Abstract
BACKGROUND
The use of chronic opioids for noncancer pain is an increasingly common and difficult problem in primary care.
OBJECTIVE
To test the effects on physicians' self-reported attitudes and behavior of a shared decision-making training for opioid treatment of chronic pain.
DESIGN
Randomized-controlled trial.
PARTICIPANTS
Internal Medicine residents (n=38) and attendings (n=7) were randomized to receive two 1-hour training sessions on a shared decision-making model for opioid treatment for chronic pain (intervention, n=22) or written educational materials (control, n=23).
MEASUREMENTS
Questionnaires assessing physician satisfaction, physician patient-centeredness, opioid prescribing practices, and completion rates of patient treatment agreements administered 2 months before and 3 months after training.
RESULTS
At follow-up, the intervention group reported significantly greater overall physician satisfaction (P =.002), including subscales on relationship quality (P =.03) and appropriate use of time (P =.02), self-reported completion rates of patient treatment agreements (P =.01), self-reported rates of methadone prescribing (P =.05), and self-reported change in care of patients with chronic pain (P =.01).
CONCLUSIONS
Training primary care physicians in the shared decision-making model improves physician satisfaction in caring for patients with chronic pain and promotes the use of patient treatment agreements. Further research is necessary to determine whether this training improves patient satisfaction and outcomes.
Keywords: chronic pain, randomized trial, physician satisfaction, opioid contracts
Chronic, noncancer pain (hereafter, chronic pain) is an increasingly common and difficult clinical problem in primary care. Professional organizations have recommended increased use of opioids,1 which has occurred in recent years.2 Some pain specialists have interpreted the growth in opioid use as evidence of better pain treatment,3 but others believe that there have not been adequate trials to prove the “safety and effectiveness of long-term opioid therapy” for chronic pain.4
Shared decision making in medical encounters has been advocated in order to respect patient values and improve patient outcomes.5 We conducted a pilot study to test a 2 session primary care physician-training program focused on shared decision making with patients with chronic pain. The study had 3 primary aims: (1) to test the feasibility of teaching a shared decision-making model concerning opioid treatment of chronic pain in primary care, (2) to test whether shared decision making enhances physicians' sense of collaboration and satisfaction in treating these patients, and (3) to obtain preliminary physician self-report data on whether the shared decision-making model might improve the quality of care for patients with chronic pain.
METHODS
The study was conducted at the General Internal Medicine Clinic (GIMC), University of Washington Medical Center, Seattle, WA. Before the training, the protocol was reviewed by a focus group of 7 physicians. Twenty-six physicians were randomly assigned to the intervention group and 23 to the control group. Four intervention physicians were subsequently excluded because of their inability to participate in both training sessions. Our final pool consisted of 22 intervention and 23 control physicians. All physicians were assessed at 2 months preintervention and at 3 months postintervention.
Physician satisfaction was assessed with a modified version of the Physician Satisfaction Questionnaire,6 adapted to assess satisfaction with recent encounters with chronic pain patients. This 20-item scale contains 4 subscales: relationship quality, adequacy of data collection, appropriate use of time, and patient's cooperative nature. Physician patient centeredness was assessed with a 20-item measure7, which has been validated for use with primary care physicians. The scale contains 4 subscales: doctor receptiveness, patient involvement, affective content of the relationship, and information giving. Three additional measures were developed by the authors: (1) frequency of opioids prescribed and patient treatment agreement completion, (2) changes in prescription practices and attitudes concerning caring for patients with chronic pain, and (3) the overall usefulness and effectiveness of the shared decision-making training.
In November 2004, intervention and control physicians were given an educational packet on the use of chronic opioids that included the following (1) an opioid conversion table, (2) an educational resource list, (3) a review article on opioid therapy for chronic pain,8 and (4) GIMC policy on the use of opiates for chronic pain (including recommendations concerning patient care agreements, depression assessment, and methadone use but no strategies or guidance). Intervention physicians attended 2-hour long shared decision-making training sessions held at GIMC.
Each session utilized a videotape of an office visit where the “patient” presented with low back pain of 1 year's duration and requested continuation of Percocet prescribed by her previous physician. The first training was divided into three 5-minute video segments with the following learning objectives: (1) to introduce the shared decision-making model, including negotiation and documentation of shared treatment goals with the patient; (2) to negotiate nonmedication treatments; and (3) to negotiate the prescription of methadone (as the long-acting opioid least prone to abuse).
The second training hour followed the patient into her next visit when she asks for more pain medication because of worsening pain. The learning objectives were as follows: (1) to review goals established in her previous visit, (2) to screen for depression while exploring declining health status, and (3) to negotiate from the patient's initial request for more pain medication to a prescription for antidepressant medication. Hypothetical third visit scenarios were then presented for discussion, portraying improving, stable, or deteriorating health status. Learning objectives for the training are listed in Table S1.
To explore the training's generalizability, it was repeated for resident and attending physicians (n=20) at the Seattle Providence Family Medicine Program. Assessments were administered immediately before and after training. There was no control group or 3-month posttraining assessment for this sample.
Differences in demographics and questionnaire responses at baseline were assessed using 2-sided t-tests on mean scores. To assess for a treatment effect, we performed ANCOVA statistical analysis on posttraining assessments for intervention and control groups, controlling for gender, training rank, and baseline scores. Analyses were performed using SPSS v12.0 (Chicago, IL).
RESULTS
Intervention and control groups were balanced in terms of gender and rank. Physician satisfaction results are presented in Table 1. There were no significant differences at baseline between groups; however, at 3 months posttraining, significant differences were found on the overall satisfaction score (F=10.74, P <.01), and on 2 subscales: relationship quality (F=4.76, P <.05) and appropriate use of time (F=6.23, P <.05).
Table 1.
Physician Satisfaction
| M (SD) | ||
|---|---|---|
| 5-Point Likert Scale Ranging from 1 (Strongly Disagree) to 5 (Strongly Agree). Higher Number Represents Higher Satisfaction. | Intervention (n=22) | Control (n=23) |
| Scale mean at baseline | 2.93 (0.35) | 2.84 (0.35) |
| Scale mean postintervention | 3.20 (0.36) | 2.86 (0.32)* |
| Subscale 1 | ||
| Relationship quality baseline | 2.94 (0.55) | 2.87 (0.53) |
| Relationship quality 3 mo postintervention | 3.27 (0.46) | 2.97 (0.54)† |
| Subscale 2 | ||
| Adequacy of data collection/visit baseline | 2.55 (0.81) | 2.23 (0.70) |
| Adequacy of data collection/visit 3 mo postintervention | 2.80 (0.77) | 2.45 (0.62) |
| Subscale 3 | ||
| Appropriate use of time baseline | 3.65 (0.63) | 3.57 (0.61) |
| Appropriate use of time 3 mo postintervention | 3.92 (0.59) | 3.44 (0.79)† |
| Subscale 4 | ||
| Patient's nondemanding, cooperative nature baseline | 2.39 (0.57) | 2.29 (0.68) |
| Patient's nondemanding cooperative nature 3 mo postintervention | 2.53 (0.70) | 2.29 (0.76) |
P<.01.
P<.05.
The overall physician patient-centeredness score and 3 subscale scores (doctor receptiveness, patient involvement, and affective content of the relationship) were not significantly different between groups at 3 months postintervention. The fourth subscale (information giving) was significantly higher in the intervention group (F=4.88, P <.05), indicating a greater propensity to give patients more information to assist them in making decisions.
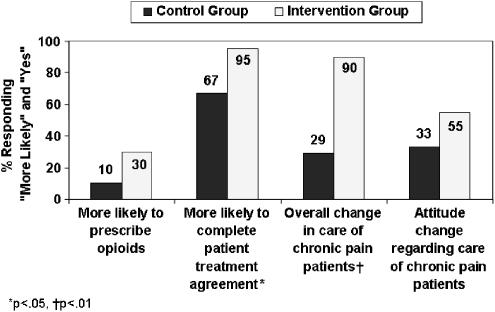
At 3 months postintervention, intervention physicians reported they were more likely to complete patient-care agreements and to report “making overall changes in their management of” and “attitude toward” chronic pain patients (see Fig. 1). At 3 months postintervention, physicians were more likely to prescribe methadone (F=4.42, P <.05) and more likely to set functional goals (F=11.65, P <.01).
FIGURE 1.
Self-reported changes in physician behavior and attitudes at 3 months posttraining.
Eighty-two percent of intervention physicians rated the training as useful at the end of the training, and 67% did so at a 3-month follow-up. After the training, 73% of physicians also reported feeling more competent to care for patients with chronic pain. Four of 22 intervention physicians attended a focus group after the 3 months posttraining assessments. Although self-selected, these 4 were typical of the intervention group in terms of pre-intervention assessment scores. They reported that the training was helpful in 3 specific areas: (1) in producing a less antagonistic relationship between the physician and chronic pain patient, (2) in promoting regular use of patient treatment agreements, and (3) in promoting a shift of focus from level of pain to patient function.
When the training was repeated for the Seattle Providence Family Medicine residents and faculty, the responses were similar: 89% described the training as “useful” or “very useful”; 50% reported feeling more competent; and 55% reported feeling more personally comfortable caring for chronic pain patients after the training sessions.
DISCUSSION
This pilot study demonstrates that 2 hours of training in a shared decision-making model for opioid treatment of chronic pain is feasible and results in improvement in self-reported physician attitudes and behaviors. After the training, physicians reported they were more likely to complete patient treatment agreements and to mutually set functional goals in these. Most intervention physicians reported feeling more competent, confident, and comfortable with chronic pain care after training, an important outcome given that such care is often considered difficult.9
Our pilot study has a number of important limitations. First, assessments were limited to self-reports of physician attitudes and behaviors. Second, this was a small sample of physicians at a single institution. We did partially replicate our findings at an additional site, but the generalizability of the intervention effects still needs to be shown. Third, 4 physicians randomized to the intervention were excluded from the study because scheduling precluded completion of both training and baseline assessment, but they were similar to the participants who were included. Fourth, the intervention group had more contact time with the investigators, a bias, that may have partially accounted for the observed effect.
Previous-randomized trials of training in shared decision making have had mixed results. Most report success at changing physician behaviors and attitudes, but fail to improve patient outcomes.10,11 A single trial of shared decision making in fibromyalgia showed improved patient receptiveness to a chronic pain treatment plan.12 Opioid contracts have been a common accompaniment to opioid prescription in the specialty pain management setting.13 They have been recently been adapted to include collaboration with the primary care physician.14 However, these contracts are generally used to put limits on patients, rather than to empower or collaborate with them. In a recent review, the goals of care were among the least common elements of pain contracts, found in only 38%.15 Truly collaborative treatment agreements focusing on negotiated goals for chronic pain care could be a powerful tool for increasing patient participation and satisfaction with care. This remains to be shown in a subsequent trial.
In summary, our trial demonstrates that it is feasible to train primary care physicians in a shared decision-making procedure concerning opioid use for chronic pain. Relevant self-reported physician attitudes and behaviors were significantly improved by this training. Further research is necessary to determine whether shared decision-making training can improve satisfaction and clinical outcomes for patients with chronic pain.
Acknowledgments
The research reported in this article was supported by a grant to Dr. Sullivan from the Greenwall Foundation (#1005928). The authors would like to thank Dr. Jennifer Gilkes for portraying the patient in the video sessions.
Supplementary Material
The following supplementary material is available for this article online at http://www.blackwell-synergy.com
Appendix A: Initial Patient Treatment Agreement Form.
Table S1. Summary Learning Objectives.
REFERENCES
- 1.The use of opioids for the treatment of chronic pain. A consensus statement from the American Academy of Pain Medicine and the American. Pain Society. Clin J Pain. 1997;13:6–8. [PubMed] [Google Scholar]
- 2.Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109:514–9. doi: 10.1016/j.pain.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Portenoy RK. Appropriate use of opioids for persistent non-cancer pain. Lancet. 2004;364:739–40. doi: 10.1016/S0140-6736(04)16951-1. [DOI] [PubMed] [Google Scholar]
- 4.Von Korff M, Deyo RA. Potent opioids for chronic musculoskeletal pain: Flying blind? Pain. 2004;109:207–9. doi: 10.1016/j.pain.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 5.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44:681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 6.Suchman AL, Roter D, Green M, Lipkin M., Jr. Physician satisfaction with primary care office visits. Collaborative Study Group of the American Academy on Physician and Patient. Med Care. 1993;31:1083–92. doi: 10.1097/00005650-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Ogden J, Ambrose L, Khadra A, et al. A questionnaire study of GPs' and patients' beliefs about the different components of patient centredness. Patient Educ Couns. 2002;47:223–7. doi: 10.1016/s0738-3991(01)00200-2. [DOI] [PubMed] [Google Scholar]
- 8.Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;349:1943–53. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- 9.Wasan AD, Wootton J, Jamison RN. Dealing with difficult patients in your pain practice. Reg Anesth Pain Med. 2005;30:184–92. doi: 10.1016/j.rapm.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Edwards A, Elwyn G, Hood K, et al. Patient-based outcome results from a cluster randomized trial of shared decision-making skill development and use of risk communication aids in general practice. Fam Pract. 2004;21:347–54. doi: 10.1093/fampra/cmh402. [DOI] [PubMed] [Google Scholar]
- 11.Brown JB, Boles M, Mullooly JP, Levinson W. Effect of clinician communication skills training on patient satisfaction. A randomized, controlled trial. Ann Intern Med. 1999;131:822–9. doi: 10.7326/0003-4819-131-11-199912070-00004. [DOI] [PubMed] [Google Scholar]
- 12.Bieber C, Muller KG, Blumenstiel K, et al. Shared decision making (SDM) with chronic pain patients. The patient as a partner in the medical decision making process. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2004;47:985–91. doi: 10.1007/s00103-004-0914-4. [DOI] [PubMed] [Google Scholar]
- 13.Kirkpatrick AF, Derasari M, Kovacs PL, Lamb BD, Miller R, Reading A. A protocol-contract for opioid use in patients with chronic pain not due to malignancy. J Clin Anesth. 1998;10:435–43. doi: 10.1016/s0952-8180(98)00062-2. [DOI] [PubMed] [Google Scholar]
- 14.Fishman SM, Mahajan G, Jung SW, Wilsey BL. The trilateral opioid contract. Bridging the pain clinic and the primary care physician through the opioid contract. J Pain Symptom Manage. 2002;24:335–44. doi: 10.1016/s0885-3924(02)00486-4. [DOI] [PubMed] [Google Scholar]
- 15.Fishman SM, Bandman TB, Edwards A, Borsook D. The opioid contract in the management of chronic pain. J Pain Symptom Manage. 1999;18:27–37. doi: 10.1016/s0885-3924(99)00035-4. [DOI] [PubMed] [Google Scholar]