average 4.7 (SD=1.1) years after the participants' appointments to Assistant Professor, 13 (7%) reported already having been promoted to Associate Professor at the time of enrollment (7 CEs and 7 CIs). At the time of the interim data collection in 2001, 35 (19%) of the participants had been promoted.
Figure 1 demonstrates that by the end of June 2003 (8 years after their appointment to the rank of Assistant Professor in 1995), 39 (62%) CIs had achieved promotion to Associate Professor, compared with 45 (42%) of the CEs and 4 (31%) of those in the “other” category (P<.01). Among the individuals that had achieved promotion, the estimated median time to promotion was 6.0 years (95% Conf. Int.=5.8 to 6.2).
Table 1 reports the major independent variables and their associations with promotion. These results are given in terms of their 6-year promotion rates and HRs. The raw scores have also been adjusted for the 9 independent predictors of promotion that emerged from the multivariable Cox proportional hazard modeling in Table 2.
Table 1.
Participant Characteristics and Their Associations with Promotion in the Prospective Study of Promotion in Academia Study, N=183
| Characteristics | Frequency n(%) | Sixth Year Promotion Rate (95% Conf.Int.) | HR (95% Conf. Int.) | |
|---|---|---|---|---|
| Row | Adjusted† | |||
| Demographics and background | ||||
| Female‡ | 64 (35) | 16% (6 to 25) | 1.1 (0.7 to 1.7) | 1.3 (0.8 to 2.1) |
| Caucasian‡ | 146 (80) | 22% (15 to 28) | 1.3 (0.7 to 2.3) | 1.0 (0.6 to 1.8) |
| Fellowship trained‡ | 136 (75) | 24% (16 to 31) | 1.7§ (1.0 to 2.9) | 1.5 (0.8 to 2.7) |
| Married‡ | 162 (89) | 21% (14 to 27) | 1.3 (0.6 to 2.7) | 1.5 (0.7 to 3.4) |
| Characteristics of position | ||||
| Career path** | ||||
| CI | 63 (35) | 26% (14 to 37) | 1.9∥ (1.3 to 3.0) | 1.3 (0.7 to 2.4) |
| Other | 13 (6) | 18% (0 to 38) | 0.6 (0.2 to 2.0) | 2.1 (0.6 to 7.6) |
| CE | 107 (59) | 16% (9 to 23) | 1.0* | 1.0* |
| Time performing research | ||||
| More than 30% | 53 (29) | 31% (17 to 42) | 3.0¶ (1.7 to 5.0) | 4.8¶ (2.6 to 8.9) |
| 6% to 30% | 57 (32) | 24% (12 to 34) | 2.2∥ (1.3 to 3.8) | 2.9¶ (1.6 to 5.4) |
| 5% or less | 71 (39) | 9% (2 to 15) | 1.0* | 1.0* |
| Time precepting learners in clinic | ||||
| 5% or less | 81 (45) | 19% (10 to 27) | 1.1 (0.7 to 1.8) | 1.8§ (1.0 to 3.2) |
| 6% to 15% | 47 (26) | 22% (9 to 33) | 1.1 (0.6 to 2.0) | 1.7 (0.9 to 3.1) |
| More than 15% | 53 (29) | 20% (8 to 30) | 1.0* | 1.0* |
| Time attending learners in hospital | ||||
| 5% or less | 62 (34) | 16% (6 to 25) | 0.9 (0.5 to 1.6) | 1.0 (0.5 to 1.8) |
| 6% to 20% | 64 (35) | 27% (15 to 38) | 1.4 (0.8 to 2.3) | 1.5 (0.9 to 2.6) |
| More than 20% | 55 (30) | 15% (5 to 25) | 1.0* | 1.0* |
| Time providing patient care without learners | ||||
| 10% or less | 70 (39) | 28% (16 to 38) | 2.0∥ (1.2 to 3.4) | 1.0 (0.5 to 1.8) |
| 11% to 30% | 50 (28) | 19% (7 to 30) | 1.3 (0.7 to 2.4) | 0.8 (0.4 to 1.5) |
| More than 30% | 61 (34) | 12% (3 to 19) | 1.0* | 1.0* |
| Time in administrative duties | ||||
| 5% or less | 83 (46) | 16% (8 to 24) | 1.1 (0.6 to 1.9) | 1.5 (0.8 to 2.7) |
| 6% to 15% | 55 (30) | 30% (17 to 41) | 1.6 (0.9 to 2.8) | 1.3 (0.7 to 2.5) |
| More than 15% | 43 (24) | 14% (3 to 24) | 1.0* | 1.0* |
| Hours per week | ||||
| More than 60 | 41 (23) | 26% (12 to 38) | 2.2∥ (1.2 to 3.8) | 1.8 (1.0 to 3.2) |
| 51 to 60 | 80 (45) | 21% (12 to 30) | 1.2 (0.7 to 2.0) | 0.9 (0.5 to 1.7) |
| 50 or less | 57 (32) | 15% (5 to 24) | 1.0* | 1.0* |
| “Clinical” track‡ | 64 (36) | 19% (9 to 28) | 0.7 (0.5 to 1.1) | 1.0 (0.6 to 1.7) |
| Eligible for tenure‡ | 75 (44) | 24% (14 to 34) | 1.4 (0.9 to 2.1) | 1.3 (0.8 to 2.1) |
| Salary | ||||
| <90K | 18 (10) | 11% (0 to 25) | 1.6 (0.6 to 4.2) | 2.3 (0.8 to 6.1) |
| 90K to 109K | 46 (26) | 15% (4 to 25) | 1.6 (0.8 to 3.5) | 1.6 (0.7 to 3.5) |
| 110K to 129K | 51 (28) | 27% (14 to 39) | 2.1 (1.0 to 4.3) | 1.9 (0.9 to 4.0) |
| 130K to 149K | 35 (19) | 31% (14 to 45) | 2.4§ (1.1 to 5.0) | 3.3∥ (1.4 to 7.4) |
| 150K or more | 30 (17) | 10% (0 to 21) | 1.0* | 1.0* |
| Career development and support | ||||
| How often meet with chief/chair to review perform and discuss expectations for promotion | ||||
| More than yearly | 69 (38) | 26% (15 to 36) | 2.9∥ (1.5 to 5.6) | 2.7∥ (1.4 to 5.5) |
| 1 to 2 y | 70 (39) | 22% (12 to 31) | 1.7 (0.9 to 3.2) | 2.4§ (1.2 to 4.9) |
| Never | 41 (23) | 10% (0 to 18) | 1.0* | 1.0* |
| Aware of expectation regarding promotion‡ | 119 (67) | 23% (15 to 31) | 1.6§ (1.0 to 2.6) | 1.0 (0.6 to 1.8) |
| Grant seminars available‡ | 109 (61) | 26% (17 to 33) | 1.5 (1.0 to 2.4) | 1.6 (1.0 to 2.6) |
| Seen written promotion guidelines‡ | 102 (57) | 27% (18 to 35) | 2.2∥ (1.4 to 3.4) | 1.1 (0.7 to 1.9) |
| >10% protected scholarly time‡ | 87 (49) | 28% (17 to 37) | 2.0 (1.3 to 3.0) | 1.2 (0.7 to 2.0) |
| Career mentors available‡ | 83 (46) | 27% (16 to 36) | 2.1¶ (1.4 to 3.2) | 1.8§ (1.1 to 2.9) |
| Faculty development program available‡ | 81 (45) | 26% (16 to 35) | 1.5 (1.0 to 2.2) | 1.1 (0.7 to 1.7) |
| Grant office available‡ | 74 (42) | 20% (10 to 29) | 1.5 (1.0 to 2.4) | 1.6 (1.0 to 2.6) |
| Manuscript review service available‡ | 42 (22) | 10% (0 to 19) | 0.6 (0.3 to 1.0) | 0.4∥ (0.2 to 0.7) |
| Job motivation and satisfaction | ||||
| Motivation: Self-expression | ||||
| High | 43 (30) | 29% (13 to 41) | 2.2∥ (1.2 to 3.9) | 2.1§ (1.1 to 4.0) |
| Medium | 53 (37) | 20% (8 to 30) | 1.2 (0.7 to 2.2) | 1.0 (0.5 to 2.0) |
| Low | 48 (33) | 15% (4 to 25) | 1.0* | 1.0* |
| Motivation: Helping others | ||||
| High | 39 (27) | 13% (2 to 24) | 0.8 (0.5 to 1.5) | 1.1 (0.6 to 2.1) |
| Medium | 54 (38) | 21% (9 to 31) | 0.9 (0.6 to 1.6) | 1.0 (0.5 to 1.8) |
| Low | 51 (35) | 27% (13 to 38) | 1.0* | 1.0* |
| Motivation: Extrinsic rewards | ||||
| High | 44 (31) | 19% (6 to 30) | 0.9 (0.5 to 1.6) | 0.9 (0.5 to 1.7) |
| Medium | 53 (37) | 31% (17 to 43) | 1.2 (0.7 to 2.1) | 1.0 (0.6 to 1.9) |
| Low | 47 (32) | 11% (1 to 20) | 1.0* | 1.0* |
| Global job satisfaction | ||||
| High | 66 (37) | 22% (11 to 31) | 2.1∥ (1.2 to 3.6) | 2.0§ (1.1 to 3.7) |
| Medium | 60 (34) | 26% (14 to 37) | 1.7 (1.0 to 3.1) | 2.0§ (1.1 to 3.7) |
| Low | 53 (30) | 11% (2 to 20) | 1.0* | 1.0* |
| Medical center characteristics | ||||
| University based‡ | 150 (83) | 23% (15 to 29) | 2.3§ (1.1 to 4.8) | 2.0 (0.9 to 4.1) |
| Region of country | ||||
| Midwest | 59 (32) | 21% (10 to 31) | 2.3∥ (1.3 to 4.1) | 2.2§ (1.2 to 4.0) |
| South | 38 (21) | 22% (7 to 34) | 2.4∥ (1.3 to 4.5) | 1.4 (0.7 to 2.8) |
| West | 27 (15) | 24% (5 to 39) | 1.6 (0.8 to 3.4) | 1.1 (0.5 to 2.4) |
| Northeast | 59 (32) | 17% (7 to 26) | 1.0* | 1.0* |
| Top 25 DOMs NIH Research Funding‡ | 40 (22) | 21% (7 to 33) | 1.5 (0.9 to 2.3) | 0.8 (0.5 to 1.3) |
| First author publications | ||||
| 11 and up | 26 (18) | 38% (17 to 55) | 6.0¶ (2.2 to 16.2) | 7.4∥ (2.2 to 24.8) |
| 6 to 10 | 34 (23) | 26% (10 to 40) | 3.1§ (1.1 to 8.2) | 4.9∥ (1.6 to 15.6) |
| 1 to 5 | 66 (46) | 16% (6 to 25) | 2.6§ (1.0 to 6.7) | 3.4§ (1.1 to 9.9) |
| Zero | 19 (13) | 0% | 1.0* | 1.0* |
1.0 indicates the reference category for this variable.
Values have been adjusted for the 9 independent predictors of promotion that emerged from the multivariable Cox proportional hazard modeling: working in research less than 5% FTE, having a manuscript review service available, never meeting with the Chair or Chief to discuss promotion, having a low global job satisfaction, making a salary of $130,000 to $149,000 per year, working 60 or more hours per week, having a career mentor, being from the Northeast region, having a grant office available.
In the interest of space, for these binary variables we have shown only one value (i.e., female vs male). The value not shown (i.e., male) would be the reference value for the HRs.
P<.05;
P<.01;
P<.001.
Assignment to the category of CE, CI, and other was made at the time of enrollment into the study, on average 4.7 years into their appointment as Assistant Professor.
CIs, clinician-investigators; CEs, clinician-educators; HR, hazard ratio; FTE, full-time equivalent.
Table 2.
Variables that are Independently Associated with Promotion According to Multivariable Cox Proportional Hazard Modeling, Listed by Strength of Their Coefficient
| Coefficient | Hazard Ratio | P value | |
|---|---|---|---|
| Percent research <5% FTE | −1.29 | 0.3 (0.2 to 0.5) | <.001 |
| Having a manuscript review service available | −0.96 | 0.4 (0.2 to 0.7) | .004 |
| Never meeting with the chair or chief about promotion | −0.94 | 0.4 (0.2 to 0.7) | .005 |
| Being in the lower third tier for job satisfaction | −0.70 | 0.5 (0.3 to 0.9) | .012 |
| Being in the $130,000 to $149,000/y salary bracket | 0.66 | 1.9 (1.1 to 3.4) | .016 |
| Working more than 60 h/wk | 0.62 | 1.9 (1.1 to 3.0) | .012 |
| Having career mentor | 0.59 | 1.8 (1.1 to 2.9) | .012 |
| Being from the Northeast region | −0.49 | 0.6 (0.4 to 1.1) | .086 |
| Having a grant office available | 0.47 | 1.6 (1.0 to 2.6) | .070 |
Likelihood ratio test=72.2 on 9 df, P=5.63e−012; n=169 (14 observations deleted because of missing values).
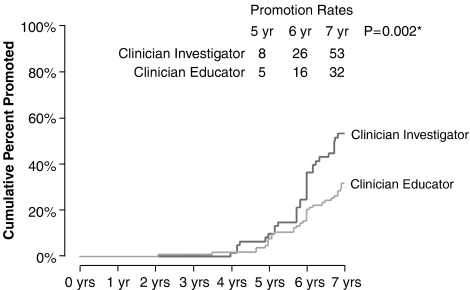
Gender, race, and marital status had no effect on promotion rates, (Table 1). Having completed a fellowship trended toward improved promotability before adjustment (P=.049). CIs appear to be promoted faster than CEs (see Fig. 2). The unadjusted HR for CIs is nearly twice that of CEs (HR=1.9, P=.003). Working more than 30% of the workday in research was strongly associated with promotion (HR=4.8,<0.0001). After adjustment, working less than 5% time as a preceptor for medical trainees in clinic trended toward increased promotion (adjusted HR [AHR]=1.8, P=.046) as did working more than 60 h/wk (AHR=1.8, P=.054). Assistant Professor faculty paid at the highest levels (>$150K) were the least successful in attaining promotion after adjustment, and it was noted that faculty salaried within the $130,000 to $149,000-per-year category were promoted at the highest rate (AHR=3.3, P=.0049).
FIGURE 2.
Kaplan-Meier graph demonstrating the promotion rate of clinician-investigators and clinician-educators.
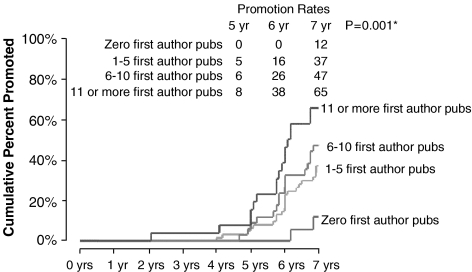
The number of first-author, peer-reviewed publications that a participant reported on the interim analysis was the strongest independent predictor of promotion, with faster promotion associated with increasing gradations of publications (see Fig. 3). The strength of this variable supports the premise that this is an intermediate outcome variable, or a surrogate marker of promotion. Because of the latter, this variable was not included in the final model (seen in Table 2), as this study looked for characteristics that would contribute to participants' productivity and eventual promotion, rather than markers of productivity themselves.
FIGURE 3.
Kaplan-Meier curves demonstrating the ability of the number of publications to predict promotion.
Each of the 87 institutions was represented in the dataset by 2.1 assistant professors (SD=1.6) on average. We analyzed the data and found a single large institution that had 10 faculty represented in the study whose promotion rates may have been different from the others. Because of the potential for a clustering effect we re-ran the data analysis with and without the faculty from this institution and found that our results were unchanged.
Other variables not shown that had no association with promotion included being in the top quartile of class rank, being Alpha Omega Alpha (AOA), having participated in research in medical school, having children, being in the top 25 ranking of U.S. News and World Report's best medical schools, having secretarial support, the size of the medical school faculty, and having statistical support.
DISCUSSION
Assistant Professors wanting to be promoted to the rank of Associate Professor could learn a lot by carefully reviewing this study's findings. While moving to the Midwest and negotiating a salary into a specific range may not be controllable, factors such as identifying career mentors, meeting with supervisors about promotion at least yearly, devoting 30% of their work to research efforts, working more than 60 h/wk, feeling satisfied at work, and being motivated by self-expression may be noteworthy considerations for those interested in achieving promotion in academic medicine.
Our sample of Assistant Professors represents only faculty members who have stayed at the institutions that initially hired them at that rank. Twenty-one percent of faculty members whom we attempted to recruit into this study had already left their institutions. The estimated rates of promotion are only representative of those who survived the first 4.7 years (on average) as Assistant Professor. This has created a potential source of selection bias, and may be artificially inflating the rate of promotion. Conversely, moving to another institution sometimes provides leverage toward earlier promotion, as one of our authors has experienced. Either way, all of the modeling results should be interpreted with this caveat in mind.
In spite of the many intriguing associations uncovered by this study, promotion in academic medicine continues to be closely connected with one's scholarly productivity. The linear association between the number of publications and promotion made it imperative to treat publications as an intervening variable. The percent job-effort directed toward research and the completion of a fellowship were the only independent predictors of the number of papers authored (P<.01). Although the number of publications is a critical factor in determining the likelihood of successful promotion, 20% of the faculty studied that were ultimately promoted had few first-authored, peer-reviewed publications at the time of interim follow-up. While we have not seen the submitted promotion portfolios for these individuals, it is likely that they were able to convincingly demonstrate excellence and accomplishment in areas other than publications, such as administration or program building.
This study should remind Departments of Medicine and their leadership about the need to keep faculty members satisfied in work that matches their inherent motivations. Happy workers are more productive.22, 23 Further, it seems intuitive that faculty members that are satisfied, excited, and motivated in their work are more likely to put in the long hours (an independent predictor of promotion) and less likely to burn out. This reasoning presumes that satisfaction is associated with the attainment of promotion, but the reverse order may be explanatory such that those individuals who are convinced that they are on track for promotion may be inherently more satisfied and fulfilled in their work.
After adjustment for factors independently associated with promotion, the HR for CIs dropped from 1.9 to 1.3, and was no longer statistically significant. However, by definition, CIs spend a substantial portion of their work effort on research, one of the most robust independent variables from the multivariable model that was used for adjustment.
Beyond the novel results, this study adds to the literature because of its unique design and methodology as a way to understand the issues related to the promotion of medical faculty members. As opposed to contacting individuals at one point in time to gain their insights and impressions as in prior studies, communications with our informants as they were navigating towards and through the promotion process allowed for data collection that was richer and subject to fewer biases. Some of this study's negative findings are most reassuring; the lack of effect of race, gender, and marital status (among others) on promotion rates may suggest that the promotion process is relatively fair and equitable across some lines.
Several other limitations of this study should be considered. First, we relied exclusively on self-report to characterize the physicians and many of the institutional variables. In balance, we attempted to use previously validated measures (e.g., job motivation and global satisfaction) and external data (e.g., NIH rank list) when available. Second, the characterization of faculty as either CEs or CIs is difficult. Our a priori awareness of this complexity was in fact the rationale for the comprehensive 3-step process to classify the faculty at enrollment. Nonetheless, the results demonstrate that a faculty member's percent effort spent on research is the strongest independent predictor of promotion. Third, the study was limited to faculty within the departments of medicine and may not be generalizable to other departments. Finally, given the resources to recruit a larger cohort, some of the variables that were close to significance after adjustment may have remained so with greater power. Also, we examined a large number of independent variables simultaneously in the regression models. Although there are no formal guidelines for the number of variables that can be considered in a single analysis, there should be 10 to 15 observations per independent variable as a rule of thumb to ensure that the results are replicable.24 This would require a sample nearly 5 times the size of our current study.
CONCLUSION
The achievement of promotion is a common goal for academic faculty members. While the difficulty in reaching this goal may vary depending on the particular institution, success should be realistically attainable for all. Those whose primary responsibilities are in the area of patient care and education (CEs) cannot be held to the same standards with respect to publications and the dissemination of new information as faculty whose efforts are dedicated primarily toward research. In order to level the playing field and to retain all types of faculty members that are an asset to a school of medicine, academic institutions should (1) provide training, mentorship, and protected time for CEs to produce scholarly endeavors, (2) assign expectations for promotion in terms of the number of publications for each faculty member commensurate with that individual's amount of protected research time, and (3) genuinely value excellent accomplishments in the areas of patient care and teaching when making decisions related to the promotion of their faculty members. Advocating for an impartial and evenhanded approach to promotion in academia can only serve to strengthen our institutions.
Acknowledgments
Dr. Wright is an Arnold P. Gold Foundation Associate Professor of Medicine. The authors would also like to acknowledge Dr. Edward Dismuke, M.D., Dean of the University of Kansas School of Medicine—Wichita, for his assistance on this project.
The PSPA study was partially funded by a grant from the Society of General Internal Medicine and a grant from the St. Luke's Hospital Foundation, Kansas City, MO.
Dr. Bresley had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis, and also obtained funding for the study. He and Dr. Wright were responsible for the conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript, and critical revision of manuscript. Dr. Simon helped him with the statistical analysis.
REFERENCES
- 1.Jones RF, Gold JS. Faculty appointment and tenure policies in medical schools: a 1997 status report. Acad Med. 1998;73:212–9. doi: 10.1097/00001888-199802000-00023. [DOI] [PubMed] [Google Scholar]
- 2.Tierney WG. The end of medical tenure as we know it? Academe. 1999;85:39–42. [Google Scholar]
- 3.Thomas PA, Diener-West M, Canto MI, Martin DR, Post WS, Streiff MB. Results of an academic promotion and career path survey of faculty at the Johns Hopkins University School of Medicine. Acad Med. 2004;79:258–64. doi: 10.1097/00001888-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Stossel TA. Volume: papers and academic promotion. Ann Intern Med. 1991;106:146–8. doi: 10.7326/0003-4819-106-1-146. [DOI] [PubMed] [Google Scholar]
- 5.Beasley BW, Wright SM, Cofrancosco J, Jr, et al. Promotion criteria for clinician-educators in the United States and Canada: a survey of promotion committee chairpersons. JAMA. 1997;278:723–8. [PubMed] [Google Scholar]
- 6.Atasoylu AA, Wright SM, Beasley BW, et al. Promotion criteria for clinician-educators. J Gen Intern Med. 2003;18:711–6. doi: 10.1046/j.1525-1497.2003.10425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levinson W, Rubenstein A. Mission critical—integrating clinician-educators into academic medical centers. N Engl J Med. 1999;341:840–3. doi: 10.1056/NEJM199909093411111. [DOI] [PubMed] [Google Scholar]
- 8.Beasley BW, Wright SM. Looking forward to promotion: characteristics of participants in the prospective study of promotion in academia (PSPA) J Gen Intern Med. 2003;18:705–10. doi: 10.1046/j.1525-1497.2003.20639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright SM, Beasley BW. The motivating factors for academic physicians within the Departments of Medicine. Mayo Clin Proc. 2004;79:1145–50. doi: 10.4065/79.9.1145. [DOI] [PubMed] [Google Scholar]
- 10.Dial TH, Bickel J, Lewicki AM. Sex differences in rank attainment among radiology and internal medicine faculty. Acad Med. 1989;64:198–202. doi: 10.1097/00001888-198904000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Palepu A, Carr PL, Friedman RH, et al. Minority faculty and academic rank in Medicine. JAMA. 1998;280:767–71. doi: 10.1001/jama.280.9.767. [DOI] [PubMed] [Google Scholar]
- 12.Sheffield JVL, Wipf JE, Buchwald D. Work activities of clinician-educators. J Gen Intern Med. 1998;13:406–9. doi: 10.1046/j.1525-1497.1998.00120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnett RC, Carr P, Boisnier AD, et al. Relationship of gender and career motivation to medical faculty members' production of academic publications. Acad Med. 1998;73:180–6. doi: 10.1097/00001888-199802000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Brancati FL, Mead LA, Levine DM, et al. Early predictors of career achievement in academic medicine. JAMA. 1992;267:1372–6. [PubMed] [Google Scholar]
- 15.Locke EA. The nature and causes of job satisfaction. In: Dunnette MD, editor. Handbook of Industrial and Organizational Psychology. Chicago: Rand McNally; 1969. [Google Scholar]
- 16.Cartography Boundary Files. [April 25 2004]; http://www.census.gov/geo/www/cob/rg_metadata.html.
- 17.NIH Extramural Awards Ranking Tables. [April 25 2004]; http://grants.nih.gov/grants/award/trends/medpt02.xls.
- 18.America's Best Graduate Schools. [April 25 2004]; http://www.usnews.com/usnews/edu/grad/rankings/med/medindex_brief.php.
- 19.Reports Available Through Faculty Roster. [April 25 2004]; http://www.aamc.org/data/facultyroster/reports.htm.
- 20.Levinson W, Branch WT, Kroenke K. Clinician-educators in academic medical centers: a two-part challenge. Ann Intern Med. 1998;129:59–64. doi: 10.7326/0003-4819-129-1-199807010-00013. [DOI] [PubMed] [Google Scholar]
- 21.Zakowski LJ, Cooney TG, Noel GL. Do general internal medicine fellows find jobs that match their training? J Gen Intern Med. 1998;13:410–3. doi: 10.1046/j.1525-1497.1998.00121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Happy Employees Make Productive Employees. [May 21 2004]; http://www.salesvantage.com/news/management/happy_employees.shtml. [PubMed]
- 23.Happy Employees Make Productive Employees. [May 21 2004]; http://www.chartcourse.com/articlehappy.htm. [PubMed]
- 24.Harrell FE Jr, Lee KL, Califf RM, et al. Regression modeling strategies for improved prognostic prediction. Statist Med. 1984;3:3143–52. doi: 10.1002/sim.4780030207. [DOI] [PubMed] [Google Scholar]