Abstract
CONTEXT
Despite theoretical concerns that health care related distrust may lead to poor health outcomes by interfering with effective health care, little is currently known about the prevalence or outcomes of distrust of the health care system in the United States.
OBJECTIVE
To investigate the association between distrust of the health care system and self-reported health status among the general population in the United States.
DESIGN
Random-digit-dialing telephone survey.
PARTICIPANTS
Nine hundred and sixty-one adult residents of the continental U.S.
PRIMARY MEASURES
Distrust of the health care system and self-reported health status.
RESULTS
Distrust of the health care system is relatively high in the United States, with between 20% and 80% of respondents reporting distrust for each item on the Health Care System Distrust scale and a median scale score of 31 (potential range from 10 to 50). Distrust of the health care system is strongly associated with self-reported fair/poor health (odds ratio [OR] 1.40%, 95% confidence interval [CI] 1.12 to 1.75 for each standard deviation increase in distrust), even after adjusting for sociodemographic characteristics, access to health care and trust in primary physicians. In contrast, low trust in one's primary physician is much lower (only 10% to 20% of respondents reported distrust for each item) and is not associated with health status.
CONCLUSIONS
Distrust of the health care system is relatively high in the general population in the United States and is strongly associated with worse self-reported health. Further studies are needed to assess the direction of this association and the mechanisms involved.
Keywords: distrust, health status
Although the influences of trust and distrust on many aspects of society are well described,1–4 interest in health care-related trust and distrust is comparatively recent and the effects of these phenomena less well understood. Theoretically, trust and distrust influence the frequency and “cost” of transactions.5,6 In settings of high trust, transactions occur more easily and fewer resources are needed for “monitoring, negotiating, litigating, and enforcing formal agreements.”7 In settings of high distrust, transactions are infrequent and transactional costs are higher. These concepts can be directly extended to health care. Patients who have higher levels of health care related trust in should be more likely to seek health care and accept health care recommendations. Health care transactions should be more effective because of better information exchange and stronger relationships. Patients with high levels of health care-related distrust in should be more likely to avoid health care, less likely to maintain continuity of care, and more likely to need to monitor and verify their health care decisions.
Despite this theoretical foundation, there is relatively little empirical evidence about the effects of health care trust and distrust on the functioning and outcomes of the health care system.8–11 Most prior research on health care related trust and distrust has focused on trust in physicians—a form of interpersonal trust—with the majority of efforts directed at understanding the determinants rather than the outcomes of this phenomenon.12–15 Despite evidence from other disciplines suggesting that broad forms of social trust may have the strongest effects on individual and group outcomes,7 studies examining institutional trust have focused on specific segments of the health care system, such as distrust of medical research16 or health insurers17–19 or hospitals,19 rather than broader forms of distrust such as distrust of the health care system. Furthermore, it has only recently been recognized that distrust may not be captured by instruments focusing solely on trust, as it is more negative than the absence of trust alone.20,21
In this paper, we report the results of a national survey to assess the prevalence of distrust of the health care system in the United States and to determine if health care system distrust is associated with self-reported health. We chose to examine the association between distrust and health status in order to demonstrate the potential public health impact of health care system distrust and to provide the framework for studies of the pathways by which distrust affects health. We used the Health Care System Distrust Scale that we had previously developed22 and compared the association between health status and health care system distrust with the association between health status and trust in personal physicians.23 In addition, we examined sociodemographic and health care access variables that correlated with health care system distrust.
METHODS
Study Design and Sample
We conducted a national random digit dialing telephone survey between November 2001 and January 2002. The sample was designed to generalize to the continental U.S. adult population among households with telephones. The study was approved by the University of Pennsylvania Institutional Review Board.
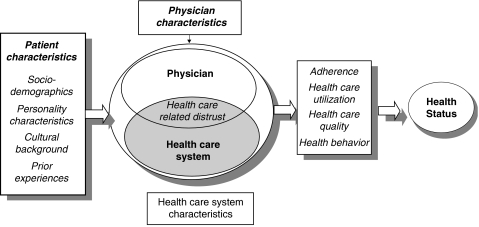
Figure 1.
Conceptual model of health care distrust
Data Collection
Interviews were conducted in English staggered over times of day and days of the week. In each household, interviewers asked for the youngest adult male at home. If no male was available, interviewers asked for the oldest female at home. This systematic respondent selection technique produces samples that closely mirror the population in terms of age and gender.24 We completed 961 interviews, with a contact rate (the proportion of working numbers where a request for interview was made) of 72%, a cooperation rate (the proportion of requests where consent was obtained) of 60%, and a completion rate of 99%.
Measures
Distrust of the Health Care System
We used the 10-item Health Care System Distrust scale to assess distrust of the health care system. The scale development has been published previously.22 In brief, the development process used focus groups of the general public in Philadelphia to define the dimensions of health care system distrust and develop an introductory definition of the health care system (hospitals, health insurance companies, and medical research). Potential items corresponding to these dimensions were generated from focus groups and existing scales of physician trust.13,25 Pilot testing using think-aloud exercises was used to refine the draft items. The final scale was determined through a pilot survey of 400 individuals in Philadelphia. Four distrust dimensions were identified (honesty—items a, d, e, j; confidentiality—items b, f; competence—items c, h; and fidelity-items g, i). Final scale scores had an internal consistency of 0.75, item-total correlations ranged between 0.27 and 0.57 and 1 general component accounted for 32% of the variance.22 Scale scores correlated positively with higher education, age, and African-American race.
Trust in Primary Physicians
We measured the respondent's trust in their primary physician using the 7 item trust subscale of the Primary Care Assessment Survey (PCAS) (Appendix A).23 This scale has a Cronbach's α of 0.86, range of item-total correlations of 0.49 to 0.73, and no substantial floor and ceiling effects.23
Health Status
Self-reported health was measured with the General Health Perceptions question that asks participants to characterize their health as excellent, very good, good, fair, or poor.26 This item is highly correlated with longer measures of health status, morbidity, and mortality.27–29
Health Care Access
Items from the Behavioral Risk Factor Surveillance System 2001 questionnaire (BRFSS) were used to assess access to health care in general, including insurance coverage, usual source of health care, and existence of a primary health care provider.30
Sociodemographic Characteristics
Sociodemographic characteristics, including age, education, and household income, were measured using items from the 2001 BRFSS.30 Items assessing race and ethnicity were based on the 2000 U.S. Census.31
Statistical Analysis
Data analysis was performed using STATA 7.0. All P-values are 2-sided. To assess the association between distrust and health status, bivariate analyses were conducted to identify correlates of health status followed by logistic regression with health status (fair/poor vs good/very good/excellent) as the dependent variable. In addition to distrust of the health care system, the potential correlates of health status included trust in physicians, sociodemographic characteristics (age, race, gender, educational attainment, and household income) and measures of access to health care (health insurance coverage, source of health care, having a primary provider). Because distrust of the health care system and trust in physicians were moderately correlated, we constructed separate models to assess the association between each of these variables and health status. However, the coefficients for the trust and distrust measures were essentially unchanged when both measures were added to the same regression. Thus, we present the model that includes both distrust of the health care system and trust in physicians. Scale scores were standardized (mean 10, standard deviation 1) to allow comparison of the coefficients for health care system distrust and trust in physicians.
To evaluate potential correlates of distrust of the health care system, we used independent sample t tests and 1-way analysis of variance followed by ordinary linear regression with distrust of the health care system as the dependent variable. Potential correlates included the sociodemographic characteristics and measures of access to care listed above. Variables were retained in the model if they were correlated with distrust (P < .05) or changed the coefficient for another variable by 15% or more. Because distrust was correlated with health status in the models described above, we also assessed the effect on these associations of adjusting for health status.
RESULTS
The 961 participants were predominantly Caucasian with a mean age of 47 and a wide range of educational attainment and household income (Table 1). Over 80% had health insurance and over three-quarters had a primary physician. Seventy-three percent said their usual source of care was a private doctor's office. Self-reported health status was widely distributed across the sample with 16% of individuals reporting excellent health, 38% reporting very good health, 29% reporting good health, 14% reporting fair health, and 3% reporting poor health. The mean score for the Distrust of the Health Care System scale was 30.5 (range 10 to 50). Between 20 and 80 percent of responses to individual items indicated distrust (Table 2). The mean score for the trust subscale of the PCAS was 28.8 (range 7 to 35), and less than 10% of responses to individual items indicated distrust. Distrust of the health care system was inversely correlated with trust in primary physicians (Pearson's correlation coefficient −0.34, P < 0.0001).
Table 1.
Subject Characteristics
| Percent of study population | Distrust of the Health Care System Scale Score (Range 10 to50) | ||
|---|---|---|---|
| Mean | P-Value | ||
| Age (y) | |||
| 18 to 30 | 21.7 | 28.7 | .001 |
| 31 to 40 | 22.2 | 31.4 | |
| 41 to 50 | 19.8 | 31.1 | |
| 51 to 60 | 15.1 | 31.4 | |
| 61 to 70 | 11.3 | 29.6 | |
| >70 | 10.0 | 29.5 | |
| Race/ethnicity | |||
| African American | 7.8 | 30.3 | .68 |
| Caucasian | 80.7 | 30.4 | |
| Hispanic | 5.9 | 30.0 | |
| Other | 5.6 | 32.3 | |
| Gender | |||
| Female | 52.3 | 30.3 | .52 |
| Male | 47.7 | 30.7 | |
| Education | |||
| Less than high school | 10.5 | 30.4 | .77 |
| High school only | 34.0 | 30.2 | |
| Some college | 24.0 | 30.9 | |
| College or higher | 31.5 | 30.2 | |
| Region | |||
| Northeast | 15.6 | 30.9 | .48 |
| Midwest | 26.0 | 29.9 | |
| South | 39.0 | 30.6 | |
| West | 19.4 | 30.8 | |
| Annual household income | |||
| < $20,000 | 18.0 | 30.5 | .94 |
| $20,000 to $39,999 | 30.0 | 30.1 | |
| $40,000 to $59,999 | 23.1 | 30.5 | |
| >$60,000 | 28.9 | 30.8 | |
| Health insurance | |||
| None | 13.8 | 31.7 | .04 |
| Government | 20.9 | 30.4 | |
| Private | 65.3 | 29.6 | |
| Personal health care provider | |||
| Yes | 78.6 | 30.5 | .81 |
| No | 21.4 | 31.0 | |
| Source of health care | |||
| Private clinic | 72.6 | 30.5 | .46 |
| Hospital-based clinic | 10.0 | 31.0 | |
| Public health clinic | 9.9 | 29.6 | |
| Emergency room | 5.3 | 29.5 | |
| Self-reported health | |||
| Excellent | 16.1 | 29.4 | .001 |
| Very good | 37.6 | 30.4 | |
| Good | 29.0 | 30.0 | |
| Fair | 14.0 | 32.4 | |
| Poor | 3.3 | 34.5 | |
Table 2.
Distrust of the Health Care System Scale Responses
| Strongly Agree (%) | Agree (%) | Not Sure (%) | Disagree (%) | Strongly Disagree (%) | |
|---|---|---|---|---|---|
| (a) Medical experiments can be done on me without my knowing about it | 16 | 20 | 3 | 19 | 42 |
| (b) My medical records are kept private | 33 | 30 | 3 | 18 | 15 |
| (c) People die every day because of mistakes by the health care system | 49 | 33 | 2 | 9 | 7 |
| (d) When they take my blood, they do tests they do not tell me about. | 17 | 19 | 6 | 22 | 35 |
| (e) If a mistake were made in my health care, the health care system would try to hide it from me | 26 | 32 | 5 | 21 | 17 |
| (f) People can get access to my medical records without my approval | 25 | 29 | 4 | 13 | 28 |
| (g) The health care system cares more about holding costs down than it does about doing what is needed for my health | 37 | 27 | 5 | 15 | 16 |
| (h) I receive high quality medical care from the health care system. | 38 | 41 | 3 | 9 | 9 |
| (i) The health care system puts my medical needs above all other considerations when treating my medical problems | 17 | 33 | 5 | 22 | 24 |
| (j) Some medicines have things in them that they do not tell you about | 39 | 32 | 3 | 14 | 13 |
(b), (h), and (i) are reverse scored to measure distrust.
Gray shading indicates responses consistent with distrust.
The next questions are about your opinion of the health care system in general. When we refer to the health care system, we mean hospitals, health insurance companies, and medical research.
Distrust of the health care system was associated with self-reported health status in unadjusted analyses (Table 1) and this association persisted after adjustment for age, gender, race, educational attainment, household income, health care access, and trust in physicians. (Table 3) Each 1 point increase in the standardized distrust score was associated with a 40% increase in the odds of fair/poor health. When examining the 4 previously specified dimensions of distrust,22 fair/poor health status was more strongly associated with honesty (P =.001) and competence (P =.02) than with confidentiality (P =.24) and fidelity (P =.39). Health status was not associated with trust of primary physicians in bivariate or multivariate analyses.
Table 3.
Multivariate Analysis of Variables Associated with Poor/Fair Self-Reported Health Status
| Odds Ratio | 95% CI | P-Value | |
|---|---|---|---|
| Health care system distrust* | 1.40 | 1.12 to 1.75 | .003 |
| Trust in personal physician*,† | 0.92 | 0.74 to 1.12 | .40 |
| Sociodemographic characteristics | |||
| Age (each decade increase) | 1.26 | 1.11 to 1.43 | < .0005 |
| Female | 1.37 | 0.90 to 2.10 | .14 |
| Race | |||
| Caucasian‡ | 1.00 | ||
| African American | 2.23 | 1.11 to 4.48 | .02 |
| Hispanic | 2.21 | 1.01 to 4.88 | .04 |
| Other | 0.94 | 0.36 to 2.47 | .90 |
| College degree or higher | 0.42 | 0.27 to 0.65 | < .0005 |
| Household income >60 K | 0.20 | 0.09 to 0.44 | < .0005 |
| Health care access | |||
| Lack of insurance | 0.86 | 0.42 to 1.73 | .67 |
| ED/public clinic as source of care | 1.61 | 0.84 to 3.07 | .15 |
Odds ratio associated with each 1 point increase in distrust (or trust) on standardized scale.
Among individuals with a personal doctor.
Reference category.
CI, confidence interval.
In unadjusted analyses examining the correlates of distrust, distrust of the health care system was highest among participants who were between 31 and 60 years of age and participants who did not have health insurance (Table 2). Overall distrust scores did not vary by race, although there was a suggestion of greater concerns about honesty among African Americans (mean score on honesty items 12.9 vs 12.0, P =.07). Distrust was not significantly associated with gender, education, household income, or source of health care. The association between age, health insurance coverage and distrust remained after multivariate adjustment, including adjustment for trust in primary physicians (Model 1) and adjustment for health status (Model 2) (Table 4).
Table 4.
Multivariate Analysis of Variables Associated with Level of Distrust of the Health Care System
| Adjusted Mean Difference in Distrust Score‡ (P-Value) | |||
|---|---|---|---|
| Model 1 | Model 2 | ||
| Sociodemographics | |||
| Age (y) | |||
| 18 to 30* | — | ||
| 31 to 40 | 2.15 (.02) | 2.13 (.02) | |
| 41 to 50 | 2.78 (.002) | 2.70 (.002) | |
| 51 to 60 | 2.47 (.008) | 2.28 (.01) | |
| 61 to 70 | 2.00 (.06) | 1.91 (.07) | |
| >70 | 2.04 (.10) | 2.18 (.08) | |
| Race/Ethnicity | |||
| Caucasian* | — | ||
| African American | 0.53 (.62) | 0.33 (.76) | |
| Hispanic | −0.34 (.77) | −0.59 (.62) | |
| Other | 2.10 (.09) | 2.02 (.10) | |
| Health care access | |||
| Health insurance | |||
| None* | — | ||
| Government | −1.95 (.04) | −2.26 (.05) | |
| Private | −2.04 (.03) | −1.81 (.05) | |
| Trust in personal physician† | |||
| Each 1 point increase | −0.47 (.001) | −0.46 (.001) | |
| Health status | |||
| Fair/poor vs good/very | 2.00 (.01) | ||
| Good/excellent | |||
Reference category.
Among individuals with a personal doctor.
Adjusted for gender, educational attainment.
DISCUSSION
This national survey demonstrates that distrust of the health care system is common in the United States, that it correlates with age and health insurance coverage, and, perhaps most importantly, that it is strongly associated with worse self-reported health, even after adjusting for age, sex, race, education, income, and insurance coverage. This finding is important for several reasons. First, the high prevalence of distrust and the strength of its association with health suggest that health care system distrust may be an important public health issue in the United States. Among our sample, the effect of an increase of 1 standard deviation in distrust was of similar magnitude (OR 1.40) as the effect of aging by 10 years (odds ratio [OR] 1.26). Although trust in physicians has generated more attention from health researchers to date, distrust of the health care system was both more prevalent and more strongly associated with health status than low trust in personal physicians. Second, the association between health care system distrust and health raises the possibility that health care distrust may be an important mediator or confounder of the widely publicized relationship between social capital and health.32–34 Levels of social trust have been demonstrated to be associated with several different measures of health, but the pathways for this relationship are not well understood. We are currently conducting studies to explore the contribution of health care system distrust to this relationship. Third, demonstrating a strong association between health care system distrust and health status suggests that reducing health care system distrust may represent a relatively unexplored avenue for improving health in the United States and provides both the impetus and justification for studies to explore the mechanisms underlying this association.
Although we believe that demonstrating an association between health care system distrust and health status is important, it is also important to recognize that this association does not prove that health care system distrust causes poor health. Several other potential explanations for the observed association should be considered. Individuals with worse health are likely to have more contact with the health care system and more negative experiences leading to negative attitudes about health care.35,36 Alternatively, distrust of the health care system may be a marker for some other factor that causes poor health. We adjusted for major socioeconomic factors that are associated with health outcomes, but there may be residual differences in socioeconomic status between high and low distrust individuals that contribute to differences in self-reported health. Furthermore, individual psychological factors, such as cynicism, depression, and locus of control were not measured and may contribute to the association between distrust and poor health status.
This study does not prove causality. However, there are several reasons to believe health care system distrust may lead to poor health. Distrust has been demonstrated to interfere with the effective functioning of many different segments of society.2,20,37 Similarly, health care related distrust may interfere with the effective functioning of the health care system, by leading to lower rates or delayed utilization of beneficial health care services, such as preventive health care, as well as increased use of unnecessary and potentially harmful health care services. Prior studies have demonstrated that other forms of trust and distrust are associated with differences in health care.15,38,39 Furthermore, because several studies suggest that distrust may be greatest for research institutions, distrust may preferentially act as a barrier to certain types of specialized care, including the use of high volume hospitals or providers, which may in turn result in lower quality care.16,40,41 Given that distrust of the health care system was associated with poor health status even in the setting of relatively high levels of trust in personal physicians, it is likely that some of these pathways affect health care without making patients distrust their personal physician.
In contrast to distrust of the health care system, low trust in one's primary physician was neither prevalent nor associated with health status. The high level of trust in primary physicians is similar to the findings of several prior studies.13,38,42 However, prior studies have documented modest associations between trust in primary physicians and health behaviors, primarily adherence to screening and treatment regimens, short-term symptom resolution and, in 1 study, physical health.11,15,17,39 The lack of association between trust in personal physicians and health status in this study may reflect a ceiling effect in the trust measure or the specific characteristics of the study population. It raises the possibility that differences in health behavior or short-term outcomes in prior studies may not translate into long-term effects on health. One potential explanation for that patients with low trust in physicians can and do change their physicians,14 thus limiting the duration of the “exposure.”
We found that distrust of the health care system is higher among individuals who do not have health insurance and individuals between 31 and 60 years of age. Our clinical experience suggests that patients without health insurance are more likely to experience conflicts with the health care system, less continuity of care, and lower quality care—factors that may increase distrust. Alternatively, it is possible that individuals who distrust the health care system are less likely to seek health insurance. Younger individuals may have less health care contact and be less likely to have had negative experiences. Age differences may reflect generational effects with some reports suggesting generally high levels of disaffection among the Baby Boom generation (individuals 40 to 60 years of age).43
Despite the widespread anecdotal reports of high levels of health care related distrust in minority groups, distrust of the health care system did not differ across racial/ethnic groups in this study, although there was a trend towards greater concerns about dishonesty among African Americans. This lack of racial difference was also seen in a national survey of general trust in physicians but differs from several other studies of physician trust.44,45 our sample included relatively few minority but provided over 90% power to detect a difference of 0.4 standard deviations between African Americans and Caucasians, often considered a relatively small effect size. Furthermore, in unadjusted analyses, the mean level of distrust was slightly lower among African Americans (30.2) and Hispanics (30.3) than among Caucasians (30.5). Although this suggests there are unlikely to be large differences in the overall scores on the Health Care System Distrust Scale, significant racial differences may still exist in specific dimensions of distrust (e.g., honesty) or other types of distrust. For example, distrust of medical research, may be particularly prevalent among African Americans.16,46 One prior study demonstrated that trust in hospitals was higher among Caucasians but trust in insurers was higher among African Americans.19 In addition, we did not create a Spanish version of the questionnaire and thus were unable to include individuals who spoke only Spanish. If these individuals are more likely to distrust the health care system, we may have underestimated the prevalence of distrust among Latinos.
This study has several limitations. We used a single item to measure health status. However, this item is highly predictive of both disability and mortality in multiple studies.27–29 Although we used established scales, trust and distrust are complex concepts that are difficult to measure. The imperfect nature of our measures may have contributed to the lack of association between trust in physicians and health status. We were only able to include individuals with working telephones. Individuals without telephones may differ from our sample in important ways, including potentially higher levels of distrust. Furthermore, it is possible that nonresponders differed from responders. If nonresponders have higher levels of distrust, we may have underestimated the prevalence of distrust of the health care system in the United States. Alternatively, if responders are more likely to have participated because of grievances about the health care system, we may have overestimated the prevalence of distrust.
Despite these limitations, this study provides the first empirical evidence that distrust of the health care system is both relatively common and associated with worse self-reported health. Further studies are needed to determine whether this association between health care system distrust and health is causal and the pathways by which it may occur. Ultimately this information is only useful if distrust of the health care system can be modified and health improved.
Acknowledgments
Larry Hugick, Margie Engle, and Jonathan Best of Princeton Survey Research Associates
Support: Dr. Armstrong is supported by an American Cancer Society Research Scholar Grant, a Robert Wood Johnson Generalist Faculty Scholar Award and RO1 2689-01 from the National Human Genome Research Institute.
REFERENCES
- 1.Coleman J. Foundation of Social Theory. Cambridge, MA: Harvard University Press; 1990. [Google Scholar]
- 2.Zak P, Knack S. Trust and growth. Econ J. 2001;111:295–321. [Google Scholar]
- 3.Tyler T. Why do people rely on others? Social identity and social aspects of trust. In: Cook K, editor. Trust in Society. II. New York: Russell Sage Foundation; 2001. pp. 285–307. [Google Scholar]
- 4.Dunn J. Trust and political agency. In: Gambetta D, editor. Trust: Making and Breaking Cooperative Relations. Oxford: Blackwell; 1988. pp. 73–93. [Google Scholar]
- 5.Hardin R. Conceptions and explanations of trust. In: Cook K, editor. Trust in Society. II. New York: Russell Sage Foundation; 2001. pp. 3–40. [Google Scholar]
- 6.Lewicki RJ, Bunker BB. Developing and maintaining trust in work relationships. In: Kramer RM, Tyler TR, editors. Trust in Organizations: Frontiers of Theory and Research. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- 7.Fukuyama F. Social Capital: Civic Community, Organization and Education. Washington, DC: IMF Conference on Second Generation Reforms, IMF Headquarters; 1999. [Google Scholar]
- 8.Mechanic D. The functions and limitations of trust in the provision of medical care. J Health Polit Policy Law. 1998;23:661–87. doi: 10.1215/03616878-23-4-661. [DOI] [PubMed] [Google Scholar]
- 9.Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Quart. 2001;79:613–39. doi: 10.1111/1468-0009.00223. v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goold SD. Trust and the ethics of health care institutions. Hastings Cent Rep. 2001;31:26–33. [PubMed] [Google Scholar]
- 11.Pearson SD, Raeke LH. Patients' trust in physicians: many theories, few measures, and little data. J Gen Intern Med. 2000;15:509–13. doi: 10.1046/j.1525-1497.2000.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thom DH, Physicians TSTS. Physician behaviors that predict patient trust. J Fam Pract. 2001;50:323–8. [PubMed] [Google Scholar]
- 13.Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients' trust in their physicians. J Gen Intern Med. 1998;13:681–6. doi: 10.1046/j.1525-1497.1998.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keating NL, Green DC, Kao AC, Gazmararian JA, Wu VY, Cleary PD. How are patients' specific ambulatory care experiences related to trust, satisfaction, and considering changing physicians?[see comment] J Gen Intern Med. 2002;17:29–39. doi: 10.1046/j.1525-1497.2002.10209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Malley AS, Sheppard VB, Schwartz M, Mandelblatt J. The role of trust in use of preventive services among low-income African-American women. Prev Med. 2004;38:777–85. doi: 10.1016/j.ypmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 16.Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Intern Med. 2002;162:2458–63. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 17.Balkrishnan R, Dugan E, Camacho FT, Hall MA. Trust and satisfaction with physicians, insurers, and the medical profession. Med Care. 2003;41:1058–64. doi: 10.1097/01.MLR.0000083743.15238.9F. [DOI] [PubMed] [Google Scholar]
- 18.Zheng B, Hall MA, Dugan E, Kidd KE, Levine D. Development of a scale to measure patients' trust in health insurers. Health Serv Res. 2002;37:187–202. [PubMed] [Google Scholar]
- 19.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Rep. 2003;118:358–65. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kramer RM. Trust and distrust in organizations: emerging perspectives, enduring questions. Am Rev Psychol. 1999;50:569–98. doi: 10.1146/annurev.psych.50.1.569. [DOI] [PubMed] [Google Scholar]
- 21.Goold SD. Trust, distrust and trustworthiness. J Gen Intern Med. 2002;17:79–81. doi: 10.1046/j.1525-1497.2002.11132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rose A, Shea JA, Armstrong K. Development of the health care system distrust scale. J Gen Inter Med. 2004;19:57–63. doi: 10.1111/j.1525-1497.2004.21146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Safran DG, Kosinski M, Tarlow AR, et al. The primary care assessment survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Troldahl V, Carter R. Random selection of respondents within households in phone surveys. J Market Res. 1964;1:71–6. [Google Scholar]
- 25.Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the trust in physician scale. The stanford trust study physicians. Med Care. 1999;37:510–7. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Ware JE, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the medical outcomes study. Med Care. 1995;33:64–79. [PubMed] [Google Scholar]
- 27.Mossey J, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982;72:800–8. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Idler E, Angel R. Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. Am J Public Health. 1990;80:446–52. doi: 10.2105/ajph.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Connelly J, Philbrick J, Smith G, Kaiser D, Wymer A. Health perceptions of primary care patients and the influence on health care utilization. Med Care. 1989;27:S99–S109. doi: 10.1097/00005650-198903001-00009. [DOI] [PubMed] [Google Scholar]
- 30.Behavioral Risk Factor Surveillance System: Center for Disease Control. 2001. [Google Scholar]
- 31.Grieco E, Cassidy R. Overview of Race and Hispanic Origin: Census 2000 Brief. Washington, DC: U.S. Census Bureau, U.S. Department of Commerce; 2001. [Google Scholar]
- 32.Kawachi I, Kennedy B, Glass R. Social capital and self-related health: a contextual analysis. Am J Public Health. 1999;89:1187–93. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kawachi I, Kennedy B, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87:1491–8. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Subramanian SV, Kim DJ, Kawachi I. Social trust and self-rated health in US communities: a multilevel analysis. J Urban Health. 2002;79:S21–34. doi: 10.1093/jurban/79.suppl_1.S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cleary P, Edgman-Levitan S, Roberts M, Moloney TWM, Delbanco T. Patients evaluate their hospital care: a national survey. Health Aff. 1991;10:254–67. doi: 10.1377/hlthaff.10.4.254. [DOI] [PubMed] [Google Scholar]
- 36.DeSalvo K, Fan V, McDonell M, Fihn S. Predicting mortality and healthcare utilization with a single question. Health Serv Res. 2005;40:1234–46. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller G. Why is trust necessary in organizations? The moral hazard of profit maximization. In: Cook K, editor. Trust in Society. II. New York: Russell Sage Foundation; 2001. pp. 307–32. [Google Scholar]
- 38.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Barriers to influenza immunization in a low-income urban population. Am J Prev Med. 2001;20:21–5. doi: 10.1016/s0749-3797(00)00263-4. [DOI] [PubMed] [Google Scholar]
- 39.Thom DH, Kravitz RL, Bell RA, Krupat E, Azari R. Patient trust in the physician: relationship to patient requests. Fam Practice. 2002;19:476–83. doi: 10.1093/fampra/19.5.476. [DOI] [PubMed] [Google Scholar]
- 40.Yarborough M, Sharp RR. Restoring and preserving trust in biomedical research. Acad Med. 2002;77:8–14. doi: 10.1097/00001888-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Birkmeyer J, Siewers A, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 42.Thom D, Campbell B. Patient-physician trust: an exploratory study. J Fam Pract. 1997;44:169–76. [PubMed] [Google Scholar]
- 43.Robinson R, Jackson E. Is trust in others declining in America? An age-period cohort analysis. Soc Sci Res. 2001;30:117–45. [Google Scholar]
- 44.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37:1419–39. doi: 10.1111/1475-6773.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African-American and white cardiac patients. Med Care Res Rev. 2000;57:146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- 46.Gamble VN. A legacy of distrust: African Americans and medical research. Am J Prev Med. 1993;9:35–8. [PubMed] [Google Scholar]