Abstract
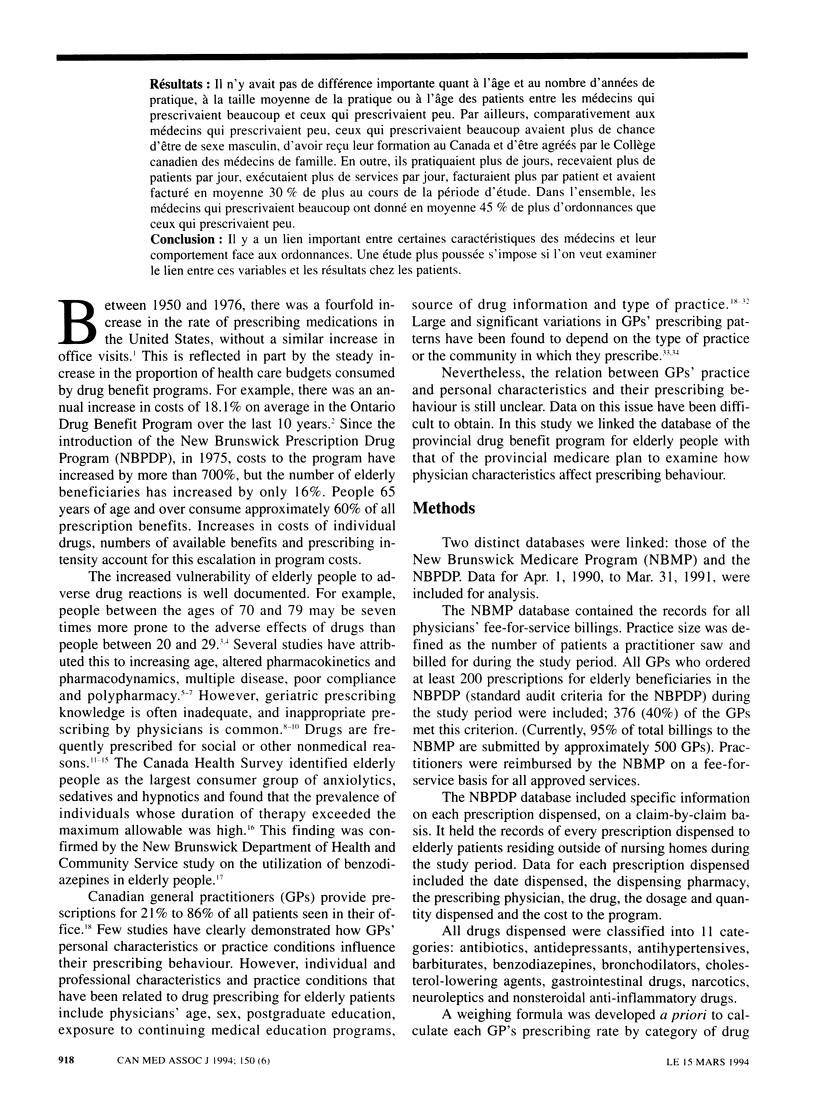
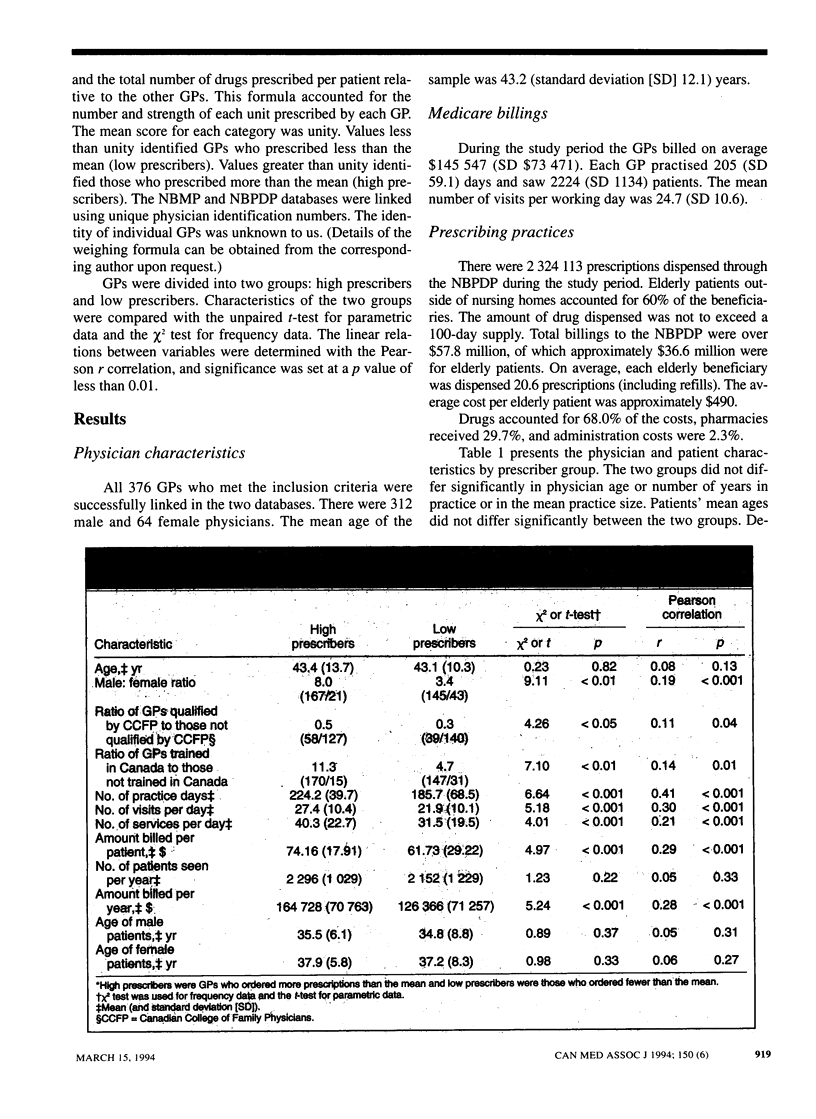
OBJECTIVE: To determine whether there is a relation between physician characteristics and prescribing for elderly patients. DESIGN: Descriptive study linking two provincial databases. SETTING: New Brunswick. PARTICIPANTS: All general practitioners (GPs) in New Brunswick who ordered at least 200 prescriptions for elderly beneficiaries of the New Brunswick Prescription Drug Program between Apr. 1, 1990, and Mar. 31, 1991; eligible GPs accounted for 376 (40%) of all physicians with a general licence in New Brunswick. MAIN OUTCOME MEASURES: GPs' personal and professional characteristics (age, sex, family practice accreditation, country of training and number of years in practice), practice characteristics (number of practice days, number of patients seen and medical services provided per day, average amount of billing per patient, total number of patients seen and their average age, and total amount of billings) and number of prescriptions by category of drug. RESULTS: High prescribers and low prescribers did not differ significantly in age, number of years in practice, mean practice size or patient age. Compared with the low prescribers the high prescribers were more likely to be male, have been trained in Canada and be qualified by the Canadian College of Family Physicians. Also, they had more practice days, saw more patients per day, performed more services per day, billed more per patient and billed on average 30% more during the study period. Overall, the high prescribers ordered on average 45% more prescriptions than the low prescribers. CONCLUSION: There is a significant relation between certain physician characteristics and prescribing behaviour. Further study is required to examine the relation between these variables and patient outcomes.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avorn J., Chen M., Hartley R. Scientific versus commercial sources of influence on the prescribing behavior of physicians. Am J Med. 1982 Jul;73(1):4–8. doi: 10.1016/0002-9343(82)90911-1. [DOI] [PubMed] [Google Scholar]
- Becker M. H., Stolley P. D., Lasagna L., McEvilla J. D., Sloane L. M. Differential education concerning therapeutics and resultant physician prescribing patterns. J Med Educ. 1972 Feb;47(2):118–127. doi: 10.1097/00001888-197202000-00006. [DOI] [PubMed] [Google Scholar]
- Chambers C. D., White O. Z., Lindquist J. H. Physician attitudes and prescribing practices: a focus on minor tranquilizers. J Psychoactive Drugs. 1983 Jan-Jun;15(1-2):55–59. doi: 10.1080/02791072.1983.10472123. [DOI] [PubMed] [Google Scholar]
- Cooperstock R. Sex differences in the use of mood-modifying drugs: an explanatory model. J Health Soc Behav. 1971 Sep;12(3):238–244. [PubMed] [Google Scholar]
- Ferry M. E., Lamy P. P., Becker L. A. Physicians' knowledge of prescribing for the elderly. A study of primary care physicians in Pennsylvania. J Am Geriatr Soc. 1985 Sep;33(9):616–625. doi: 10.1111/j.1532-5415.1985.tb06318.x. [DOI] [PubMed] [Google Scholar]
- Freeman T. R. A study of telephone prescriptions in family practice. J Fam Pract. 1980 May;10(5):857–862. [PubMed] [Google Scholar]
- Gurwitz J. H., Soumerai S. B., Avorn J. Improving medication prescribing and utilization in the nursing home. J Am Geriatr Soc. 1990 May;38(5):542–552. doi: 10.1111/j.1532-5415.1990.tb02406.x. [DOI] [PubMed] [Google Scholar]
- Hurwitz N., Wade O. L. Intensive hospital monitoring of adverse reactions to drugs. Br Med J. 1969 Mar 1;1(5643):531–536. doi: 10.1136/bmj.1.5643.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kofoed L., Bloom J. D., Williams M. H., Rhyne C., Resnick M. Physicians investigated for inappropriate prescribing by the Oregon Board of Medical Examiners. West J Med. 1989 May;150(5):597–601. [PMC free article] [PubMed] [Google Scholar]
- Linn L. S., Davis M. S. Physicians' orientation toward the legitimacy of drug use and their preferred source of new drug information. Soc Sci Med. 1972 Apr;6(2):199–203. doi: 10.1016/0037-7856(72)90025-x. [DOI] [PubMed] [Google Scholar]
- Linn L. S., Davis M. S. Physicians' orientation toward the legitimacy of drug use and their preferred source of new drug information. Soc Sci Med. 1972 Apr;6(2):199–203. doi: 10.1016/0037-7856(72)90025-x. [DOI] [PubMed] [Google Scholar]
- Lohr K. N., Brook R. H. Quality of care in episodes of respiratory illness among Medicaid patients in New Mexico. Ann Intern Med. 1980 Jan;92(1):99–106. doi: 10.7326/0003-4819-92-1-99. [DOI] [PubMed] [Google Scholar]
- Nolan L., O'Malley K. Adverse drug reactions in the elderly. Br J Hosp Med. 1989 May;41(5):446, 448, 452-7. [PubMed] [Google Scholar]
- Renaud M., Beauchemin J., Lalonde C., Poirier H., Berthiaume S. Practice settings and prescribing profiles: the simulation of tension headaches to general practitioners working in different practice settings in the Montreal area. Am J Public Health. 1980 Oct;70(10):1068–1073. doi: 10.2105/ajph.70.10.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SELLERS E. M. THE INFLUENCES OF GROUP AND INDEPENDENT GENERAL PRACTICE ON PATIENT CARE: A COMPARATIVE STUDY IN ONTARIO. Can Med Assoc J. 1965 Jul 24;93:147–157. [PMC free article] [PubMed] [Google Scholar]
- Schmucker D. L. Drug disposition in the elderly: a review of the critical factors. J Am Geriatr Soc. 1984 Feb;32(2):144–149. doi: 10.1111/j.1532-5415.1984.tb05856.x. [DOI] [PubMed] [Google Scholar]
- Schwartz R. K., Soumerai S. B., Avorn J. Physician motivations for nonscientific drug prescribing. Soc Sci Med. 1989;28(6):577–582. doi: 10.1016/0277-9536(89)90252-9. [DOI] [PubMed] [Google Scholar]
- Shimp L. A., Ascione F. J., Glazer H. M., Atwood B. F. Potential medication-related problems in noninstitutionalized elderly. Drug Intell Clin Pharm. 1985 Oct;19(10):766–772. doi: 10.1177/106002808501901024. [DOI] [PubMed] [Google Scholar]
- Shorr R. I., Bauwens S. F. Effects of patient age and physician training on choice and dose of benzodiazepine hypnotic drugs. Arch Intern Med. 1990 Feb;150(2):293–295. [PubMed] [Google Scholar]
- Shorr R. I., Bauwens S. F. Effects of patient age and physician training on choice and dose of benzodiazepine hypnotic drugs. Arch Intern Med. 1990 Feb;150(2):293–295. [PubMed] [Google Scholar]
- Stolley P. D., Becker M. H., Lasagna L., McEvilla J. D., Sloane L. M. The relationship between physician characteristics and prescribing appropriateness. Med Care. 1972 Jan-Feb;10(1):17–28. doi: 10.1097/00005650-197201000-00003. [DOI] [PubMed] [Google Scholar]
- Waldron I. Increased prescribing of Valium, Librium, and other drugs--an example of the influence of economic and social factors on the practice of medicine. Int J Health Serv. 1977;7(1):37–62. doi: 10.2190/FPJT-V9YE-VWM1-UXPA. [DOI] [PubMed] [Google Scholar]


