Abstract
BACKGROUND
Learning environments overtly or implicitly address patient-centered values and have been the focus of research for more than 40 years, often in studies about the “hidden curriculum.” However, many of these studies occurred at single medical schools and used time-intensive ethnographic methods. This field of inquiry lacks survey methods and information about how learning environments differ across medical schools.
OBJECTIVE
To examine patient-centered characteristics of learning environments at 9 U.S. medical schools.
DESIGN
Cross-sectional internet-based survey.
PARTICIPANTS
Eight-hundred and twenty-three third- and fourth-year medical students in the classes of 2002 and 2003.
MEASUREMENTS
We measured the patient-centeredness of learning environments with the Communication, Curriculum, and Culture (C3) Instrument, a 29-item validated measure that characterizes the degree to which a medical school's environment fosters patient-centered care. The C3 Instrument contains 3 content areas (role modeling, students' experiences, and support for students' patient-centered behaviors), and is designed to measure these areas independent of respondents' attitudes about patient-centered care. We also collected demographic and attitudinal information from respondents.
RESULTS
The variability of C3 scores across schools in each of the 3 content areas of the instrument was striking and statistically significant (P values ranged from .001 to .004). In addition, the patterns of scores on the 3 content areas differed from school to school.
CONCLUSIONS
The 9 schools demonstrated unique and different learning environments both in terms of magnitude and patterns of characteristics. Further multiinstitutional study of hidden curricula is needed to further establish the degree of variability that exists, and to assist educators in making informed choices about how to intervene at their own schools.
Keywords: physician-patient relations; patient-centered care; schools, medical; students, medical; culture; organizational culture; education, medical, undergraduate; curriculum
Recent priorities in medical education have increasingly emphasized teaching skills and fostering attitudes related to patient-centered care.1–4 The Liaison Council for Medical Education, the Accreditation Council for Graduate Medical Education, the National Board of Medical Examiners, and various specialty certification boards have all taken steps in their spheres of influence to raise awareness about the importance of preparing medical students and trainees in several competencies related to patient-centered care.5–7 Examples of these competencies include patient-physician communication, fostering effective medical relationships, and practicing in a manner consistent with professional norms and values.
In addition, educators have developed a keen awareness that an institution's learning environment influences students' patient-centered attitudes and behaviors.8–10 A number of terms, including the “hidden curriculum,” the “informal curriculum,” and the “meta curriculum,” have been used to describe the implicit learning environment with respect to a variety of content areas, including patient-centered care.11–13 Studies of learning environments note inconsistencies between explicit norms that are taught during formal educational experiences such as coursework or clerkships, and implicit norms that are experienced by students during patient care.14,15 As students progress through medical school, such inconsistencies may result in an erosion of patient-centered behaviors and attitudes and an increase in cynicism.16–20 These changes may partially explain evidence showing that humanistic attitudes and ethical reasoning decline as the level of training increases.15,21–25
Medical school learning environments have been the focus of systematic study since the late 1950s.8,9,12,14,26–30 Most of these studies used sociological and anthropological methods to describe the diversity of covert messages transmitted through institutional culture. Examples of such messages include: “Good clinical care focuses on the biomedical over the psychosocial,”“It is undesirable to form emotional bonds with your patients,” and “Patient nonadherence reflects defects on the part of the patient, rather than physician misunderstanding or issues in the medical relationship.”14,31,32 While these studies have advanced our knowledge about general messages and processes inherent in the medical education milieu, there is a dearth of information about the diversity of learning environments across institutions. Do patient-centered learning environments share similar characteristics at all institutions, or are they uniquely situational and variable from institution to institution?
Our group, the Communication, Curriculum, and Culture (C3) Study Group, has developed a tool (the C3 Instrument) to quantitatively measure several characteristics of a medical school's learning environment with respect to patient-centered care.33 Our purpose in this study was to use the C3 Instrument to examine whether characteristics of learning environments with respect to patient-centered care differed across 9 U.S. medical schools.
METHODS
Data Source
We used data from the validation study of the C3 Instrument, which was conducted between March 1, 2002 and May 30, 2003.33 In that study, 890 third- and fourth-year medical students from the classes of 2002 and 2003 at 10 institutions completed an internet-based survey that included the C3 Instrument, and demographic items including age, gender, undergraduate degree, ethnicity, other advanced degrees (e.g., PhD, Masters' degrees), parents' education, extracurricular activities, and medical specialty of interest. The survey also included a previously validated measure of respondents' own attitudes toward patient–centered care.34 Participating institutions represented a diversity of geographical regions, funding source (public vs private), and student class size. We obtained institutional review board approval at all participating institutions.
We calculated participation rates at each school using institutional student rosters for each medical school class. While the overall participation rate was 45%, 1 school had a participation rate that was significantly lower (10%) than the rest of the cohort. We therefore performed all analyses with and without this school's data. There were no differences in any of our analyses based on inclusion or exclusion of this school. We excluded this school from our final report, because of its low participation rate.
Characterizing the Patient-Centered Learning Environment
The C3 Instrument is a 29-item survey completed by students with at least some experience in the clinical years of medical school. The 29 items comprise 5 dimensions that are organized into 3 general content areas: (1) “role modeling” measures the frequency with which students observed teachers modeling patient-centered behaviors in the course of clinical work; (2) “students' experiences” presents students with several vignettes that portray varying levels of patient-centered activities, and measures how often students found themselves in similar scenarios; and (3) “support for students' behaviors” measures how much encouragement students received when they engaged in patient-centered activities. The complete instrument has been published elsewhere33; sample items from each content area appear below:
Role modeling: “Please indicate how often you observed senior residents communicate concern and interest in patients as unique persons” (always, almost always, more than half the time, less than half the time, rarely, never).
Students' experiences: “You hear an attending physician discussing a patient's case history with another attending or house officer. During the course of the conversation, the patient is referred to as a diagnosis (e.g., “I had a great pancreatitis on my team the other day”). Rate how often you have experienced a similar situation” (very often, fairly often, occasionally, rarely, never).
Support for students' behaviors: “In general, when I made an effort to legitimize patients' concerns about their condition or care, my instructors ____________ me.” (completely encouraged, mostly encouraged, slightly encouraged, neither encouraged or discouraged, discouraged).
Prior factor analysis of the C3 Instrument revealed factors with Eigenvalues greater than 1.0 and corresponding to the instrument's dimensions. All items on the instrument had loadings greater than 0.5 on their respective factors. In addition, the dimensions of the instrument exhibited very good to excellent internal consistency, with Cronbach αs ranging from 0.67 to 0.93.33 Summary scores were calculated for each of the 3 content areas separately. The score for each content area represents the mean of its individual item scores. We did not combine content area scores or calculate an “overall score” because the importance of each content area relative to the others is currently unknown.
Data Analysis
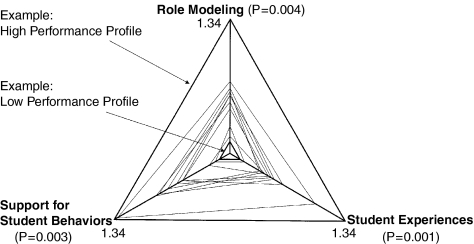
To facilitate comparison and interpretation, we transformed all scores to a 0 to 100 scale. On this scale, higher scores indicate a learning environment that is more supportive of patient-centered care. We performed a multivariate analysis of variance, using students' scores on the 3 content areas as dependent variables, and school ID, gender, age, attitudes toward patient-centered care, and days into clinical experience as independent variables. We report adjusted mean scores and confidence intervals for each school. For each C3 content area, we calculated a “relative score” for each school, defined as the school's adjusted mean divided by the adjusted mean of the lowest-scoring school in that content area. We plotted the schools' relative scores on 3 axes to give a pictorial representation of the overall patient-centered learning environment at the 9 schools.
RESULTS
Characteristics of the 823 students in the final dataset are shown in Table 1. The overall response rate for the 9 schools was 49%, with individual schools' response rates ranging from 35% to 70%. Students' attitudes toward patient-centered care were measured with the Patient-Practitioner Orientation Scale, a previously validated instrument, and are similar to previously published means for students in the clinical years of medical school.16,35 The “days into clinical experience” variable reflects the number of days students had experienced in their clerkship years at the time that they completed the survey.
Table 1.
Students' Characteristics
| Student Characteristic | Percentage or Mean (SD) |
|---|---|
| Age | 27.2 (3.3) |
| Women | 54 |
| Science and technology undergraduate major | 61 |
| White | 61 |
| Advanced degrees (Masters, PhD, professional degrees) | 15 |
| Parents with advanced degree (beyond bachelors degree) | 54 |
| Parents with medical degree (MD or DO) | 15 |
| Involved in organized activities outside of medical school (e.g., religious/civic activities, intramural sports) | 71 |
| Attitudes toward patient-centered care score* | 4.8 (0.6) |
| Interested in primary care specialty† | 25 |
| Days into clinical experience‡ | 523 (161) |
Possible scores range from 1 to 6; higher scores correspond to more patient-centered attitudes.34
Primary care was defined as general internal medicine, general pediatrics, or family and community medicine
Number of days since the start of the clinical years of medical school (day 1 defined as 6/1/2001 for the class of 2002 and 6/1/2002 for the class of 2003)
Adjusted school scores, confidence intervals, and relative scores for each of the C3 content areas are shown in Table 2. After adjusting for student age, gender, attitudes toward patient-centered care, and days into clinical experience, school ID was significantly associated with each of the C3 content scores. P-values for these associations were .001 for students' experiences, .004 for role modeling, and .003 for support for students' behaviors. As is demonstrated in Table 2, each school scored highest in support for students' behaviors, and lowest in students' experiences.
Table 2.
C3 Scores for 9 U.S. Medical Schools*
| School ID | Role Modeling | Students' Experiences | Support for Students' Behaviors |
|---|---|---|---|
| 1 | 60.9 (58,64) [1.08] | 54.7 (52,58) [1.08] | 66.8 (62,72) [1.11] |
| 2 | 56.3 (53,60) [1.00] | 54.0 (51,57) [1.07] | 61.2 (55,67) [1.02] |
| 3 | 63.5 (60,67) [1.13] | 53.1 (50,56) [1.05] | 69.7 (64,75) [1.16] |
| 4 | 63.0 (59,67) [1.12] | 57.3 (54,61) [1.13] | 66.7 (61,72) [1.11] |
| 5 | 58.0 (56,60) [1.03] | 50.6 (48,53) [1.00] | 60.2 (56,64) [1.00] |
| 6 | 65.1 (58,72) [1.16] | 62.5 (56,69) [1.24] | 79.9 (68,91) [1.33] |
| 7 | 64.2 (60,69) [1.14] | 55.6 (52,60) [1.10] | 71.5 (65,78) [1.19] |
| 8 | 61.7 (56,66) [1.10] | 53.6 (50,57) [1.06] | 71.9 (65,78) [1.20] |
| 9 | 63.0 (60,66) [1.12] | 55.1 (52,58) [1.09] | 68.1 (63,73) [1.13] |
School score (95% confidence interval) [relative score], adjusted for age, gender, attitudes toward patient-centered care, and days into clinical experience.
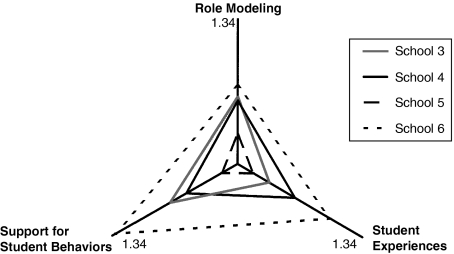
Each school's relative scores in the 3 content areas are represented graphically in Figure 1. Each axis in the figure represents a content area; our calculation of a relative score for each school represents an attempt to normalize the data along each axis. The P values in the figure pertain to the difference among schools along each axis. As the relative scores ranged from 1.00 to 1.33, the scales of each of the axes in the figure range from 0.95 to 1.34. For this dataset, therefore, a school whose learning environment is minimally patient-centered compared with other schools would be represented by a small triangle, and a school that is maximally patient-centered would have the shape of a large triangle. For reference, the bold triangles indicate high and low performance profiles. Figure 1 demonstrates that different schools have different C3 profiles, as reflected in the shapes and sizes of the triangles. To reduce the complexity of the figure and highlight some of the diversity among schools, we plotted Schools #3 to 6 in Figure 2. In this figure, Schools #5 and 6 have global differences in magnitude in all C3 content areas. Schools #3 and 4, by contrast, have triangles that are roughly equal in size, but are shaped differently. School #3 performed at its best (relative to other schools) in the support for student behaviors content area, whereas School #4 performed at its best in the students' experiences area. While none of the schools could be considered to perform ideally in all dimensions, they vary considerably by dimension in “room to improve.”
Figure 1.
Relative characteristics of patient-centered learning environments at 9 U.S. medical schools.
Figure 2.
Relative learning environment patterns at 4 sample schools.
DISCUSSION
We conducted this study to ask whether patient-centered learning environments at 9 schools were substantially similar or different, both in strength and character. Our results indicate a more complex reality than the question would suggest.
The learning environments at the 9 institutions differed significantly in magnitude in all 3 areas that the C3 Instrument measures. Each school demonstrated differences in their support of role modeling, students' experiences, and support for students' actions. This finding sharply contrasts with the previously held notion that learning environments (as articulated in the singular term “hidden curriculum”) are similar across institutions.
Of the 3 content areas on the C3 Instrument, all schools scored highest on support for students' behaviors, and lowest on students' experiences. One possible explanation for this finding is that faculty and residents are comfortable giving positive feedback to students, making the reinforcement of patient-centered behaviors relatively easy to accomplish. Conversely, the unscripted experiences that students encounter are not as easily controlled, and often arise in the stressful, demanding, and chaotic environments of the hospital and clinic. It is possible that our biggest challenge is to discover the formula to change what our students and patients experience, and to actively learn about the circumstances that produce suboptimal responses from us as medical educators and care providers.36
While all of the schools scored highest on support for students' behaviors, the patterns of individual schools' scores relative to the others were not consistent. As demonstrated in the figures, some schools showed a balance between the 3 content areas, while other schools showed differential degrees of patient-centeredness between content areas. The implication for administrators and educators is that gaining an understanding of the unique nature of one's institutional learning environment is important, because it can inform one's efforts at change. For example, educators at School #3 may choose to focus on aspects that affect students' experiences rather than on those that affect support for students' behaviors. School #4 may choose the converse, or choose to collaborate with School #3 to learn about each others' strengths. School #5 may wish to address any of the C3 content areas, whereas School #6 might create support for the patient-centered environment that appears already to exist. One of the advantages of the C3 Instrument is that by categorizing the patient-centered learning environment into 3 separate and potentially mutable areas, medical educators may be able to develop effective interventions. In an era of limited resources for curriculum reform, being able to systematically collect data and direct attention can help schools to maximize the impact of their efforts.
Before the development of the C3 Instrument, no quantitative measures of the patient-centered learning environment existed. Our data open the door to a new area of potential quality improvement for medical education. Several schools have already begun to implement innovative strategies to reform their learning environment.37–39 The C3 Instrument can augment such efforts, because it provides a validated tool that can easily evaluate interventions, both formatively and summatively. We suggest that further work is needed both to understand and apply C3 Instrument results, and to develop tools to measure other aspects of medical schools' learning environments.
We note several important limitations to this study. First, the dataset we used contains data also used to validate the C3 Instrument, so our findings may be unique to the schools we surveyed. Second, we did not assess outcomes data, such as objective measures of graduating students' patient-centered skills. Therefore, we are unable to interpret the meaning of differences in scores between schools or to determine the relative importance of the 3 content areas on the instrument. In our future work, we plan to collect outcomes information in addition to C3 Instrument data in order to corroborate our findings, inform the scoring procedures for the instrument, and build meaning about its results. A final limitation is that the relatively small number of medical schools and the modest response rate at those schools may influence the generalizability of our results. Given the ease with which the C3 Instrument can be administered (the final version of the instrument takes students approximately 15 minutes to complete), we advocate for collaborative work to collect additional data from a larger and possibly more representative number of institutions.
In conclusion, we measured characteristics of the patient-centered learning environment at 9 medical schools, and demonstrated important similarities and differences between these institutions. We advocate for continued systematic study of learning environments in medical education, both to understand the relative effectiveness of efforts aimed at change, and to understand the effects of the learning environment on the patient-centered behaviors of graduates.
Acknowledgments
Supported by grants from the Bayer Institute for Health Care Communication and the Baylor College of Medicine Academy of Distinguished Educators Fullbright and Jaworski Fund for Medical Education Research. At the time of this writing, Drs. Haidet, Kelly, and Helmer were supported by career development awards from the Office of Research and Development, Health Services R&D Service, U.S. Department of Veterans Affairs. A mentoring relationship between Drs. Inui (mentor) and Haidet (mentee) is supported by a research mentorship award from the Society of General Internal Medicine. In addition to the authors, the Communication, Curriculum, and Culture Study Group includes Vinay Babu, MD, Mark Kuebeler, MS, Gregory Makoul, PhD, Linda Perkowski, PhD, Boyd Richards, PhD, A. Lynn Snow, PhD, and Julianne Souchek, PhD. The opinions contained herein are those of the authors and do not necessarily represent the views of the U.S. Department of Veterans Affairs, The Bayer Institute for Health Care Communication, or the institutions of the C3 Study Group Investigators.
REFERENCES
- 1.Makoul G, Schofield T. Communication teaching and assessment in medical education: an international consensus statement. Netherlands Institute of Primary Health Care. Patient Educ Couns. 1999;37:191–5. doi: 10.1016/s0738-3991(99)00023-3. [DOI] [PubMed] [Google Scholar]
- 2.Contemporary Issues in Medicine: Communication in Medicine. Washington, DC: The Association of American Medical Colleges; 1999. Report III of the Medical School Objectives Project. [PubMed] [Google Scholar]
- 3.Beckman HB, Frankel RM. Training practitioners to communicate effectively in cancer care: it is the relationship that counts. Patient Educ Couns. 2003;50:85–9. doi: 10.1016/s0738-3991(03)00086-7. [DOI] [PubMed] [Google Scholar]
- 4.Haidet P, Paterniti DA. “Building” a history rather than “taking” one: a perspective on information sharing during the medical interview. Arch Intern Med. 2003;163:1134–40. doi: 10.1001/archinte.163.10.1134. [DOI] [PubMed] [Google Scholar]
- 5.The Accreditation Council for Graduate Medical Education Outcome Project. [April 29, 2005]; doi: 10.1097/00001503-200212000-00009. Available at http://www.acgme.org/outcome. [DOI] [PubMed]
- 6.Eckhert NL. Step 2 clinical skills examination. Med Encounter. 2004;18:7–9. [Google Scholar]
- 7.The American Board of Internal Medicine Maintenance of Certification Program. [April 29, 2005]. Available at http://www.abim.org/moc.
- 8.Becker HS, Geer B, Hughes EC, Strauss AL. Chicago: University of Chicago Press; 1961. Boys in White: Student Culture in Medical School. [Google Scholar]
- 9.Hafferty FW. New Haven: Yale University Press; 1991. Into the Valley: Death and the Socialization of Medical Students. [Google Scholar]
- 10.Branch WT, Kern D, Haidet P, et al. Teaching the human dimensions of care in clinical settings. JAMA. 2001;286:1067–74. doi: 10.1001/jama.286.9.1067. [DOI] [PubMed] [Google Scholar]
- 11.Hafferty FW. Beyond curriculum reform: confronting medicine's hidden curriculum. Acad Med. 1998;73:403–7. doi: 10.1097/00001888-199804000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Stein HF. Boulder, CO: Westview Press; 1990. American Medicine as Culture. [Google Scholar]
- 13.Hundert EM, Douglas-Steele D, Bickel J. Context in medical education: the informal ethics curriculum. Med Educ. 1996;30:353–64. doi: 10.1111/j.1365-2923.1996.tb00847.x. [DOI] [PubMed] [Google Scholar]
- 14.Haas J, Shaffir W. Greenwich, CT: JAI Press; 1987. Becoming Doctors: The Adoption of a Cloak of Competence. [Google Scholar]
- 15.Stern DT. Practicing what we preach? An analysis of the curriculum of values in medical education. Am J Med. 1998;104:569–75. doi: 10.1016/s0002-9343(98)00109-0. [DOI] [PubMed] [Google Scholar]
- 16.Haidet P, Paterniti DA, Dains J, et al. Medical student attitudes toward the physician-patient relationship. Med Educ. 2002;36:568–74. doi: 10.1046/j.1365-2923.2002.01233.x. [DOI] [PubMed] [Google Scholar]
- 17.Pfeiffer C, Madray H, Ardolino A, Willms J. The rise and fall of students' skill in obtaining a medical history. Med Educ. 1998;32:283–8. doi: 10.1046/j.1365-2923.1998.00222.x. [DOI] [PubMed] [Google Scholar]
- 18.Craig JL. Retention of interviewing skills learned by first year medical students: a longitudinal study. Med Educ. 1992;26:276–81. doi: 10.1111/j.1365-2923.1992.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 19.Engler CM, Saltzman GA, Walker ML, Wolf FM. Medical student acquisition and retention of communication and interviewing skills. Med Educ. 1981;56:572–9. doi: 10.1097/00001888-198107000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Wright AD, Green ID, Fleetwood-Walker PM, Bishop JM, Wishart EH, Swire H. Patterns of acquisition of interview skills by medical students. Lancet. 1980;2:964–6. doi: 10.1016/s0140-6736(80)92116-9. [DOI] [PubMed] [Google Scholar]
- 21.Branch WT., Jr Supporting the moral development of medical students. J Gen Int Med. 2000;15:503–8. doi: 10.1046/j.1525-1497.2000.06298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feudtner C, Christakis DA. Making the rounds. The ethical development of medical students in the context of clinical rotations. Hastings Center Rep. 1994;24:6–12. [PubMed] [Google Scholar]
- 23.Feudtner C, Christakis DA. Ethics in a short white coat; the ethical dilemmas that medical students confront. Acad Med. 1993;68:249–64. doi: 10.1097/00001888-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Self D, Baldwin D. Moral reasoning in medicine Moral Development in the Professions. Psychogy and Applied Ethics. In: Rest JR, editor. Hillsdale, NJ: Lawrence Erlbaum Associates; 1994. pp. 147–62. [Google Scholar]
- 25.Feudtner C, Christakis DA, Christakis NA. Do clinical clerks suffer ethical erosion? Students perception of their ethical environment and personal development. Acad Med. 1994;69:669–70. doi: 10.1097/00001888-199408000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Merton RK, Reader GG, Kendal PI, editors. Cambridge: Harvard University Press; 1957. The Student-Physician: Introductory Studies in the Sociology of Medical Education. [Google Scholar]
- 27.Konner M. New York: Penguin Books; 1988. Becoming a Doctor: A Journey of Initiation in Medical School. [Google Scholar]
- 28.Seabrook MA. Intimidation in medical education: students' and teachers' perspectives. Stud Higher Educ. 2004;29:59–74. [Google Scholar]
- 29.Coombs RH. New York: Free Press; 1978. Mastering Medicine: Professional Socialization in Medical School. [Google Scholar]
- 30.DelVecchio-Good MJ. Berkeley: University of California Press; 1995. American Medicine: The Quest for Competence. [Google Scholar]
- 31.Klass P. New York: GP Putnam; 1987. A Not Entirely Benign Procedure. [Google Scholar]
- 32.Katz P. Needham Heights, MA: Allyn & Bacon; 1999. The Scalpel's Edge: The Culture of Surgeons. [Google Scholar]
- 33.Haidet P, Kelly PA, Chou C, et al. Characterizing the patient-centeredness of hidden curricula in medical schools: development and validation of a new measure. Acad Med. 2005;80:44–50. doi: 10.1097/00001888-200501000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Krupat E, Bell RA, Kravitz RL, Thom D, Azari R. When patients and physicians think alike: patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001;50:1057–62. [PubMed] [Google Scholar]
- 35.Haidet P, Dains JE, Paterniti DA, Chang T, Tseng E, Rogers JC. Medical students' attitudes toward patient-centered care and standardized patients' perceptions of humanism: a link between attitudes and outcomes. Acad Med. 2001;76(suppl):s42–s4. doi: 10.1097/00001888-200110001-00015. [DOI] [PubMed] [Google Scholar]
- 36.Inui TS. Washington, DC: Association of American Medical Colleges; 2003. A Flag in the Wind: Educating for Professionalism in Medicine. [Google Scholar]
- 37.Suchman AL, Williamson PR, et al. the Relationship-Centered Care Discovery Team. Toward an informal curriculum that teaches professionalism: transforming the social environment of a medical school. J Gen Intern Med. 2004;19(Part 2):501–4. doi: 10.1111/j.1525-1497.2004.30157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haidet P, Caudill TS, Knight C. Innovation and community among medical educators. SGIM Forum. 2005;28:4–10. [Google Scholar]
- 39.Hatem D, Ferrara E. Becoming a doctor: fostering humane caregivers through creative writing. Patient Educ Couns. 2001;45:13–22. doi: 10.1016/s0738-3991(01)00135-5. [DOI] [PubMed] [Google Scholar]