Abstract
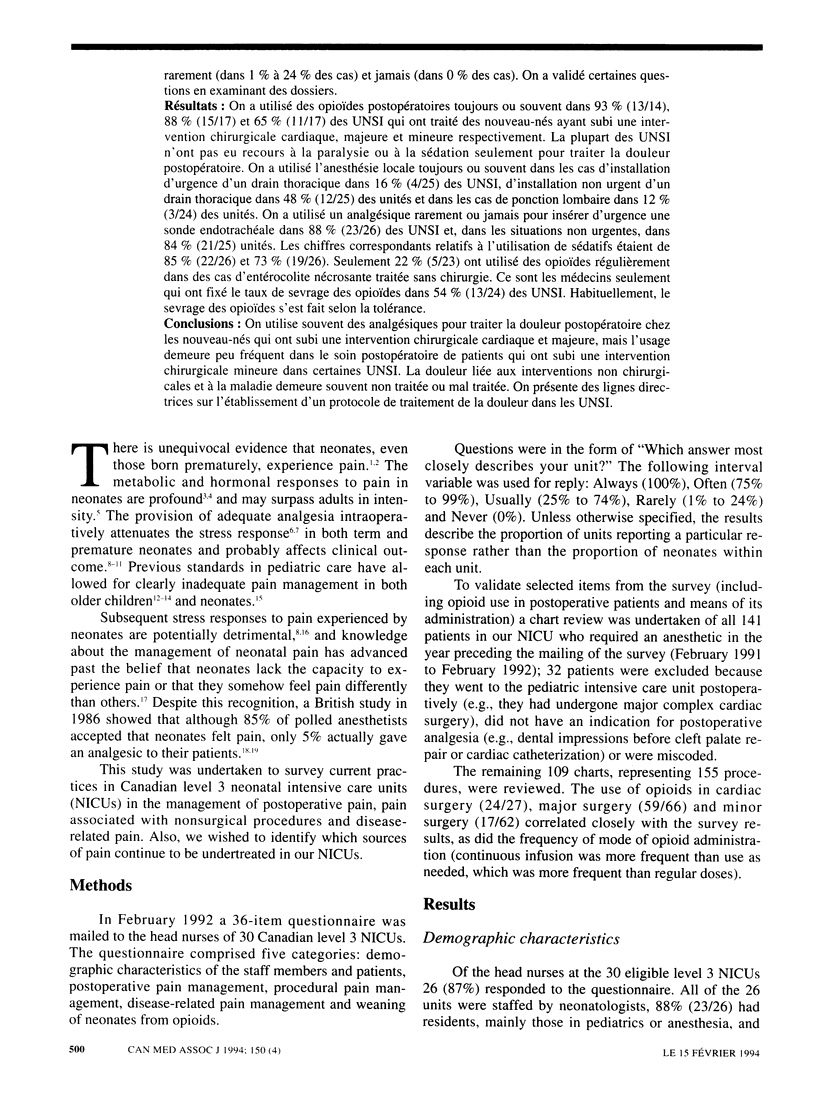
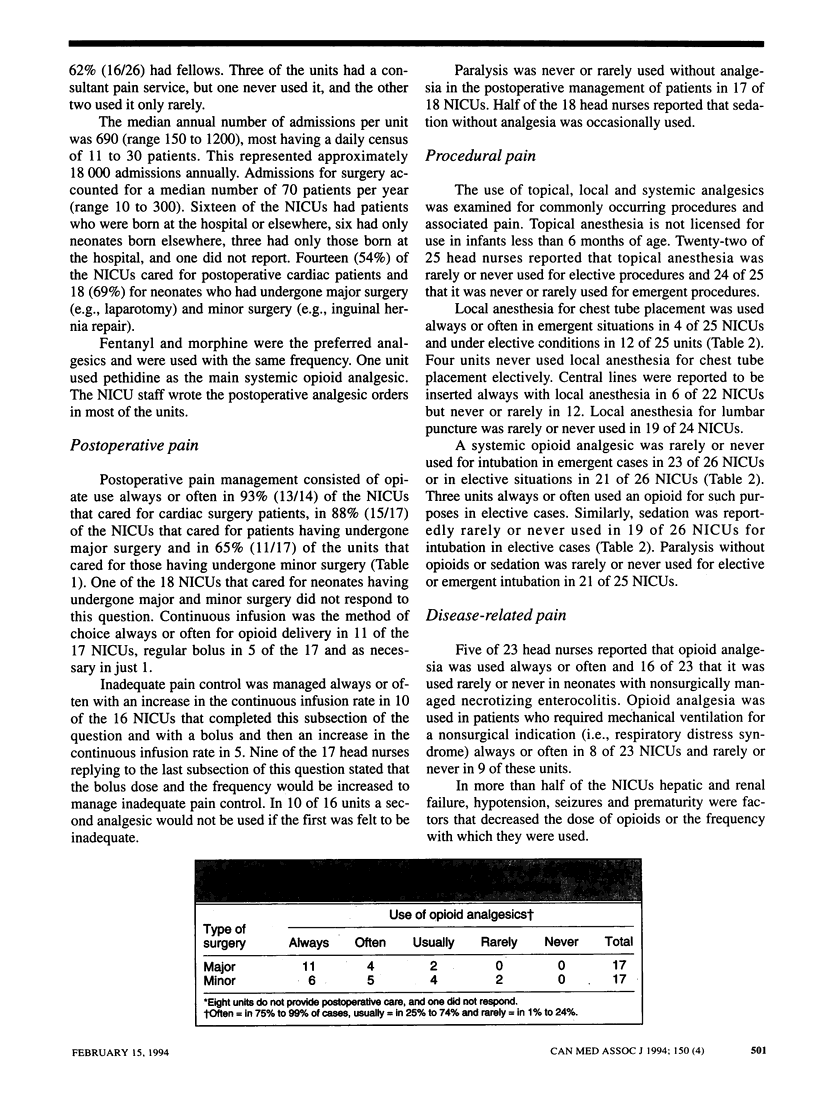
OBJECTIVE: To determine current practices in neonatal intensive care units (NICUs) of managing postoperative pain, pain associated with nonsurgical procedures and disease-related pain. DESIGN: Retrospective, self-administered descriptive mail survey. SETTING: Level 3 NICUs in Canada. PARTICIPANTS: The head nurses of the 30 Canadian level 3 NICUs in February 1992; 26 (87%) responded. MAIN OUTCOME MEASURES: Five-point Likert scale of Always (in 100% of cases), Often (in 75% to 99%), Usually (in 25% to 74%), Rarely (in 1% to 24%) and Never (in 0%). Selected items were validated through a chart review. RESULTS: Opioids were used postoperatively always or often in 93% (13/14), 88% (15/17) and 65% (11/17) of the NICUs that cared for neonates having undergone cardiac, major and minor surgery respectively. Most of the NICUs did not use paralysis or sedation alone for postoperative pain management. Local anesthesia was used always or often for emergent chest tube placement in 16% (4/25) of the NICUs, for elective chest tube placement in 48% (12/25) and for lumbar puncture in 12% (3/24). An analgesic was rarely or never used for insertion of a tracheal tube in emergent situations in 88% (23/26) of the NICUs and in elective situations in 84% (21/25); the corresponding figures for sedative use were 85% (22/26) and 73% (19/26). Only 22% (5/23) used opioids regularly in cases of nonsurgically managed necrotizing enterocolitis. Physicians alone determined the rate of opioid weaning in 54% (13/24) of the NICUs. Opioids were usually described as being weaned as tolerated. CONCLUSIONS: Analgesic use for the management of postoperative pain in neonates having undergone cardiac and major surgery is frequent but continues to be infrequent in the postoperative care of patients having undergone minor surgery in some NICUs. Procedural and disease-related pain is frequently untreated or undertreated. Guidelines for establishing a protocol to manage pain in NICUs are given.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anand K. J., Brown M. J., Bloom S. R., Aynsley-Green A. Studies on the hormonal regulation of fuel metabolism in the human newborn infant undergoing anaesthesia and surgery. Horm Res. 1985;22(1-2):115–128. doi: 10.1159/000180083. [DOI] [PubMed] [Google Scholar]
- Anand K. J., Brown M. J., Causon R. C., Christofides N. D., Bloom S. R., Aynsley-Green A. Can the human neonate mount an endocrine and metabolic response to surgery? J Pediatr Surg. 1985 Feb;20(1):41–48. doi: 10.1016/s0022-3468(85)80390-0. [DOI] [PubMed] [Google Scholar]
- Anand K. J., Carr D. B. The neuroanatomy, neurophysiology, and neurochemistry of pain, stress, and analgesia in newborns and children. Pediatr Clin North Am. 1989 Aug;36(4):795–822. doi: 10.1016/s0031-3955(16)36722-0. [DOI] [PubMed] [Google Scholar]
- Anand K. J., Hansen D. D., Hickey P. R. Hormonal-metabolic stress responses in neonates undergoing cardiac surgery. Anesthesiology. 1990 Oct;73(4):661–670. doi: 10.1097/00000542-199010000-00012. [DOI] [PubMed] [Google Scholar]
- Anand K. J., Hickey P. R. Halothane-morphine compared with high-dose sufentanil for anesthesia and postoperative analgesia in neonatal cardiac surgery. N Engl J Med. 1992 Jan 2;326(1):1–9. doi: 10.1056/NEJM199201023260101. [DOI] [PubMed] [Google Scholar]
- Anand K. J., Hickey P. R. Pain and its effects in the human neonate and fetus. N Engl J Med. 1987 Nov 19;317(21):1321–1329. doi: 10.1056/NEJM198711193172105. [DOI] [PubMed] [Google Scholar]
- Bauchner H., May A., Coates E. Use of analgesic agents for invasive medical procedures in pediatric and neonatal intensive care units. J Pediatr. 1992 Oct;121(4):647–649. doi: 10.1016/s0022-3476(05)81164-3. [DOI] [PubMed] [Google Scholar]
- Beyer J. E., DeGood D. E., Ashley L. C., Russell G. A. Patterns of postoperative analgesic use with adults and children following cardiac surgery. Pain. 1983 Sep;17(1):71–81. doi: 10.1016/0304-3959(83)90129-X. [DOI] [PubMed] [Google Scholar]
- Calabrese J. R., Gulledge A. D. The neonatal narcotic abstinence syndrome: a brief review. Can J Psychiatry. 1985 Dec;30(8):623–626. doi: 10.1177/070674378503000814. [DOI] [PubMed] [Google Scholar]
- Clotz M. A., Nahata M. C. Clinical uses of fentanyl, sufentanil, and alfentanil. Clin Pharm. 1991 Aug;10(8):581–593. [PubMed] [Google Scholar]
- Ellis D. J., Steward D. J. Fentanyl dosage is associated with reduced blood glucose in pediatric patients after hypothermic cardiopulmonary bypass. Anesthesiology. 1990 May;72(5):812–815. doi: 10.1097/00000542-199005000-00007. [DOI] [PubMed] [Google Scholar]
- Franck L. S. A national survey of the assessment and treatment of pain and agitation in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 1987 Nov-Dec;16(6):387–393. doi: 10.1111/j.1552-6909.1987.tb01599.x. [DOI] [PubMed] [Google Scholar]
- Friesen R. H., Honda A. T., Thieme R. E. Changes in anterior fontanel pressure in preterm neonates during tracheal intubation. Anesth Analg. 1987 Sep;66(9):874–878. [PubMed] [Google Scholar]
- Greisen G., Frederiksen P. S., Hertel J., Christensen N. J. Catecholamine response to chest physiotherapy and endotracheal suctioning in preterm infants. Acta Paediatr Scand. 1985 Jul;74(4):525–529. doi: 10.1111/j.1651-2227.1985.tb11022.x. [DOI] [PubMed] [Google Scholar]
- Grunau R. V., Craig K. D. Pain expression in neonates: facial action and cry. Pain. 1987 Mar;28(3):395–410. doi: 10.1016/0304-3959(87)90073-X. [DOI] [PubMed] [Google Scholar]
- Hickey P. R., Hansen D. D., Wessel D. L., Lang P., Jonas R. A., Elixson E. M. Blunting of stress responses in the pulmonary circulation of infants by fentanyl. Anesth Analg. 1985 Dec;64(12):1137–1142. [PubMed] [Google Scholar]
- Mather L., Mackie J. The incidence of postoperative pain in children. Pain. 1983 Mar;15(3):271–282. doi: 10.1016/0304-3959(83)90062-3. [DOI] [PubMed] [Google Scholar]
- Perlman J. M., McMenamin J. B., Volpe J. J. Fluctuating cerebral blood-flow velocity in respiratory-distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med. 1983 Jul 28;309(4):204–209. doi: 10.1056/NEJM198307283090402. [DOI] [PubMed] [Google Scholar]
- Pinheiro J. M., Furdon S., Ochoa L. F. Role of local anesthesia during lumbar puncture in neonates. Pediatrics. 1993 Feb;91(2):379–382. [PubMed] [Google Scholar]
- Purcell-Jones G., Dormon F., Sumner E. Paediatric anaesthetists' perceptions of neonatal and infant pain. Pain. 1988 May;33(2):181–187. doi: 10.1016/0304-3959(88)90089-9. [DOI] [PubMed] [Google Scholar]
- Schechter N. L., Allen D. A., Hanson K. Status of pediatric pain control: a comparison of hospital analgesic usage in children and adults. Pediatrics. 1986 Jan;77(1):11–15. [PubMed] [Google Scholar]
- Schechter N. L. The undertreatment of pain in children: an overview. Pediatr Clin North Am. 1989 Aug;36(4):781–794. doi: 10.1016/s0031-3955(16)36721-9. [DOI] [PubMed] [Google Scholar]
- Srinivasan G., Jain R., Pildes R. S., Kannan C. R. Glucose homeostasis during anesthesia and surgery in infants. J Pediatr Surg. 1986 Aug;21(8):718–721. doi: 10.1016/s0022-3468(86)80395-5. [DOI] [PubMed] [Google Scholar]
- Yaster M., Deshpande J. K. Management of pediatric pain with opioid analgesics. J Pediatr. 1988 Sep;113(3):421–429. doi: 10.1016/s0022-3476(88)80622-x. [DOI] [PubMed] [Google Scholar]


