Abstract
BACKGROUND
Incentive-based formularies have been widely instituted to control the rising costs of prescription drugs. To work properly, such formularies depend on patients to be aware of financial incentives and communicate their cost preferences with prescribing physicians. The impact of financial incentives on patient awareness of and communication about those costs is unknown.
OBJECTIVE
To evaluate the relationship between enrollment in incentive-based pharmacy benefit plans and awareness of out-of-pocket costs and rates of communication about out-of-pocket costs.
DESIGN
A matched telephone survey of patients and their primary care physicians.
SETTING
Los Angeles County.
PARTICIPANTS
One thousand nine hundred and seventeen patients aged 53 to 82 (73% response rate).
MEASUREMENTS
Patient-reported pharmacy benefit design, knowledge of out-of-pocket costs, and discussion of out-of-pocket costs with physicians.
RESULTS
Sixty-two percent of patients who had prescription drug coverage and were aware of their pharmacy benefit design reported being enrolled in incentive-based plans. The majority of these (54%) were “never” or only “sometimes” aware of their out-of-pocket cost requirements at the time of the physician visit. After controlling for numerous physician and patient level variables, we found that patients enrolled in pharmacy benefit designs requiring no copayments were more likely to report they “never” discuss out-of-pocket costs with physicians compared with patients enrolled in incentive-based pharmacy benefit designs (81% vs 67%, P =.001) and patients with no prescription druginsurance (57%, P <.001).
CONCLUSIONS
Incentive-based pharmacy benefit plans and lack of insurance are associated with increased rates of discussions about out-of-pocket costs. Nonetheless, most incentive-based enrollees are unaware of out-of-pocket costswhen prescriptions are written and never discuss out-of-pocket costs with their physicians, likely mitigating the effectiveness of financial incentives to guide decision making. Considering that out-of-pocket costs are associated with adherence to medical therapy, interventions to improve patient access to out-of-pocket cost information and the frequency of patient-physician discussions about costs are needed.
Keywords: pharmacy benefit design, prescription drugs, doctor patient communication, incentive-based
Over the past decade, insurers have broadly increased cost-sharing requirements and implemented multitiered, incentive-based formularies in hopes that market forces would help stem the rapidly rising cost of prescription drugs. By 2004, approximately 65% of Americans with employer-sponsored prescription drug benefits were enrolled in 3-tier plans.1 These plans utilize financial incentives in the form of tiered copayments to steer patients toward drugs they consider more cost-effective. Many policy makers believe this approach will lead to an “ownership society” in which educated consumers will be sensitive to medical care costs and communicate their preferences, leading to greater efficiency and cost management.2 The Medicare Modernization Act (MMA) has endorsed the creation of a marketplace to provide prescription drug coverage to seniors,3 likely increasing enrollment of seniors in tiered, incentive-based prescription drug plans.4
For incentive-based formularies to operate as intended, consumers must be aware of cost-sharing informationabout prescription drugs and communicate their preferences,5 or providers must be aware of such costs in order to make informed prescribing decisions. Recent studies have found that physicians are frequently unaware of their patients' formularies and out-of-pocket costs when prescribing.6,7 Therefore, providers must rely on patients to communicate their cost concerns at the time of prescribing or must depend on some other outside source, such as dispensing pharmacists or pharmacy benefits managers, to do so after the fact. Hence, discussions about the financial costs and clinical benefits of various medications at the time ofprescribing are key to making clinically and economically relevant cost/benefit decisions.8
The few studies that have tested whether patients and physicians discuss out-of-pocket costs when drug treatment decisions are made have found that these discussions occur rarely.8 However, it is unclear whether the use of incentive-based pharmacy plans influences patient knowledge about such costs and/or affects the frequency of discussions between patients and clinicians. To address these issues, we interviewed physicians and their patients. First, we evaluated whether patients enrolled in incentive-based plans were aware of the out-of-pocket costs of their prescription drugs at the time thatprescriptions were written. Second, we studied whether enrollment in incentive-based pharmacy benefit plans orlack of prescription drug insurance affected the likelihood that patients would discuss out-of-pocket cost requirements with their physicians.
METHODS
Sampling
We performed a matched telephone survey of patients selected from primary care physician patient panels in 2003. We utilized the sampling frame of a previous survey, performed in 2000, which assessed physicians participating in an intervention to improve physician-patient communication about cancer screening. Eligible subjects were patients managed by family medicine/general practice, and general internal medicine physicians who participated in the 2000 survey.
The primary care physicians who participated in the 2000 survey were identified from the American Medical Association Physician Masterfile. As an important study focus was on Latino versus non-Latino physician comparisons, the AMA Masterfile was supplemented by the Latino Physicians Directory due to concern about Latino physician underrepresentation. It was our belief that many minority physicians practice in areas of high concentrations of patients of the same ethnicity. We sampled physicians from areas of Los Angeles County with high concentrations of Latinos and, although physicians of all ethnicities were sampled, we felt this strategy would help ensure an adequate number of Latino physicians to allow for meaningful analytic comparisons. In total, 111 physicians responded to the baseline survey and comprise the eligible sample for this survey.
We enumerated patients aged 50 to 79 who had an appointment with a physician in our sample between October and November of 1999. On average, 110 patients were identified from each physician. Those patients were contacted for the baseline survey in 2000, and a total of 3,172 participated. Of those, 2,622 patients were presumedeligible for the follow-up survey in 2003 (the other 550 could not be interviewed because of intervening death, incapacitation, or inability to reach the patient), and 1,917 participated representing a response rate of 73%.
Because of concerns that the survey was too time-consuming for patients, approximately 11% of patients received an abbreviated survey that excluded the survey item that identified patient's pharmacy benefit structure. There were no particular patient characteristics associated with receiving the abbreviated survey. This resulted in 1,707 participants being available for multivariate analyses. Respondents were similar to nonrespondents in terms of age, but Hispanic, Asian and male patients were less likely to participate in the survey.In addition, patients without a high school degree were less likely to participate while those with graduate work were more likely.
Survey Instrument
The baseline physician survey in 2000 included questions concerning demographics, training, practice setting and practice characteristics, and was updated in our follow-up survey in 2003.
The patient survey explored patient demographics, education, income, self-reported health, presence of chronic conditions, and insurance coverage. We asked patients to report whether they had any prescription drug insurance coverage (yes/no). For those with prescription drug insurance, we asked patients to identify their pharmaceutical benefit design (i.e., no copayments, single copayment for all medications, different copayments for different drugs [tiered, or incentive-based, copayments] or “don't know”). Among patients enrolled in tiered benefits, we asked how often they were familiar with their out-of-pocket costs at the time of prescribing. Finally, we ascertained the frequency that patients enrolled in each pharmacy benefit designdiscuss out-of-pocket costs of prescription drugs with their physicians. The variables of interest were structured on a 4-point Likert scale. Survey questions focused on “new” prescriptions because this is the most likely time for discussion of out-of-pocket costs for chronic medications.
Analysis
Survey data were analyzed with Intercooled STATA 8.1 software.9 Information about physician characteristics was derived from the baseline survey. The baseline survey was used to estimate physician characteristics for patients who reported that they are seeing a new primary carephysician because we have no demographic information about their most recent physician. A sensitivity analysisexcluding patients who reported they changed their primary care physician did not significantly affect the results.
Multiple logistic regression was used to estimate the influence of patient, physician, and pharmacy benefitdesign factors on the likelihood that patients discuss out-of-pocket costs with their physicians. Patients whoreported that they discuss out-of-pocket costs with their physicians “sometimes,”“usually,” or “always” were categorized as communicating out-of-pocket costs. Patients who responded to the abbreviated survey were dropped from this portion of the analysis because we did not have data on their pharmacy benefit design. We calculated the relative risks associated with each independent variable representing the relative likelihood that patients report they discuss out-of-pocket costs with their physicians. We calculated 95% confidence intervals (CIs) for relative risks using the bootstrap method.10 Standard errors were adjusted for clustering at the physician level using generalized estimating equations. We also performed a sensitivity analysis and included a dummy variable for those who were not asked about their pharmacy benefit design and found no qualitative change in the results.
We then estimated ordered logit models to further explore the relationship between pharmacy benefit structure and rates of communication about cost. Ordered logit models permit full use of information provided by an ordered scale. Communication rates were collapsed into 3 mutually exclusive categories: “Never,”“Sometimes,” and “Usually or Always.” The ordered logit model was used to predict the effect of pharmacy benefit design on discussion rates of out-of-pocket costs. We used the bootstrap method to generate 95% CIs to test for statistically significant differences in rates of communication by typeof pharmacy benefit design. The model was clustered at the physician level and passed the test of proportionalodds (P =.224).
RESULTS
Patient and Physician Characteristics
The average age of physicians in the sample was 50 and over; 40% were foreign medical graduates. (Table 1) Approximately 68% of participating physicians were male. Hispanic physicians were overrepresented in our sample compared with the national average, comprising almost29% of the sample.11
Table 1.
Physician, Patient, and Physician-Patient Relationship Characteristics
| Physicians (n=111) | Mean * or Percentage |
|---|---|
| Male | 67.6% |
| Patients seen per day | 25.4 (±10.9) |
| Age | 50.1 (±9.3) |
| Race | 40.5% non-Hispanic White |
| 7.2% African American | |
| 21.6% Asian | |
| 28.8% Hispanic | |
| 1.8% other race | |
| Foreign medical graduate | 40.5% |
| Practice setting | 46.0% private solo practice |
| 24.3% private group practice | |
| 2.7% community clinic | |
| 22.5% staff model HMO | |
| 2.7% IPA or PPO | |
| 1.8% other |
| Patients ( n=1,707) | Mean * or Percentage |
|---|---|
| Education | 23.5% less than high school |
| 21.7% high school | |
| 24.3% some college | |
| 15.0% college grad | |
| 14.5% graduate school | |
| Income | 25.8% less than $15,000 |
| 26.1%$15 to 35,000 | |
| 29.9%$35 to 75,000 | |
| 18.2% greater than $75,000 | |
| Male | 33.3% |
| Age | 67.2 (±8.18) |
| Race | 52.6% White |
| 9.6% African American | |
| 4.2% Asian | |
| 32.7% Hispanic | |
| 1.0% other race | |
| Self-reported health | 7.2% poor |
| 23.2% fair | |
| 32.9% good | |
| 25.5% very good | |
| 11.1% excellent | |
| Has a chronic condition | 79.1% |
| Type of pharmacy benefit | 21.3% no coverage |
| 10.0% no copayments | |
| 17.8% single copayment for all drugs | |
| 44.5% tiered copayments | |
| 6.4% do not know |
| Patient physician relationship | |
|---|---|
| Gender concordance | 54.5% |
| Race concordance | 64.5% |
±SD.
PPO, preferred provider organization; HMO, health maintenance organization; IPA, independent provider association.
Of the 1,707 patients included in our multivariate analyses, the average age was 67% and 33% were male. (Table 1) Almost 53% were non-Hispanic white, 33% Hispanic, and 10% African American. Nearly 80% of patients reported that they had at least1 chronic condition, suggesting that most purchase prescription drugs. Approximately 72% of patients reported they continue to see their primary care physician identified in the 2000 baseline survey, and 28% indicated they receive their primary care from a new physician. Over half (55%) of patient-physician pairs were concordant by gender, and 65% were concordant by race.
Type of Prescription Coverage
Approximately 21% of patients surveyed stated that they had no insurance to help pay for prescription drugs. Almost 45% of patients reported that they were enrolled in tiered, or incentive-based, pharmacy benefit plans and are charged different copayments for different medications. Ten percent of patients surveyed reported they paid no copayments, 18% paid a single copayment for all medications, and 6% of patients did not know about their coverage. As a percentage of those with pharmaceutical coverage who were aware of their benefit design, 62% of patients were enrolled in tiered benefits, slightly lower than the national average.1
Patient Knowledge of Out-Of-Pocket Costs and Rates of Patient-Physician Discussions About Those Costs at the Time of Prescribing
Among patients enrolled in tiered benefit structures (n=745), most reported that they were either never or only sometimes aware of out-of-pocket costs at the time of prescribing. Approximately 38% of patients reported they never know their out-of-pocket costs and 16% were only sometimes knowledgeable.
All 1,917 patient participants were asked how frequently they discussed out-of-pocket costs with their physicians when new prescriptions were written. Over 68% of patients reported that they never discussed out-of-pocket costs with their physicians, 18% reported that they sometimes engaged in discussions, 6% discussed costs most of the time, and 8% always discussed costs.
Factors That Influence Whether Patients Report That They Ever Discuss Out-Of-Pocket Costs With Physicians
In our multiple logistic regression model, few variables significantly affected the likelihood that patients and physicians discuss out-of-pocket costs. Physician age, gender, ethnicity, and country of medical education did not affect the likelihood of discussions about costs, nor did patient age, gender, self-reported healthstatus, or the presence of a chronic medical condition (Table 2). No consistent trend was seen in patient income. Gender and race concordance between physicians and patients did not influence discussion rates. However, Hispanic patients were 28% less likely to discuss out-of-pocketcosts (P =.003) than white patients, patients with a graduate school education were 36% less likely to discuss costs than those who dropped out of high school (P =.008), older patients were less likely to communicate about out-of-pocket costs (P =.036), and patients enrolled in staff-model health maintenance organizations (HMOs) were over 34% less likely to discuss costs than patients with private, solo practitioners (P =.001).
Table 2.
Logistic Regression Results Evaluating Factors That Impact Whether Patients Discuss Out-of-Pocket Costs With Their Physicians
| Relative Risk* | 95% Confidence Interval† | |
|---|---|---|
| Physician | ||
| Male | 0.86 | 0.70 to 1.06 |
| Age‡ | 0.97 | 0.78 to 1.16 |
| Foreign medical graduate | 1.05 | 0.88 to 1.27 |
| Years in current practice‡ | 1.07 | 0.86 to 1.29 |
| Race | ||
| African American | 1.03 | 0.71 to 1.55 |
| Asian | 0.75 | 0.56 to 1.00 |
| Hispanic | 1.10 | 0.83 to 1.41 |
| Other race | 0.99 | 0.33 to 1.71 |
| Practice setting | ||
| Private group practice | 1.14 | 0.93 to 1.38 |
| Community clinic | 0.93 | 0.52 to 1.50 |
| Staff model HMO | 0.66§ | 0.53 to 0.84 |
| IPA | 0.92 | 0.45 to 1.46 |
| PPO | 1.50 | 0.46 to 2.55 |
| Patient | ||
| Male | 0.98 | 0.80 to 1.18 |
| Age‡ | 0.84§ | 0.72 to 0.996 |
| Self-reported health | ||
| Fair | 1.05 | 0.76 to 1.48 |
| Good | 1.06 | 0.77 to 1.48 |
| Very good | 0.96 | 0.70 to 1.39 |
| Excellent | 0.90 | 0.63 to 1.41 |
| Race | ||
| African American | 0.80 | 0.53 to 1.11 |
| Asian | 0.80 | 0.52 to 1.24 |
| Hispanic | 0.72§ | 0.57 to 0.96 |
| Other race | 0.96 | 0.34 to 1.86 |
| Chronic condition (y/n) | 1.21 | 0.98 to 1.52 |
| Income | ||
| $15 to 35,000 | 1.41§ | 1.14 to 1.78 |
| $35 to 75,000 | 1.18 | 0.87 to 1.52 |
| Greater than $75,000 | 0.83 | 0.57 to 1.13 |
| Education | ||
| High school | 0.80 | 0.64 to 1.04 |
| Some college | 0.88 | 0.70 to 1.14 |
| College | 0.84 | 0.64 to 1.14 |
| Grad school | 0.64§ | 0.45 to 0.90 |
| Pharmacy benefits | ||
| No coverage | 2.30§ | 1.57 to 3.37 |
| Single copayment | 1.15 | 0.75 to 1.76 |
| Tiered copayments | 1.71§ | 1.16 to 2.49 |
| Do not know | 1.79§ | 1.08 to 2.73 |
| Patient-Physician | ||
| Gender concordance | 0.96 | 0.78 to 1.16 |
| Race concordance | 0.88 | 0.72 to 1.09 |
Reference categories: Physician race (white), Patient Health (poor), Patient Race (non-Hispanic white), Patient Education (less than high school), Patient Drug Coverage (no copayments), Income (less than $15,000).
Relative risks: relative likelihood that patients report they engage in discussions about out-of-pocket costs with their physicians, as compared to the referent category.
Derived using bias-corrected bootstrap method.
Continuous variables evaluated at change from one standard deviation below to one standard deviation above mean value.
Boldface indicates statistically significant at the P<.05 level.
Complete Data Sample Size 1,647 (less than 2% missing values for frequency of communication, patient education, patient race, race concordance, and patient self-reported health).
PPO, preferred provider organization; HMO, health maintenance organization; IPA, independent provider association.
The variable that most powerfully predicted the likelihood that patients and physicians discuss out-of-pocket costs was the patients' pharmacy benefit design. Patients without prescription drug insurance coverage were 2.3 times more likely to discuss out-of-pocket costs with their physicians than patients paying no copayments (P <.001). Patients enrolled in incentive-based formularies were 1.7 times more likely to discuss costs (P =.002) and patients who did not know their type of pharmacy benefit structure were 1.8 times more likely to discuss out-of-pocket costs (P =.008) than patients charged no copayments. There was no statistically significant difference in discussion rates between patients charged a single copayment and patients charged no copayments for prescription drugs.
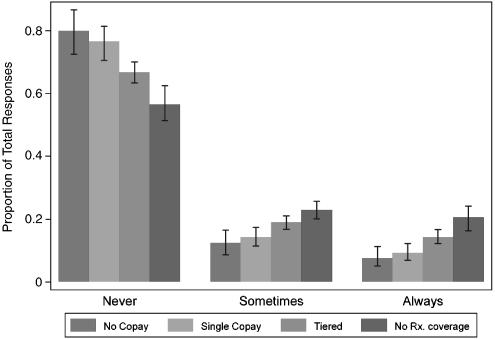
Predicted Rates that Patients and Physicians Discuss Out-Of-Pocket Costs, by Pharmacy Benefit Structure
Our ordered logit results also indicate that pharmacy benefit design significantly affects the likelihood that patients engage in discussions about costs. Figure 1 presents the relationship between pharmacy benefit design and cost discussions as adjusted rates. After controlling for patient and physician characteristics, we found that 77% of patients required to pay a single copayment for prescription drugs report that they never discuss out-of-pocket costs for prescription drugs. No significant difference was seen between patients enrolled in plans requiring a single copayment for all drugs and patients who paid no copayments for their medications (80%, P =.41). The rate that patients report they never discuss out-of-pocket costs declines to 67% in patients enrolled in incentive-based plans (P =.001) and 57% in patients with no insurance coverage for prescription drugs (P <.001). Patients that were unfamiliar with their copayment structure answered similarly to those enrolled in incentive-based designs; 66% never discussed out-of-pocket costs with their physicians. An evaluation of Figure 1 suggests that there is a dose-related relationship between exposure to out-of-pocket costs and communication rates about costs, with increasing cost exposure corresponding to increased communication rates.
Figure 1.
Rates at which patients report they discuss out-of-pocket costs with their physicians by pharmaceutical benefit system *. Results from ordered logit model, holding all other variables constant. *95% confidence intervals shown, derived by bootstrap method.
DISCUSSION
Our study indicates that patients who are enrolled in tiered, incentive-based pharmacy benefit designs are more likely to talk to their physicians about out-of-pocket costs for prescription drugs than patients who areenrolled in plans requiring a single copayment or no copayment at all. Nevertheless, a majority of patients enrolled in incentive-based benefit designs report that they are never or only sometimes aware of their out-of-pocket requirements for new prescription drugs at the time of prescribing, suggesting that incentives often fail to induce patients to use cost information to participate in decision making. Among patients enrolled in incentive-based pharmacy benefit systems, 67% report that they never talk to their physicians about out-of-pocket costs when new prescriptions are written. Even among patients without prescription drug coverage, who should be most sensitive to copayments, the majority (57%) never discuss out-of-pocket costs. Controlling for a wide array of physician and patient characteristics did not alter these conclusions.
Rather than discussing costs at the time of prescribing, many patients may learn about their cost-sharing requirements at the point of filling their prescription at the pharmacy, where prescriptions cannot easily be adjusted. These patients may be charged unnecessarily high copayments which likely lead to decreased utilization,12–18 and may adversely impact health outcomes.19,20 Decreased utilization may result from patients who find it difficult to advocate for themselves when their cost decisions are isolated in time from clinical benefit discussions, forcing them to ask their pharmacist, health plan, or physician for assistance. We found that Hispanic ethnicity and older age are associated with less frequent discussions of out-of-pocket costs with their physicians, suggesting that cultural, linguistic, or cognitive factors may also pose a barrier.
Patients enrolled in staff-model HMOs were also less likely to discuss out-of-pocket costs with their physicians. Physicians practicing in staff-model HMOs typically only prescribe from a single formulary. The challenges of prescribing in compliance with formularies are significantly attenuated in this setting,21 likely facilitating management of patients' costs. It is also possible that these plans more efficiently steer patients toward generic or preferred formulary agents, requiring less communication. In addition, patients with a graduate school education were less likely to discuss costs than high school dropouts, likely because our graduate school variable captured information about patient income, and greater income may be associated with less concern about costs.
A limitation of our study may be patients' inaccuracy in identifying their pharmaceutical benefit coverage, although only 6% of patients reported that they were unaware of their benefit design. A recent study evaluating patient knowledge of their pharmacy benefit design in a managed care setting found that patients were wrong about their type of benefit design approximately 25% of the time.22 Some patients may have guessed or overstated their knowledge of their prescription drug coverage. Patient misclassification of their pharmacy benefit design may have biased our study toward underestimating the effect of benefit design on communication rates. Two potential limitations result from our response rate of 73%. First, incomplete participation implies a smaller total sample size, which limits the precision of model estimates. Second, we cannot rule out the possibility that sample selection bias limits the generalizability of our findings, despite the robustness of the relationship between pharmacy benefit design and discussion rates about costs. In addition, our sample was limited to a physician and patient sample from a single geographic region, is not broadly generalizable, and ought to be confirmed elsewhere.
We also did not have current physician information for approximately one fifth of the patients sampled, those who reported that they changed their primary care physician as the baseline survey. Therefore, we may have conservatively estimated the relationship between physician characteristics and rates of communication about out-of-pocket costs, although our sensitivity analyses suggest that our findings are robust to this limitation.
Some may argue that communication about costs is unnecessary as long as physicians are aware of patients' out-of-pocket costs when prescribing and can serve as their financial agents, or patients, who learn about costs at the pharmacy, can ask to switch to a less expensive medication. Yet physicians are rarely aware of patient's formularies and out-of-pocket costs, and generally do not believe it is their responsibility to help patients manage out-of-pocket costs for prescription drugs.6 Patients are often unaware of their cost-sharing requirements and likely find it challenging to identify the particular medications that fall in each tier on their formulary. When patients are initiated on nonpreferred drugs from their formulary, they frequently ask the doctor to switch their prescription to a less expensive medication, yet initiation on more expensive medications has been shown to adversely affect subsequent adherence to chronic therapy.23
Overall, this study highlights strengths and shortfalls of the tiered, incentive-based pharmacy benefit design to increase patient cost sensitivity. Although incentive-based plans increase the likelihood that patients and physicians will discuss out-of-pocket costs for prescription drugs as intended, and likely increase patient awareness of these costs, most patients in tiered benefits still are unaware of their out-of-pocket cost requirements when prescribing decisions are made and a majority report that they “never” talk to their doctors about out-of-pocket costs.
This study highlights a key limitation of using market reforms and an “ownership society” to generate efficiencies in health care. If consumers are not aware of their cost-sharing requirements when health care decisions are made, these market reforms constitute post hoc penalties for patients who, along with their physicians, are least knowledgeable about costs. Until cost information is consistently available at point of service, then price incentives may not offer the most efficient and effective way to influence prescriptiondrug use. Systems improvements must be employed to guarantee that patients and physicians have access to cost information. As increasing numbers of seniors find themselves enrolled in incentive-based plans after implementation of the MMA, studies are needed to evaluate whether seniors are aware of their out-of-pocket expenses, whether they are communicating their preferences with physicians, and whether access to essential medications is impeded by out-of-pocket requirements.
Acknowledgments
This research is supported by a grant from the NIH (RO1 CA 74322). We would like to thank Sally Carson for her hard work, support, and assistance with this project.
REFERENCES
- 1.Kaiser Family Foundation and Health Research and Educational Trust. Employer health benefits: 2004 summary of findings. [January 22, 2005]; Available at http://www.kff.org/insurance/7148/sections/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=46224.
- 2.Frist WH. Health care in the 21st century. N Engl J Med. 2005;352:267–72. doi: 10.1056/NEJMsa045011. [DOI] [PubMed] [Google Scholar]
- 3.Doherty RB. Assessing the new medicare prescription drug law. [August 17, 2004];Ann Intern Med. 2004 141(5) doi: 10.7326/0003-4819-141-5-200409070-00100. Available at http://www.annals.org/ [DOI] [PubMed] [Google Scholar]
- 4.Hoadley J. The Effects of Formularies and Other Cost Management Tools on Access to Medications: An Analysis of the MMA and the Final Rule. Kaiser Family Foundation Report. [April 17, 2005]; Available at http://www.kff.org/medicare/loader.cfm?url=/commonspot/security/getfile.cfm&PageID=51878.
- 5.Trude S, Grossman JM. Patient cost-sharing innovations: promises and pitfalls. Issue Brief No. 75, Center for the Study of Health Systems Change. [May 6, 2004]; Available at http://www.hschange.com/CONTENT/643/ [PubMed]
- 6.Shrank WH, Young H, Ettner SL, Glassman P, Asch SM, Kravitz R. Do the incentives in three-tier, incentive-based pharmaceutical benefit plans operate as intended? Results from a physician leadership survey. Am J Manage Care. 2005;11:16–22. [PubMed] [Google Scholar]
- 7.Alexander GC, Casalino LP, Meltzer DO. Physician strategies to reduce patients' out-of-pocket prescription costs. Arch Intern Med. 2005;165:633–6. doi: 10.1001/archinte.165.6.633. [DOI] [PubMed] [Google Scholar]
- 8.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA. 2003;290:953–8. doi: 10.1001/jama.290.7.953. [DOI] [PubMed] [Google Scholar]
- 9.Medical Expenditure Panel Survey Highlights. Distribution of Healthcare Expenses, 1996. Publication 00-0024. Rockville, MD: AHRQ; 2000. [Google Scholar]
- 10.Mooney C, Duval R. Bootstrapping: a nonparametric approach to statistical inference. In: Lewis-Beck M, editor. Quantitative Applications in Social Science. Vol. 95. Newbury Park, CA: Sage University Press; 1993. [Google Scholar]
- 11.Physician Characteristics and Distribution in the US, American Medical Association, 2003–2004 Edition. Hyattsville, MD: National Center for Health Statistics; 2004. [Google Scholar]
- 12.Huskamp HA, Deverka PA, Epstein AM, Epstein RS, McGuigan KA, Frank RG. The effect of incentive-based formularies on prescription-drug utilization and spending. N Engl J Med. 2003;349:2224–32. doi: 10.1056/NEJMsa030954. [DOI] [PubMed] [Google Scholar]
- 13.Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291:2344–50. doi: 10.1001/jama.291.19.2344. [DOI] [PubMed] [Google Scholar]
- 14.Hillman AL, Pauly MV, Escarce JJ, et al. Financial incentives and drug spending in managed care. Health Affairs. 1999:189–200. doi: 10.1377/hlthaff.18.2.189. [DOI] [PubMed] [Google Scholar]
- 15.Stuart B, Zacker C. Who bears the burden of Medicaid drug copayment policies. Health Affairs. 1999;18:201–12. doi: 10.1377/hlthaff.18.2.201. [DOI] [PubMed] [Google Scholar]
- 16.Smith DG. The effects of copayments and generic substitution on the use and costs of prescription drugs. Inquiry. 1993;30:189–98. [PubMed] [Google Scholar]
- 17.Reeder CE, Nelson AA. The differential impact of copayment on drug use in a Medicaid population. Inquiry. 1985;22:396–403. [PubMed] [Google Scholar]
- 18.Harris BL, Stergachis A, Reid A. The effect of drug copayments on utilization and cost of pharmaceuticals in a health maintenance organization. Medical Care. 1990;28:907–17. doi: 10.1097/00005650-199010000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285:421–9. doi: 10.1001/jama.285.4.421. [DOI] [PubMed] [Google Scholar]
- 20.Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004;42:626–34. doi: 10.1097/01.mlr.0000129352.36733.cc. [DOI] [PubMed] [Google Scholar]
- 21.Glassman PA, Tanielian T, Harris K, et al. Provider perceptions of pharmacy management: lessons from the military health system. Med Care. 2004;42:361–6. doi: 10.1097/01.mlr.0000118862.92043.9b. [DOI] [PubMed] [Google Scholar]
- 22.Hsu J, Reed M, Brand R, Fireman B, Newhouse JP, Selby JV. Cost-sharing:patient knowledge and effects on seeking emergency department care. Med Care. 2004;42:290–6. doi: 10.1097/01.mlr.0000114917.50457.52. [DOI] [PubMed] [Google Scholar]
- 23.Shrank WH, Hoang T, Ettner SL, et al. The implications of choice: prescribing generic or preferred formulary medications improves adherence to chronic medications. Arch Intern Med. 2006;166:322–7. doi: 10.1001/archinte.166.3.332. [DOI] [PubMed] [Google Scholar]