Abstract
BACKGROUND
Many inpatients receive stress ulcer prophylaxis (SUP) inappropriately. This indiscriminate usage increases costs and avoidable side-effects. Practice-based learning and improvement (PBLI) methodology may improve compliance with published guidelines.
OBJECTIVE
To investigate the response of internal medicine residents to an educational intervention regarding SUP.
DESIGN
A prospective, pre and postintervention cohort study using an educational intervention based on PBLI.
PATIENTS
Three groups of consecutively admitted patients (1 group preintervention and 2 groups postintervention) on the medicine ward at a University Hospital.
MAIN OUTCOME MEASURE
Rates of inappropriate SUP prescription and discharge with an inappropriate prescription.
RESULTS
One month after the intervention, inappropriate prophylaxis was significantly decreased (59% pre, 29% postintervention, P<.002). The rate of discharge with an inappropriate prescription also decreased, but was not significant (25% pre, 14% postintervention, P = .14). In the 6-month postintervention cohort, inappropriate SUP remained lower (59% pre, 33% postintervention, P<.007). The rate of discharge with an inappropriate prescription was also significantly lower (25% pre, 7% postintervention, P<.009).
CONCLUSION
Practice-based learning and improvement can improve compliance with published guidelines, and change practice patterns. After the intervention, both inappropriate prophylaxis and inappropriate prescriptions upon discharge were reduced. Importantly, the intervention was sustained, transmitted across academic years to a new class of interns who had not directly experienced the intervention.
Keywords: stress ulcer prophylaxis, practice-based learning and improvement
While gastrointestinal (GI) bleeding attributed to stress ulcers in patients admitted to an intensive care unit is a serious problem with significant associated morbidity and mortality, not all hospitalized patients are at significant risk for stress ulcers.1,2 Clinical guidelines based on prospective multicenter trials describe the appropriate indications and usage of agents to reduce the incidence of GI bleeding associated with critical illness.3–5 These indications are limited to prolonged mechanical ventilation and the presence of coagulopathy.
Despite the presence of guidelines that delineate the limited populations that derive benefit from stress ulcer prophylaxis (SUP), multiple studies have estimated that 27% to 50% of hospitalized patients receive these “prophylactic” medicines.6–8 Importantly, approximately half of these treated patients are subsequently discharged with prescriptions for these medications, an additional burden to both the patient and the health care system.1,7,9,10
In the present study, we sought to measure the baseline rates of inappropriate SUP as well as the results of a simple, low-cost intervention aimed at improving adherence. We report the results of our effective, sustainable, and low-cost intervention using practice-based learning and improvement (PBLI) methodology to reduce the inappropriate use of SUP.
METHODS
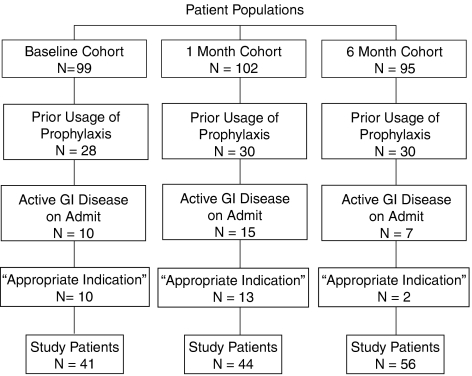
The University of Chicago Hospitals is a 577-bed tertiary care hospital with an affiliated residency program in Internal Medicine. We prospectively measured rates of usage of SUP at 3 separate times: at baseline (preintervention) and at 2 separate times postintervention. Each time, consecutive patients were approached until approximately 100 had been enrolled. We also measured rates of discharge with a new prescription for these medications. “Prophylaxis” was defined as sustained (>1 day) administration of an acid-suppressive medicine (H2 blocker or proton pump inhibitor [PPI]) that was not for purposes of treatment of active GI disease, based on medical record review. The American Society of Health-Systems Pharmacists (ASHP) has published guidelines that describe the appropriate indications for the usage of SUP, and they are: (1) mechanical ventilation for >48 hours, and (2) presence of coagulopathy, defined as INR>1.5, PTT>2 × normal or platelet count <50,000. Therefore, if the patient had either of these indications and was receiving SUP, this was deemed “appropriate.” All other cases were deemed “inappropriate.” Patients were excluded from analysis if they had active GI disease on admission or had a preexisting prescription for the medications (Chart 1). Rates of usage, class of acid-suppressive agent, and the presence of side-effects attributed to the medication were determined by chart review.
After data collection, a practice-based educational intervention for the house staff was implemented. The intervention consisted of a 1-hour presentation based on the principles of PBLI. These principles include understanding and appraising the evidence for a specific clinical activity, analyzing one's own practice data, and comparing those data against expected outcomes and goals of care, and finally, adjusting one's practice patterns to achieve those outcomes and goals.11 During the intervention, we described the incidence of stress-related mucosal disease, its risk factors, the efficacy of the different medications, and their potential side-effects. We presented data describing the overusage of SUP and also presented published cost-analyses of prophylaxis. In keeping with the principles of PBLI, we presented the residents with feedback on their own practice patterns, including the results of our baseline assessment of the rates of prophylaxis and discharge with prophylaxis for the house staff. We performed an informal cost analysis of the house staff's prescribing behavior, and finished the educational intervention with a presentation and discussion of the ASHP recommended guidelines.
Stress ulcer prophylaxis use was measured again at 1 month and at 6 months, in similar populations, and compared with preintervention rates. The 6-month follow-up occurred several months after the beginning of a new academic year. There was no follow-up information given to the house staff during this time period, and the house staff did not receive updates on their practice patterns after the intervention.
The hospital's IRB approved all investigations. Patients who were consecutively admitted to the general medicine floor services were approached for inclusion in the study, and informed consent was obtained from each patient prior to chart review. On average, 130 patients in each cohort were approached in order to achieve the desired goal of 100 patients enrolled (Fig. 1). All statistics were analyzed using software supplied by STATA™ (College Station, TX). A P value of less than .05 was considered to indicate statistical significance, and all hypotheses testing were 2-tailed. All data were analyzed based on the intention-to-treat principle.
Figure 1.
Description of patients in each cohort
RESULTS
The charts of 4 patients in the preintervention group, 1 patient in the 1-month group, and 8 patients in the 6-month group were unavailable for review. Baseline characteristics were similar in the pre and postintervention patients.
In the baseline preintervention cohort, 59% of patients in the study inappropriately received SUP. Twenty-five of these patients were subsequently discharged with a prescription for these medications.
In the 1-month postintervention cohort, the rate of inappropriate prophylaxis fell to 29% (P<.002). The rate of discharge from the hospital with an inappropriate prescription for these medications was 14% (P = .14).
In the 6-month postintervention cohort, the rate of inappropriate prophylaxis with either PPI or H2 blocker remained significantly low, with a value of 33% (P<.007). The rate of discharge from the hospital with an inappropriate prescription decreased even more, to a value of 7% (P<.009) (Table 1).
Table 1.
Rates of Inappropriate Stress Ulcer Prophylaxis Prescription
| Baseline Cohort | One Month Cohort | Six Months Cohort | |
|---|---|---|---|
| Inappropriately receiving prophylaxis | 24/41 (59%) | 13/44 (29%, P<.002) | 18/56 (33%, P<.007) |
| Inappropriately discharged with prescription | 10/41 (25%) | 17/44 (14%, P = .14) | 4/56 (7%, P<.009) |
DISCUSSION
This study demonstrated that a low-cost educational intervention based on the principles of PBLI can positively impact patient care. After implementing the intervention, rates of inappropriate SUP were significantly reduced, sparing one out of every 3 patients an inappropriate medication. The number of inappropriate prescriptions upon discharge was also dramatically reduced. However, this study had 2 important advantages over previously published interventions that aimed to improve adherence to guidelines through strategies that addressed barriers to physician adherence.9–12 The only cost associated with this intervention was investigator time, and because it used a “train the trainer” approach, the effects were sustained and may have even improved overtime.
This study used a PBLI methodology, modeling a quality improvement project for the entire residency, and adding value to both clinical care and medical education for the residents and their patients.11 Practice-based learning and improvement-based interventions will not be universally effective. This problem, however, was well suited for this type of intervention for many reasons. It is a very common clinical scenario and, based on a preevaluation survey, we discovered that house officers learned about prophylaxis from their supervising residents. There are also clear, objective, and limited indications for the appropriate use of prophylaxis making a focused measurement relatively easy.
There are limitations to this study. It is a pre and postintervention study rather than a randomized-controlled trial. However, we studied consecutively admitted patients who were admitted to 8 different teams with 24 house staff members in each investigative period. This should have decreased the potential variability caused by differences between individual residents. Additionally, as the proposed method of effect was through within-program dissemination and culture change, a simultaneous control would be impossible to identify. Additionally, our study was a small study performed at only 1 hospital, which may limit its generalizability. Finally, although theoretically there may have been a confounding trend toward a decrease in SUP usage at that time, our preintervention rates of prophylaxis were similar to that seen in other studies and we know of no secular trends or other newly enacted hospital policies designed to reduce SUP usage during the time of this intervention.10,12,13
Perhaps most intriguing is what may appear to be an ongoing enhancement of effect seen at 6 months, as evidenced by the lower rate of inappropriate discharge use. This may simply reflect the small study size and may not be truly lower. However, if the point estimate reflects a true drop, that would support the proposed mechanism for the effect. The new class of interns would have been taught prophylaxis use by house officers who were part of the intervention. Not only does this study support the idea that PBLI can improve clinical practice, but that these methods can be incorporated into residency training programs through QI projects and provide meaningful educational opportunities.
We focused on providing residents with the tools they need to practice and teach appropriate, safe, and cost-effective medicine. We feel that that as a result, our intervention had a lasting effect that was transmitted across academic years to a new class of interns who had never directly experienced the intervention. This suggests that when we teach the teachers, our lessons can be self-perpetuating.
Footnotes
Funding source: There was no funding source for this research. The primary author had full access to all the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Ben-Menachem T, McCarthy BD, Fogel R, et al. Prophylaxis for stress-related gastrointestinal hemorrhage. Crit Care Med. 1996;24:338–45. doi: 10.1097/00003246-199602000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Cook DJ, Fuller HD, et al. Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med. 1994;330:377–81. doi: 10.1056/NEJM199402103300601. [DOI] [PubMed] [Google Scholar]
- 3.Cook D, Heyland D, Griffith L, Cook R, Marshall J, Pagliarello J. Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Crit Care Med. 1999;27:2812–7. doi: 10.1097/00003246-199912000-00034. [DOI] [PubMed] [Google Scholar]
- 4.Terdiman JP, Ostroff JW. Gastrointestinal bleeding in the hospitalized patient: a case-control study to assess risk factors, causes, and outcome. Am J Med. 1998;104:349–54. doi: 10.1016/s0002-9343(98)00055-2. [DOI] [PubMed] [Google Scholar]
- 5.American Society of Health System Pharmacists. ASHP therapeutic guidelines on stress ulcer prophylaxis. Am J Health Syst Pharm. 1999;56:347–79. doi: 10.1093/ajhp/56.4.347. [DOI] [PubMed] [Google Scholar]
- 6.Nardino RJ, Vender RJ, Herbert PN. Overuse of acid-suppressive therapy in hospitalized patients. Am J Gastroenterol. 2000 Nov;95:3118–22. doi: 10.1111/j.1572-0241.2000.03259.x. [DOI] [PubMed] [Google Scholar]
- 7.Lam NP, Le PD, Crawford SY, Patel S. National survey on stress ulcer prophylaxis. Crit Care Med. 1999;27:98–103. doi: 10.1097/00003246-199901000-00034. [DOI] [PubMed] [Google Scholar]
- 8.Frankel HL, FitzPatrick MK, Gaskell S, Hoff WS, Rotondo MF, Schwab CW. Strategies to improve compliance with evidence-based clinical management guidelines. J Am Coll Surg. 1999;189:533–8. doi: 10.1016/s1072-7515(99)00222-7. [DOI] [PubMed] [Google Scholar]
- 9.Barletta JF, Erstad BL, Fortune JB. Stress ulcer prophylaxis in trauma patients. Crit Care. 2002;6:526–30. doi: 10.1186/cc1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:458–86. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 11.Accreditation Council for Graduate Medical Education. Advancing Education in Practice-Based Learning and Improvement. [January 15, 2006]; Available at http://www.acgme.org/outcome/implement/complete_PBLIBooklet.pdf.
- 12.Erstad BL, Barletta JF, Jacobi J, et al. Survey of stress ulcer prophylaxis. Crit Care. 1999;3:145–9. doi: 10.1186/cc368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devlin JW, Claire KS, Dulchavsky SA, Tyburski JG. Impact of trauma stress ulcer prophylaxis guidelines on drug cost and frequency of major gastrointestinal bleeding. Pharmacotherapy. 1999;19:452–60. doi: 10.1592/phco.19.6.452.31049. [DOI] [PubMed] [Google Scholar]