Abstract
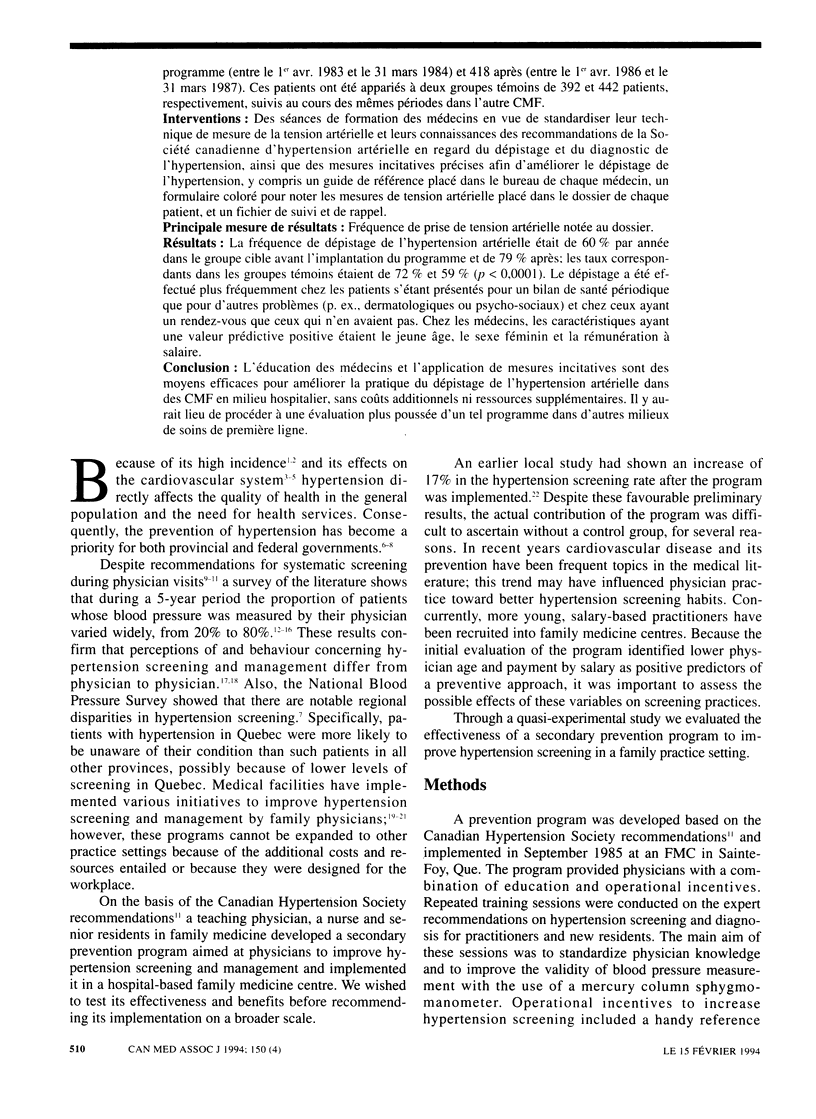
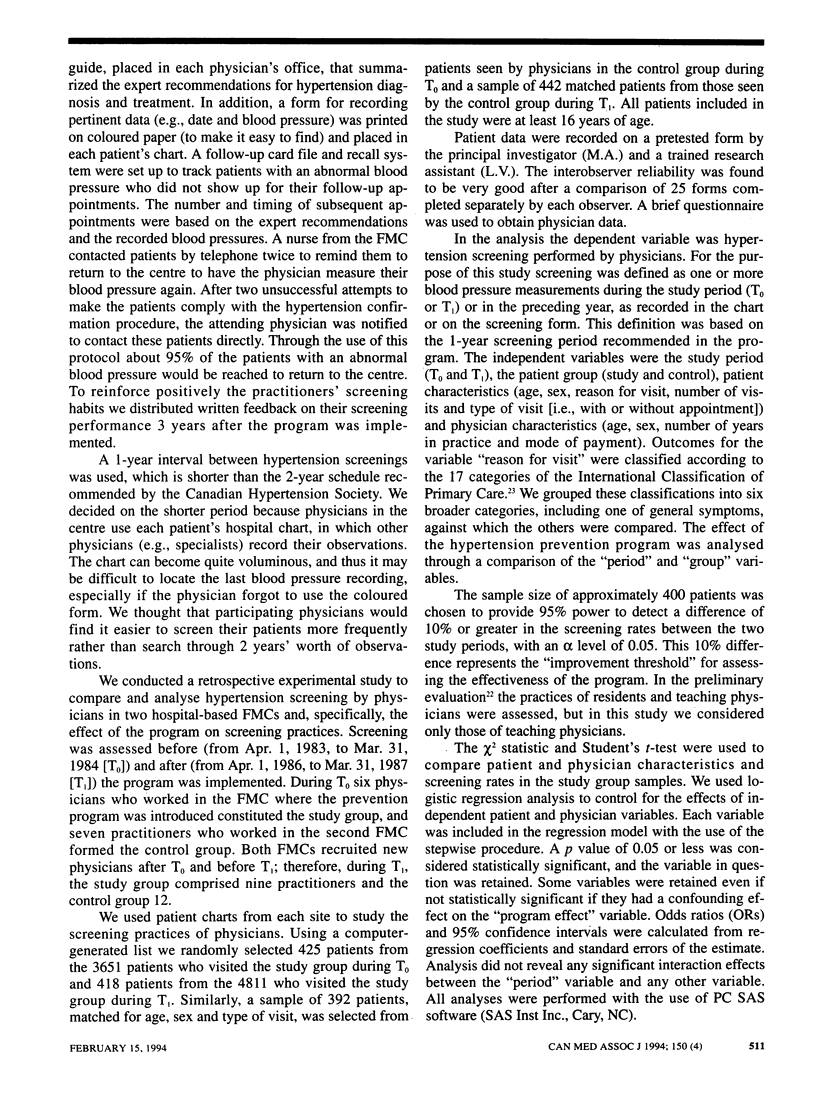
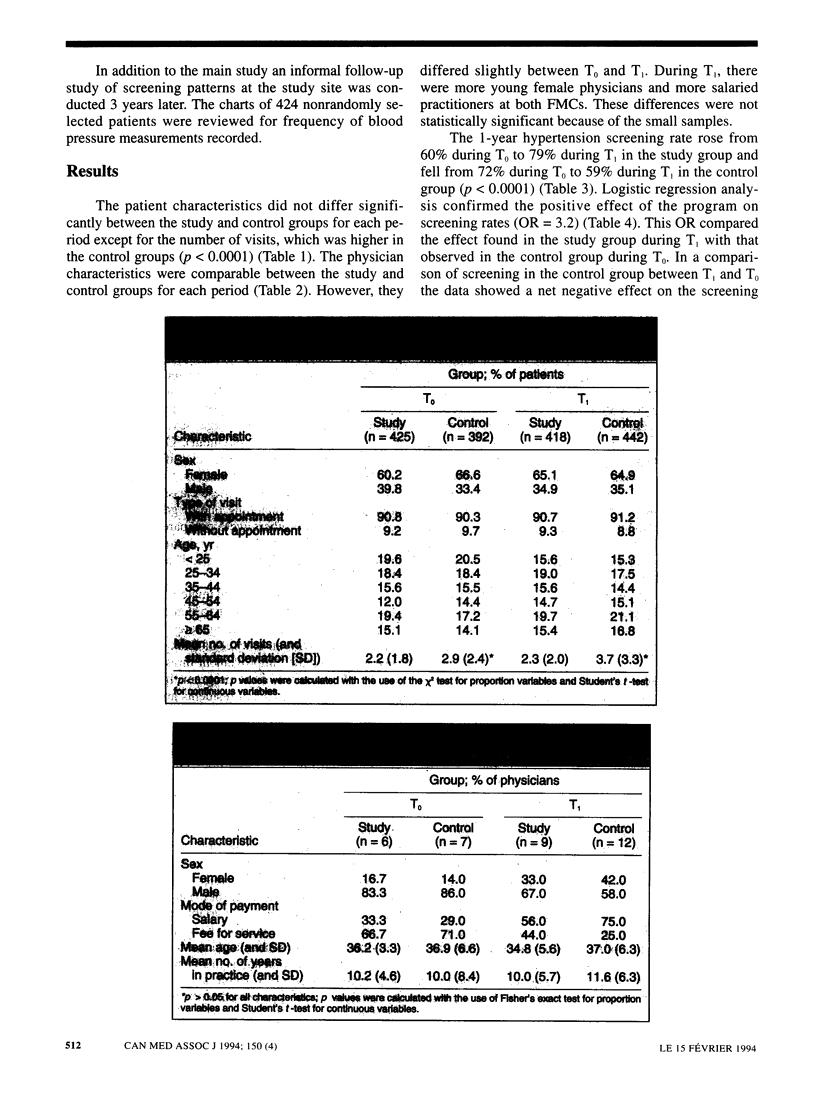
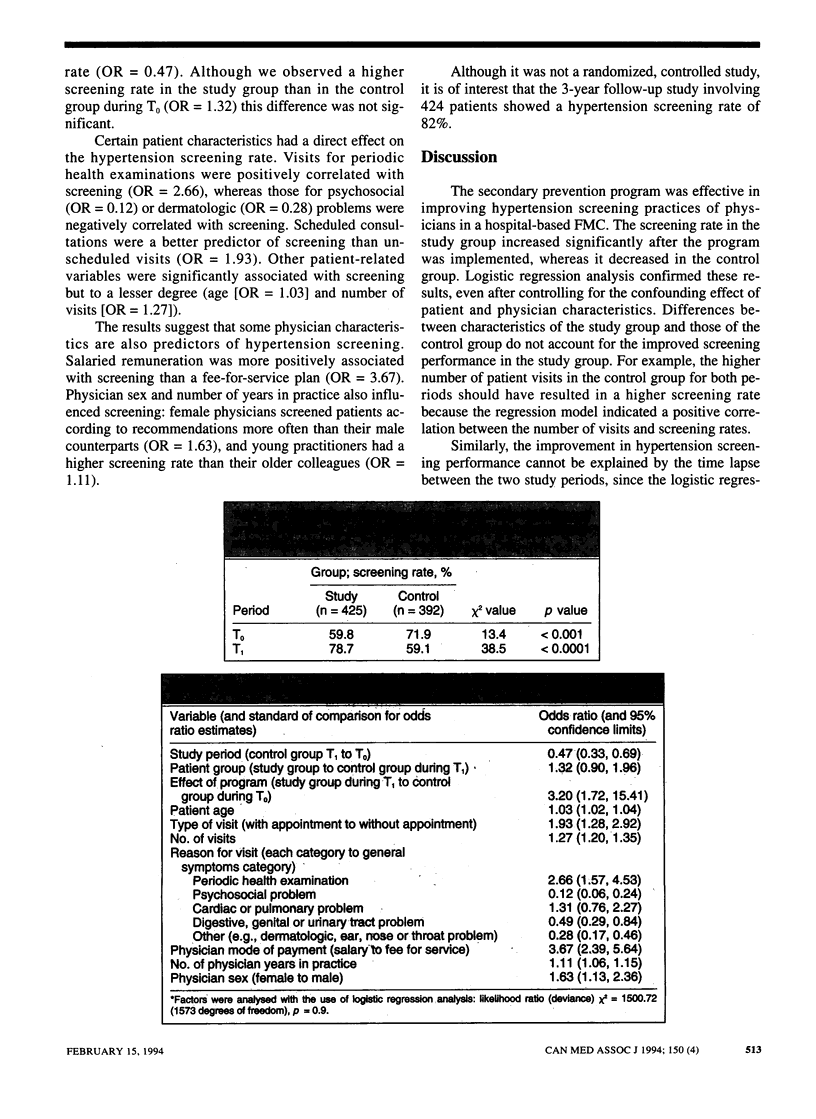
OBJECTIVE: To evaluate the effectiveness of a program to improve hypertension screening practices in primary care. DESIGN: Retrospective quasi-experimental study. SETTING: Two hospital-based family medicine centres (FMCs). PATIENTS: In the study FMC, two study groups of randomly selected adult patients: 425 who visited the FMC before implementation of the screening improvement program (from Apr. 1, 1983, to Mar. 31, 1984) and 418 who visited it afterward (from Apr. 1, 1986, to Mar. 31, 1987). These patients were matched with 392 and 442 control patients respectively seen during the same time frames at the second FMC. INTERVENTIONS: Educational sessions for physicians to standardize blood pressure measurement and knowledge of the recommendations from the Canadian Hypertension Society on hypertension screening and diagnosis, and specific operational incentives to improve hypertension screening, including a reference guide placed in each physician's office, a coloured form for recording blood pressure measurements placed in every patient's chart and a follow-up and recall card file. MAIN OUTCOME MEASURE: Frequency of blood pressure measurements recorded in patient charts. RESULTS: The hypertension screening rate was 60% per year in the study group before program implementation and 79% in the study group afterward; the corresponding rates in the two control groups were 72% and 59% (p < 0.0001). Patients were more likely to be screened if they visited the physician for a periodic health examination than for other problems (e.g., psychosocial or dermatologic) and if they had a scheduled appointment rather than no appointment. Physician characteristics that were positive predictors of screening were low age, female sex and payment on a salary basis. CONCLUSION: Physician education and incentives are effective in improving hypertension screening practices in hospital-based FMCs without incurring additional costs or other use of resources. Further evaluation of such a program should be undertaken in other primary care settings.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aubin M., Vézina L., Fortin J. P., Bernard P. M. Un projet d'intervention efficace pour le dépistage de l'hypertension artérielle en médecine familiale. Union Med Can. 1992 Jul-Aug;121(4):227–232. [PubMed] [Google Scholar]
- Bass M. J., McWhinney I. R., Donner A. Do family physicians need medical assistants to detect and manage hypertension? CMAJ. 1986 Jun 1;134(11):1247–1255. [PMC free article] [PubMed] [Google Scholar]
- Battista R. N. Adult cancer prevention in primary care: patterns of practice in Québec. Am J Public Health. 1983 Sep;73(9):1036–1039. doi: 10.2105/ajph.73.9.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battista R. N., Williams J. I., MacFarlane L. A. Determinants of primary medical practice in adult cancer prevention. Med Care. 1986 Mar;24(3):216–224. doi: 10.1097/00005650-198603000-00004. [DOI] [PubMed] [Google Scholar]
- Cypress B. K. The role of ambulatory medical care in hypertension screening. Am J Public Health. 1979 Jan;69(1):19–24. doi: 10.2105/ajph.69.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn E., Hilditch J., Chipman M., Hardacre G., Morrison M. Diagnosis and management of hypertension: the stated practices of family physicians. Can Med Assoc J. 1984 Apr 15;130(8):985–988. [PMC free article] [PubMed] [Google Scholar]
- Fleming D. M., Lawrence M. S. An evaluation of recorded information about preventive measures in 38 practices. J R Coll Gen Pract. 1981 Oct;31(231):615–620. [PMC free article] [PubMed] [Google Scholar]
- Gordon T., Kannel W. B. Predisposition to atherosclerosis in the head, heart, and legs. The Framingham study. JAMA. 1972 Aug 14;221(7):661–666. [PubMed] [Google Scholar]
- Kannel W. B. Some lessons in cardiovascular epidemiology from Framingham. Am J Cardiol. 1976 Feb;37(2):269–282. doi: 10.1016/0002-9149(76)90323-4. [DOI] [PubMed] [Google Scholar]
- Maheux B., Dufort F., Lambert J., Berthiaume M. Do female general practitioners have a distinctive type of medical practice? CMAJ. 1988 Oct 15;139(8):737–740. [PMC free article] [PubMed] [Google Scholar]
- Michael G. Quality of care in managing hypertension by case finding in north west London. Br Med J (Clin Res Ed) 1984 Mar 24;288(6421):906–908. doi: 10.1136/bmj.288.6421.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radecki S. E., Mendenhall R. C. Patient counselling by primary care physicians: results of a nationwide survey. Patient Educ Couns. 1986 Jun;8(2):165–177. doi: 10.1016/0738-3991(86)90087-x. [DOI] [PubMed] [Google Scholar]
- Ritchie L. D., Currie A. M. Blood pressure recording by general practitioners in north-east Scotland. Br Med J (Clin Res Ed) 1983 Jan 8;286(6359):107–109. doi: 10.1136/bmj.286.6359.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robitaille N. M., Dagenais G. R., Rochon J., Lupien P. J. Incidence d'hypertension artérielle dans la région de Québec. Clin Invest Med. 1983;6(1):39–42. [PubMed] [Google Scholar]


