Abstract
BACKGROUND
Entry into general internal medicine (GIM) has declined. The effect of the inpatient general medicine rotation on medical student career choices is uncertain.
OBJECTIVE
To assess the effect of student satisfaction with the inpatient general medicine rotation on pursuit of a career in GIM.
DESIGN
Multicenter cohort study.
PARTICIPANTS
Third-year medical students between July 2001 and June 2003.
MEASUREMENTS
End-of-internal medicine clerkship survey assessed satisfaction with the rotation using a 5-point Likert scale. Pursuit of a career in GIM defined as: (1) response of “Very Likely” or “Certain” to the question “How likely are you to pursue a career in GIM?”; and (2) entry into an internal medicine residency using institutional match data.
RESULTS
Four hundred and two of 751 (54%) students responded. Of the student respondents, 307 (75%) matched in the 2 years following their rotations. Twenty-eight percent (87) of those that matched chose an internal medicine residency. Of these, 8% (25/307) were pursuing a career in GIM. Adjusting for site and preclerkship interest, overall satisfaction with the rotation predicted pursuit of a career in GIM (odds ratio [OR] 3.91, P<.001). Although satisfaction with individual items did not predict pursuit of a generalist career, factor analysis revealed 3 components of satisfaction (attending, resident, and teaching). Adjusting for preclerkship interest, 2 factors (attending and teaching) were associated with student pursuit of a career in GIM (P<.01).
CONCLUSIONS
Increased satisfaction with the inpatient general medicine rotation promotes pursuit of a career in GIM.
Keywords: medical student, career interest, general internal medicine
Although the most recent data show no change in the number of medical students choosing and entering categorical internal medicine residencies, student interest in general internal medicine (GIM) has been declining over most of the past decade.1,2 This declining interest is evident in the results of the Medical Student Graduation Questionnaire administered by the Association for American Medical Colleges which demonstrate a decrease in the percentage of students intending to enter a career in GIM between 1999 and 2003 (from 12.1% to 5.2%), with a corresponding increase in the number of students intending to enter a specialty of internal medicine.3
To assure an adequate supply of future General Internists, factors associated with medical student interest in this career path require attention.4 A desire for a controllable lifestyle, the rising cost of medical education, and physician dissatisfaction because of poor reimbursement and practice hassles are all potential causes of this declining student interest.5–13 This waning interest also may relate, in part, to the experience of medical students during their medicine rotations. Although studies suggest that ambulatory experiences or exposure to generalist preceptors during the third year are associated with improved perception of and increased entry into generalist careers, many of these studies took place over a decade ago, when initiatives deisgned to promote primary care were implemented and the economic environment for medicine was different.14–19 In many academic teaching hospitals, though medical student exposure to GIM is primarily through the inpatient general medicine rotation, the effect of this rotation on a student's intention to pursue a career in GIM is not known. While internal medicine clerkships are consistently highly rated by graduating medical students, their impact on student interest in pursuing a career in GIM is debatable.20 Indeed, the president of the Association of American Medical Colleges has suggested that the third-year inpatient experience in internal medicine has a negative impact on medical student interest in a GIM career because of the complex nature of medical inpatients and the frequent absence of well-functioning systems in academic teaching hospitals.21
One important challenge to studying student entry into a career in GIM is defining an appropriate outcome variable. Earlier studies often used the outcome, “number of students choosing a generalist specialty,” defined as exclusively family medicine or the composite outcome of family medicine, pediatrics, or internal medicine.22 Entry into an internal medicine residency alone may not accurately reflect student entry into a career as a General Internist given the increasing majority of internal medicine trainees choosing subspecialty fellowship training or hospitalist careers.23 An ideal study would follow third-year students for at least 5 years until the end of their internal medicine residency, to determine if residents ultimately choose careers as General Internists, hospitalists, or subspecialists. In the absence of this ideal study, a potential short-term measure we can use to reflect student pursuit of a GIM career may be obtained by using students' stated likelihood of entering a career in GIM, coupled with matching into an internal medicine residency. In this multicenter study, we used this measure to assess the effect of student satisfaction with the inpatient general medicine rotation and aspects of the rotation (teaching, attending and resident characteristics, and patient care) on student pursuit of a career in GIM.
METHODS
The data used for this study were collected for the Multicenter Trial of Academic Hospitalists, a quasi-randomized study of the effect of hospitalists as attendings on patient outcomes on general medicine services at 6 academic medical centers (Brigham and Women's Hospital, University of Chicago, University of California, San Francisco, University of Iowa, University of New Mexico, and University of Wisconsin) between July 2001 and June 2003. All sites are large academic medical centers that have prominent academic sections or divisions of GIM. Third-year medical students were asked to complete a questionnaire upon completion of their general medicine rotation. Students were required to rotate on an inpatient general medicine rotation for an average of 4 weeks, with no student doing less than 2 weeks. Inpatient general medicine services were staffed by an attending physician who was a General Internist, a subspecialist, or a hospitalist. The Institutional Review Board at all sites approved this study.
QUESTIONNAIRE DESIGN
Medical students were administered a 22-item end-of-clerkship questionnaire that assessed overall satisfaction and satisfaction with specific aspects of the rotation in 3 domains: (1) teaching; (2) characteristics of attending and resident; and (3) patient care. Overall satisfaction and satisfaction with specific aspects of the rotation were measured on a 5-point Likert scale from 1 (Very Dissatisfied) to 5 (Very Satisfied). Questions regarding patient volume and supervision of clinical work were measured on a 5-point scale, ranging from 1 (Far too Little) to 5 (Far too Much), with a score of 3 corresponding to “Just Right.” These surveys have been used at one of the sites in prior studies of the effect of a hospitalist service on teaching and satisfaction.24,25 The response to the question, “Upon completion of this clerkship, how likely are you to pursue a career in GIM?” was measured on a 5-point scale with the following possible responses: (1) Not At All Likely; (2) Not Very Likely; (3) Somewhat Likely; (4) Very Likely; and (5) Certain. Using this same response set, the following question was asked to gauge student's preclerkship interest in pursuing a career in GIM: “Before this clerkship began, how likely were you to pursue a career in GIM?”
MATCH DATA
Entry into an internal medicine residency was determined by using institutional match data from the 2 years after completion of the students' clerkships. Those students that matched into categorical internal medicine, primary care internal medicine, or medicine pediatrics residency programs were labeled as students that entered an internal medicine residency.
DATA ANALYSIS
Descriptive statistics were used to summarize overall satisfaction, satisfaction with specific aspects of the rotation, preclerkship interest in a career in GIM, intention to pursue a career in GIM, and entry into an internal medicine residency. Student pursuit of a career in GIM was defined as: (1) a stated likelihood of 4 (Very Likely) or 5 (Certain) of pursuing a career in GIM after the rotation and (2) matching into an internal medicine residency. Because it is likely that students interpreted “GIM” to include hospitalist as well as outpatient generalist careers, an additional question was asked regarding whether students' envisioned a mostly inpatient career, mostly outpatient career or were uncertain. Those students with a high stated likelihood of pursuing a career in GIM, and who envisioned a mostly inpatient career were excluded because of presumed interest in a hospitalist career. Those students that were uncertain were also excluded. Multivariable logistic regression was performed, controlling for site and initial interest in career in GIM, to determine the effect of overall satisfaction on student pursuit of a career in GIM. These analyses were repeated to determine the effect of satisfaction with specific rotation elements on student pursuit of a career in GIM. We then used multivariable ordinal logistic regression, adjusting for site and initial interest in a career in GIM, to assess the effect of satisfaction with specific rotation elements on increased overall satisfaction with the rotation. Because survey items were highly correlated, factor analysis was performed to extract principal components of overall satisfaction based on responses to survey items.26 Factor analysis is a statistical procedure to allow analysis of highly correlated items by extracting independent factors that may be responsible for variability across them, By definition, factors are uncorrelated and can be used in regression analyses without concern of collinearity. Each factor has an eigenvalue which measures the amount of variation in the total sample accounted for by each factor. Those factors with an eigenvalue >1 were retained. These factors were extracted through iterated principal factor extraction, along with varimax rotation to simplify the interpretation of the factors. Survey items were scored based on their relationship to each factor to identify the factor. Similar to a prior study of medical students, the factors were then used to predict our outcome of interest, student pursuit of a career in GIM.27 All statistical tests were performed using Intercooled Stata 8.0 (Stata Corp., College Station, TX), with statistical significance defined as P<.05.
RESULTS
Of the 751 third-year medical students that rotated on general medicine services, 402 (54%) completed our survey. Response rates per site were: site 1 (107/173; 62%); site 2 (46/123; 37%); site 3 (58/156; 37%); site 4 (55/78; 71%); site 5 (81/116; 70%); and site 6 (55/105; 52%). The majority of students (354/397; 89%) were either Satisfied (4) or Very Satisfied (5) with their general medicine rotation, with a mean rating of 4.34 (Table 1). Students were particularly satisfied with certain attending or resident characteristics (e.g., availability, relationship, clinical excellence, and emphasis on education), with an average rating above 4.2. Items relating to other rotation aspects, such as teaching about clinical topics and emphasis on evidence-based medicine, all scored above 4. However, there were certain aspects of the rotation with which students were less satisfied, namely teaching about basic science topics, cost-effectiveness, and managed care.
Table 1.
Student Satisfaction with the Inpatient General Medicine Rotation: Overall and with Specific Elements
| Question (n = 402) | Mean | Standard Deviations |
|---|---|---|
| Overall, how satisfied were you with your experience on the general medicine service this month?* | 4.34 | 0.86 |
| How satisfied are you with the following aspects of your work on the medical wards this month?* | ||
| Teaching | ||
| Teaching about clinical topics | 4.19 | 0.85 |
| Emphasis on evidence-based medicine | 4.10 | 0.92 |
| Presence of structured curriculum | 3.86 | 0.95 |
| Teaching about basic science topics | 3.44 | 0.95 |
| Teaching about cost-effectiveness | 3.22 | 1.01 |
| Teaching about managed care | 2.79 | 0.99 |
| Attending characteristics | ||
| Quality of attending rounds | 4.23 | 0.83 |
| Clinical excellence | 4.53 | 0.74 |
| Availability | 4.34 | 0.88 |
| Relationship | 4.32 | 0.90 |
| Emphasis on education | 4.26 | 0.92 |
| Provision of timely feedback | 4.05 | 1.04 |
| Resident characteristics | ||
| Clinical excellence | 4.55 | 0.70 |
| Availability | 4.60 | 0.71 |
| Relationship | 4.59 | 0.74 |
| Emphasis on education | 4.22 | 0.94 |
| Provision of timely feedback | 4.16 | 0.95 |
| Patient care | ||
| Patient volume† | 2.97 | 0.49 |
| Supervision of your clinical work† | 2.82 | 0.60 |
Likert scale responses ranged from 1 (Very Dissatisfied) to 5 (Very Satisfied)
Likert scale responses ranged from 1 (Too Little) to 5 (Too Much)
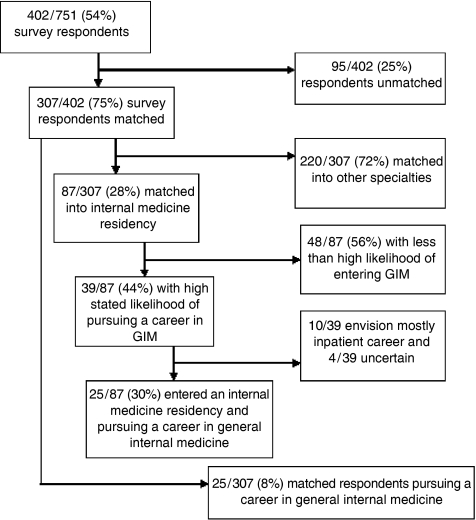
Three hundred and seven (75%) of survey respondents matched into a residency program in the 2 years after their third-year internal medicine clerkship (Fig. 1). Of these, 87 (28%) chose to enter an internal medicine residency. This is higher than the reported 19% of students choosing internal medicine residencies of those that successfully match in the National Residency Matching Program for the years of this study.28 Rates of matching into an internal medicine residency varied by site between 21% and 31%, and these differences were not significantly different. Of those students that matched into an internal medicine residency, 39/87 (44%) state a high likelihood of pursuing a career in general intenral medicine. Ten of these 39 students responded that they also envisioned a career that was mostly inpatient and an additional 4 were uncertain. After excluding these students, 25/87 (30%) of those students that matched into an internal medicine residency, or 25/307 (8%) of students that matched overall, met criteria for the outcome of interest, students pursuing a career in GIM.
Figure 1.
*High stated likelihood of pursuing a career in general internal medicine (GIM) is defined as a response of 4 (Very Likely) or 5 (Certain) to the question, “Upon Completion of this clerkship,how likely are you to pursue a career in GIM?”
†Envisioning a predominantly inpatient career is defined as a response of 1 (mostly inpatient) or 2 (somewhat more inpatient) to the question, “If you do choose a career in GIM, what balance of inpatient and outpatient do you envision for yourself?”
In multivariable analysis, controlling for preclerkship interest and site, overall satisfaction with the rotation was directly related to student pursuit of a GIM career (Table 2). For every 1 point increase in overall satisfaction on the 5-point scale, students were almost 4 times more likely to intend to pursue a career in GIM (odds ratio [OR] 3.91, P<.001). Of note, 2 of the sites did not have any students that were pursuing a career in GIM.
Table 2.
Predictors of Pursuit of a Career in General Internal Medicine*
| Predictor† (n = 297) | Odds Ratio | 95% Confidence Interval | P value |
|---|---|---|---|
| Overall satisfaction | 3.91 | 1.52 to 10.07 | .01 |
| Preclerkship interest‡ | |||
| Not at all likely (1) | 0.24 | 0.03 to 1.99 | .19 |
| Not very likely (2) | 0.15 | 0.03 to 0.71 | .02 |
| Very likely (4) | 0.72 | 0.24 to 2.09 | .54 |
| Certain (5) | 5.51 | 1.12 to 27.09 | .04 |
| Site | |||
| Site 2 | 0.68 | 0.13 to 3.59 | .65 |
| Site 4 | 1.23 | 0.30 to 4.98 | .77 |
| Site 5 | 0.87 | 0.29 to 2.56 | .79 |
We defined a student as pursuing a career in general internal medicine if they met all of the following 3 criteria: (1) a high stated likelihood of pursuing a career in general internal medicine (a response of 4 (Very Likely) or 5 (Certain) to the question, “Having completed this clerkship, how likely do you feel you are to pursue a career in general internal medicine?”); (2) matched into an internal medicine residency; and (3) did not envision a predominantly inpatient practice setting
These are the results of a multivariable logistic regression model, controlling for level of preclerkship interest and site, to test the effect of overall satisfaction, ranging from 1 to 5 on pursuit of a career in general internal medicine. Those students who had a preclerkship interest of “Somewhat Likely” served as the reference group. Because sites 3 and 6 included no students in pursuit of a career in general internal medicine, they were combined with site 1 to form the reference group
Preclerkship interest is defined as response to the following question, “Before this clerkship began, how likely did you feel you are to pursue a career in general internal medicine?” The reference group is those students who responded “Somewhat Likely” (3)
Student satisfaction with specific elements of the rotation predicted increased overall rotation satisfaction (Table 3). These elements included attending and residents characteristics such as better relationships with attending and resident and quality of attending rounds; and elements related to teaching, such as teaching about clinical topics, and the presence of a structured curriculum.
Table 3.
Elements of Inpatient Rotation that Predict Increased Overall Satisfaction*
| Predictor (n = 402) | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Teaching | 1.44 | 1.04 to 2.00 | .03 |
| Presence of structured curriculum | |||
| Clinical topics | 1.72 | 1.12 to 2.65 | .01 |
| Attending characteristics | |||
| Quality of attending rounds | 1.91 | 1.25 to 2.94 | .01 |
| Relationship | 1.81 | 1.17 to 2.82 | .01 |
| Resident characteristics | |||
| Relationship | 1.96 | 1.17 to 3.27 | .01 |
| Provision of timely feedback | 1.72 | 1.22 to 2.44 | .01 |
| Patient care | |||
| High volume | 0.40 | 0.17 to 0.95 | .04 |
| Site‡ | |||
| Site 2 | 2.82 | 1.05 to 7.57 | .04 |
Results are for a multivariate ordinal logistic regression model using satisfaction with rotation elements listed in Table 1 to predict odds of increased overall satisfaction, measured on a 5-point Likert scale from 1 (Not at All Satisfied) to 5 (Very Satisfied). Only those items that were statistically significant predictors of overall satisfaction are included in the table
Results are adjusted for pre-clerkship interest and site (reference groups include those students that responded “Somewhat Likely” (3) and those students from site 1, respectively).
Satisfaction with specific rotation elements did not predict student pursuit of a career in GIM. Factor analysis of rotation elements confirmed the existence of 3 factors corresponding to attending characteristics, resident characteristics, and teaching. The total variance explained by the 3 factors is 70%. Survey items that corresponded to these factors are grouped accordingly in Table 1. In multivariable logistic regression, 2 of these factors (attending characteristics and teaching) were significant predictors of student pursuit of a career in GIM (attending OR 2.15, P<.017; teaching OR 2.16, P<.002).
DISCUSSION
Our study shows that third year medical students are generally satisfied with the inpatient general medicine rotation. Satisfaction with the GIM rotation was an important independent predictor of student pursuit of a career in GIM. Overall satisfaction could be attributed to 3 distinct factors: satisfaction with the attending, resident, or teaching. Two of these, attending characteristics and teaching, were also significant predictors of pursuit of a career in GIM.
Given the projected shortage of generalist physicians, it is especially important to target efforts to improve interest and entry of medical students into GIM. While it has been acknowledged that the medicine clerkship is not likely the primary driver of career choice, our data suggest that its contribution is important.29 Specifically, improvements in overall satisfaction with the rotation may result in increased entry into GIM independent of a student's initial interest in a generalist career. Although student satisfaction with the internal medicine clerkship is high, our data suggest that if all students were “Very Satisfied” with the rotation, the number of students pursuing a career in GIM would increase by nearly 50%, a notable contribution to increasing the size of the future generalist workforce.
In considering specific interventions to improve overall satisfaction on the general medicine rotation, this study suggests the importance of relationship building with the attending and resident.30,31 This may be facilitated through optimization of medical student interaction with the attending and resident during the rotation period by minimizing team switches. Departments of medicine and GIM should consider selecting attendings with the high teaching evaluations to rotate on inpatient teaching services and protect attending time to ensure adequate teaching and relationship building time. Faculty development in teaching skills may also help. In addition, augmenting current teaching efforts through a structured curriculum focused on clinical topics may also improve overall satisfaction with the rotation. Students' feedback about teaching, quality of rounds, and patient volume should be solicited early in the rotation to set and exceed expectations to improve student satisfaction.
This study also attempts to build on earlier studies by using a novel outcome measure that incorporates both entry into an internal medicine residency and a high stated likelihood of pursuing a career in GIM. Although the validity and reliability of this outcome measure is still unknown, our results are consistent with national trends that demonstrate approximately one-third of internal medicine residents do not pursue subspecialty training.32 Nevertheless, 1 reason for caution in interpretation of these results is that the students' stated likelihood of pursuing a career in GIM after the rotation was much higher than expected. It is likely that students interpreted the definition of GIM to refer to a wide range of careers in internal medicine, including internal medicine subspecialty practice or hospitalist practice. Confusion regarding the meaning of the term “GIM” with the advent of hospital medicine raises important implications for future work and recruitment to the field. First, a measure to assess student intention to enter a career in GIM may need to include a more specific definition of GIM or include further qualifying questions, such as interest in subspecialty medicine used in prior studies.33 Second, students may only be considering the proximate choice they face, the choice of a general residency program. In answering this question, they may be expressing their intention to pursue a residency in internal medicine, but remain relatively undifferentiated regarding careers within internal medicine. For example, changing the definition of pursuit of a career in GIM to include those students that envisioned inpatient careers or were uncertain does not change our results. Lastly, third-year students may be interested in pursuing a career in GIM which diminishes by the end of their internal medicine residency.
There were several limitations of this study. First, although not atypical for surveys of medical students, our 54% average response rate and varying response rate by site may have caused sampling bias.34–36 This could be partly responsible for the statistically significant site differences observed in overall satisfaction at site 2 compared with the reference site. This could also partly explain why 2 sites did not have any students actively pursuing a career in GIM. However, because our results are adjusted by site, differences in response rates and interest in GIM alone cannot explain the findings. In addition, after adjusting for site, nonresponders did not differ in their rates of matching into residency programs or in the rate of matching into an internal medicine residency from responders. Second, we did not have statistical power in stratified analyses to examine the effect of satisfaction with the rotation and its elements on student pursuit of a career in GIM. For example, the 35% of students who were “Somewhat Likely” to pursue a career in GIM before the rotation began represent a group that might be particularly valuable to understand and target for intervention if there was adequate statistical power to draw conclusions within that subgroup. Third, we assessed preclerkship interest through retrospective report on the end-of-clerkship survey, raising the issue of the validity of these responses. For example, students' satisfaction with the rotation may have biased their rating of preclerkship interest. However, in simple χ2 analyses and in site-adjusted ordinal logistic regression models, level of preclerkship interest and overall satisfaction did not appear to be significantly associated. In additional analyses, removing preclerkship interest from our models did not change our results. Lastly, we did not assess the effect of specialty of the attending physicians (e.g., hospitalist, subspecialist, generalist) and resident career interest on students interest in GIM.
In conclusion, increased satisfaction with the inpatient general medicine rotation promotes student pursuit of a career in GIM. The inpatient general medicine rotation may be an important target for efforts to increase entry into the field.
Acknowledgments
This study was supported by the Agency for Healthcare Research and Quality grant R01 10597-A Multicenter Trial of Academic Hospitalists. We are grateful to Ms. Jennifer Higa, Mr. Micah Prochaska, Ms. Veronica Tirado, and Drs. David Gonzales, Anupama Gupta, and Rajiv Swamy for their research assistance.
REFERENCES
- 1.Biola H, Green LA, Phillips RL, Guirguis-Blake J, Fryer GE. The U.S. primary care physician workforce: persistently declining interest in primary care medical specialties. Am Fam Physician. 2003;68:1484. [PubMed] [Google Scholar]
- 2.Newton DA, Grayson MS. Trends in career choice by US medical school graduates. JAMA. 2003;290:1179–1182. doi: 10.1001/jama.290.9.1179. [DOI] [PubMed] [Google Scholar]
- 3.Medical School Graduation Questionnaire. Washington, DC: Association of American Medical Colleges; 1978–2004. [Google Scholar]
- 4.Whitcomb ME, Cohen JJ. The future of primary care medicine. N Engl J Med. 2004;351:710–2. doi: 10.1056/NEJMsb045003. [DOI] [PubMed] [Google Scholar]
- 5.Lee BY, Hecht T, Volpp K. Lifestyle as a factor in medical students' career choices. JAMA. 2003;290:2941. doi: 10.1001/jama.290.22.2941-a. [DOI] [PubMed] [Google Scholar]
- 6.Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003;290:1173–8. doi: 10.1001/jama.290.9.1173. [DOI] [PubMed] [Google Scholar]
- 7.Landon BE, Reschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians, 1997–2001. JAMA. 2003;289:442–9. doi: 10.1001/jama.289.4.442. [DOI] [PubMed] [Google Scholar]
- 8.Kravitz RL, Greenfield S, Rogers W, et al. Differences in the mix of patients among medical specialties and systems of care: results from the medical outcomes study. JAMA. 1992;267:1617–23. [PubMed] [Google Scholar]
- 9.Stoddard JJ, Hargraves JL, Reed M, Vratil A. Managed care, professional autonomy, and income. J Gen Intern Med. 2001;16:675–84. doi: 10.1111/j.1525-1497.2001.01206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zuger A. Dissatisfaction with medical practice. N Engl J Med. 2004;350:69–75. doi: 10.1056/NEJMsr031703. [DOI] [PubMed] [Google Scholar]
- 11.Colquitt WL, Zeh MC, Killian CD, Cultice JM. Effect of debt on U.S. medical school graduates' preferences for family medicine, general internal medicine, and general pediatrics. Acad Med. 1996;71:399–411. doi: 10.1097/00001888-199604000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Berg D, Cerletty J, Byrd JC. The impact of educational loan burden on housestaff career decisions. J Gen Intern Med. 1993;8:143–5. doi: 10.1007/BF02599760. [DOI] [PubMed] [Google Scholar]
- 13.Wetterneck TB, Linzer M, McMurray JE, et al. Worklife and satisfaction of general internists. Arch Intern Med. 2002;162:649–56. doi: 10.1001/archinte.162.6.649. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz MD, Linzer M, Babbott D, Divine GW, Broadhead WE. The impact of an ambulatory rotation on medical student interest in internal medicine. The society of general internal medicine task force on career choice in internal medicine. J Gen Intern Med. 1995;10:542–9. doi: 10.1007/BF02640362. [DOI] [PubMed] [Google Scholar]
- 15.Bauer RL, Venkatachalam HM, Forrester RH, Harris GD, Diehl AK. The effect of an ambulatory internal medicine rotation on students' career choices. Acad Med. 1997;72:147–9. doi: 10.1097/00001888-199702000-00024. [DOI] [PubMed] [Google Scholar]
- 16.Rucker L, Morgan C, Ward KE, Bell BM. Impact of an ambulatory care clerkship on the attitudes of students from five classes (1985–1989) toward primary care. Acad Med. 1991;66:620–2. doi: 10.1097/00001888-199110000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Davidson RA, Schwartz MD, Harris JO. Effect of a simple ambulatory experience on career choice and attitudes of medical students. Am J Med Sci. 1994;307:36–39. doi: 10.1097/00000441-199401000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Henderson MC, Hunt DK, Williams JW., Jr General internists influence students to choose primary care careers: the power of role modeling. Am J Med. 1996;101:648–53. doi: 10.1016/S0002-9343(96)00334-8. [DOI] [PubMed] [Google Scholar]
- 19.Hauer KE, Alper EJ, Clayton CP, et al. Educational responses to declining student interest in internal medicine careers. Am J Med. 2005;118:1164–70. doi: 10.1016/j.amjmed.2005.03.050. [DOI] [PubMed] [Google Scholar]
- 20.Kassebaum DG, Szenas PL, Schuchert MK. Determinants of the generalist career intentions of 1995 graduating medical students. Acad Med. 1996;71:198–209. doi: 10.1097/00001888-199602000-00030. [DOI] [PubMed] [Google Scholar]
- 21.Whitcomb ME, Cohen JJ. The future of primary care medicine. N Engl J Med. 2004;351:710–2. doi: 10.1056/NEJMsb045003. [DOI] [PubMed] [Google Scholar]
- 22.Hauer KE, Alper EJ, Clayton CP, et al. Educational responses to declining student interest in internal medicine careers. Am J Med. 2005;118:1164–70. doi: 10.1016/j.amjmed.2005.03.050. [DOI] [PubMed] [Google Scholar]
- 23.Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80:507–12. doi: 10.1097/00001888-200505000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998;279:1560–65. doi: 10.1001/jama.279.19.1560. [DOI] [PubMed] [Google Scholar]
- 25.Wachter RM, Goldman L. Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience. Am J Med. 1999;106:127–33. doi: 10.1016/s0002-9343(99)00012-1. [DOI] [PubMed] [Google Scholar]
- 26.Conway J, Huffcutt A. A review and evaluation of exploratory factor analysis practices in organizational research. Organizational Res Methods. 2003;6:147–68. [Google Scholar]
- 27.Schwartz MD, Linzer M, Babbott D, Divine GW, Broadhead E. Medical student interest in internal medicine. Initial report of the Society of General Internal Medicine Interest Group Survey on factors influencing career choice in internal medicine. Ann Int Med. 1991;114:6–15. doi: 10.7326/0003-4819-114-1-6. [DOI] [PubMed] [Google Scholar]
- 28.National Resident Match Program. Home page [Internet]. Available at http://www.nrmp.org/ Cited November 2, 2005.
- 29.Hauer KE, Alper EJ, Clayton CP, et al. Educational responses to declining student interest in internal medicine careers. Am J Med. 2005;118:1164–70. doi: 10.1016/j.amjmed.2005.03.050. [DOI] [PubMed] [Google Scholar]
- 30.Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12:53–6. doi: 10.1046/j.1525-1497.1997.12109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paice E, Heard S, Moss F. How important are role models in making good doctors? BMJ. 2002;325:707–10. doi: 10.1136/bmj.325.7366.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80:507–12. doi: 10.1097/00001888-200505000-00021. [DOI] [PubMed] [Google Scholar]
- 33.Schwartz MD, Linzer M, Babbott D, Divine GW, Broadhead WE. The impact of an ambulatory rotation on medical student interest in internal medicine. The Society of General Internal Medicine Task Force on Career Choice in Internal Medicine. J Gen Intern Med. 1995;10:542–9. doi: 10.1007/BF02640362. [DOI] [PubMed] [Google Scholar]
- 34.Robbins B, Ostrovsky DA, Melgar T. Factors in medical students' selection and ranking of combined medicine-pediatrics programs. Acad Med. 2005;80:199. doi: 10.1097/00001888-200502000-00020. [DOI] [PubMed] [Google Scholar]
- 35.Weyant RJ, Simon MS, Bennett ME. Changes in students' attitudes toward HIV-infected patients as the students progress through medical school. Acad Med. 1993;68:377–9. doi: 10.1097/00001888-199305000-00023. [DOI] [PubMed] [Google Scholar]
- 36.Agrawal JR, Huebner J, Hedgecock J, et al. Medical students' knowledge of the U.S. health care system and their preferences for curricular change: a national survey. Acad Med. 2005;80:484–8. doi: 10.1097/00001888-200505000-00017. [DOI] [PubMed] [Google Scholar]