Abstract
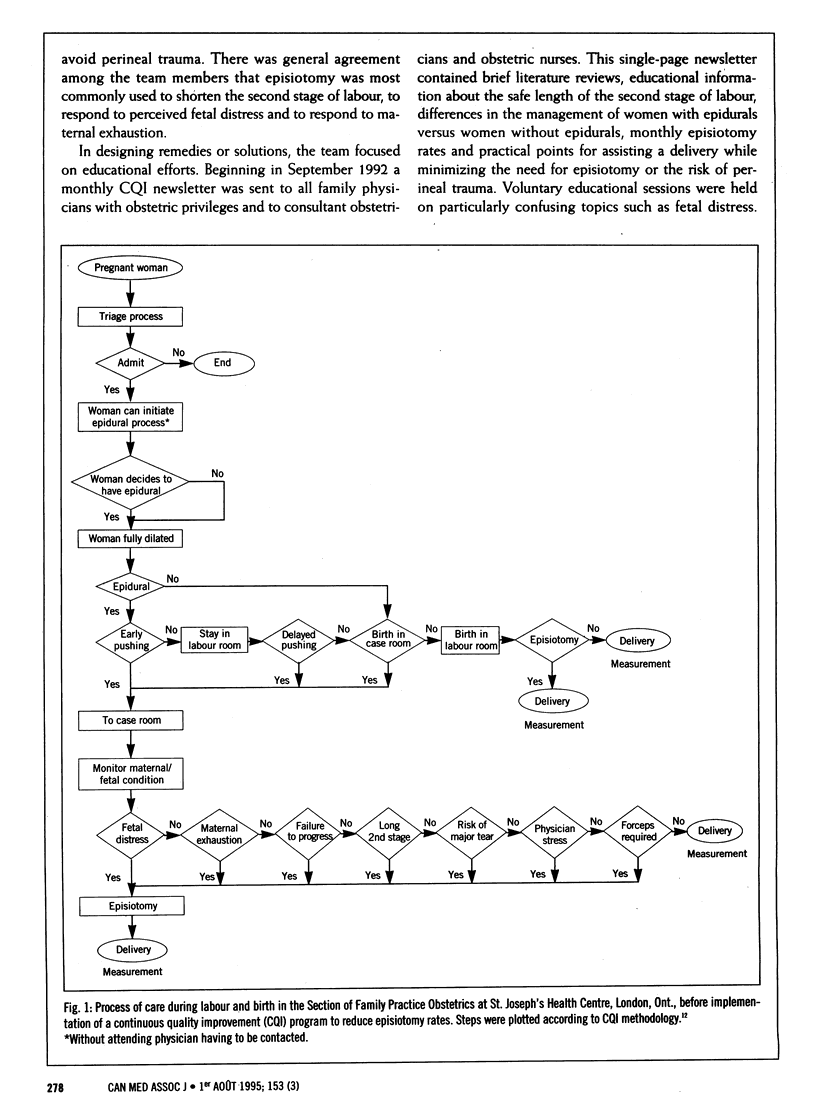
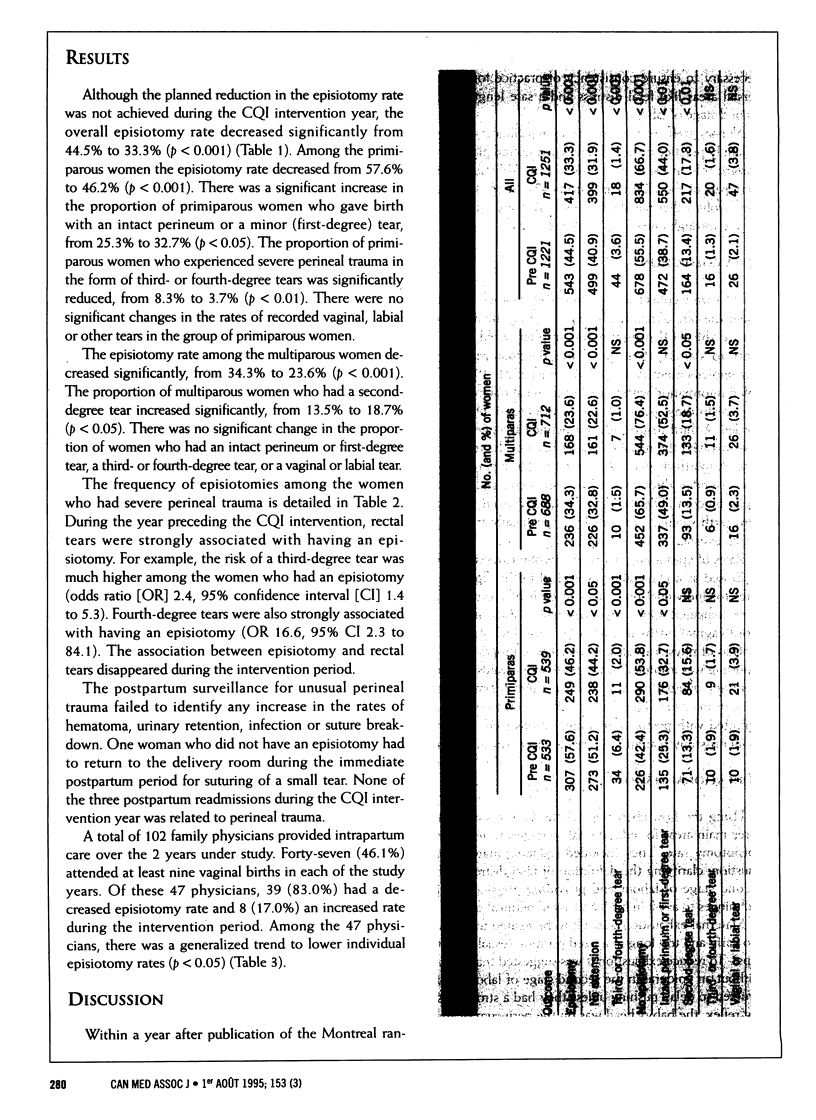
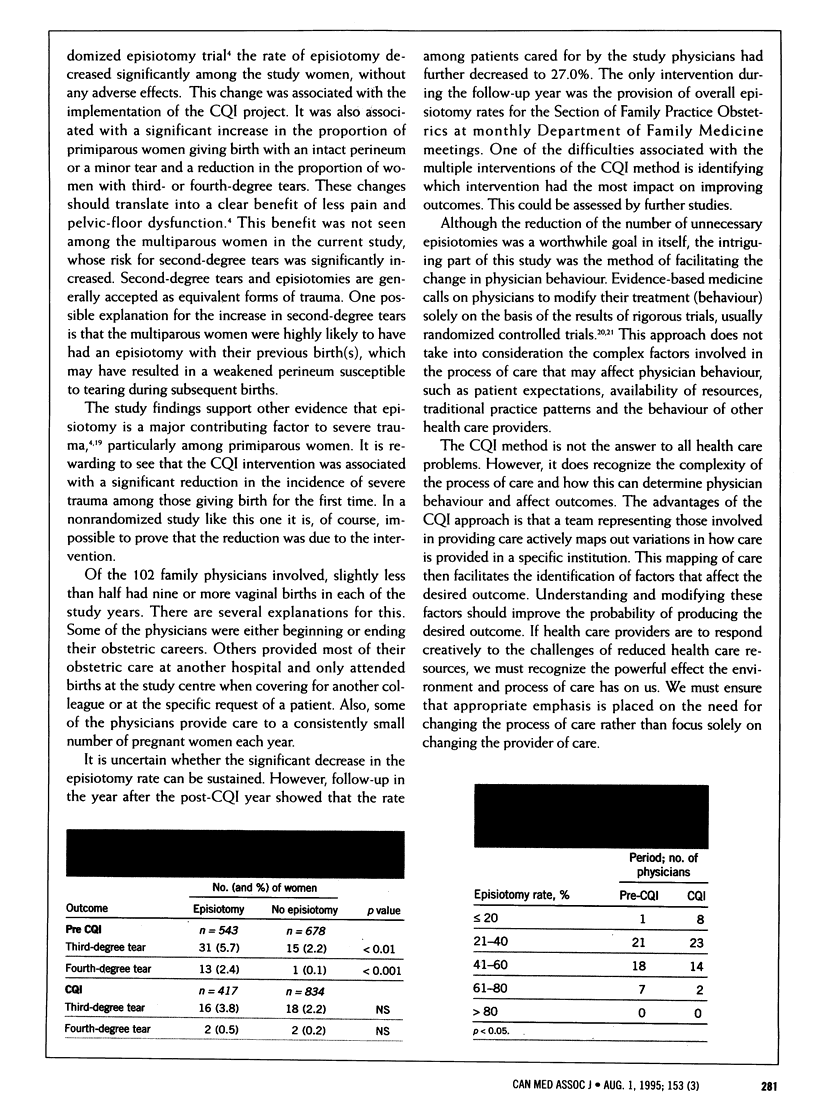
OBJECTIVE: To determine the effectiveness of a continuous quality improvement (CQI) program in reducing episiotomy rates. DESIGN: Before-and-after study; CQI methods were used to examine the process of care during labour and birth. INTERVENTIONS: Identification of care factors that would increase the probability of episiotomy. Implementation of initiatives that would change the process of care to minimize the probability of episiotomy. Educational strategies included promotion of better understanding of what constitutes an appropriate episiotomy rate and ways to reduce maternal exhaustion and true fetal distress as well as manoeuvres to protect the perineum during birth. SETTING: Low-risk family practice obstetrics service in a tertiary care hospital in southwestern Ontario. PARTICIPANTS: All 102 family physicians at the study hospital who provided intrapartum care in the year before and the year during which the CQI program was implemented and the women for whom the care was provided (approximately 1,400 per year). OUTCOME MEASURES: Episiotomy rates (overall, among primiparous and multiparous women, and among individual family physicians) and rates of perineal tear, perineal infection and postpartum readmission. RESULTS: Although the planned reduction in the episiotomy rate was not achieved during the study period, the overall rate decreased significantly from 44.5% to 33.3% (p < 0.001). Among the primiparous women the rate decreased from 57.6% to 46.2% (p < 0.001) and among the multiparous women from 34.3% to 23.6% (p < 0.001). The reduced episiotomy rate among the primiparous women was associated with a significant decrease in the rate of third- and fourth-degree perineal tears and a significant increase in the number of women giving birth with an intact perineum or a minor (first-degree) tear. These benefits were not seen among the multiparous women, whose decreased episiotomy rate was associated with a significant increase in the number of women experiencing a second-degree perineal tear. During the intervention period, there was no increase in the rates of vaginal trauma or postpartum bleeding, infection or readmission because of complications related to perineal trauma. The episiotomy rates for most physicians decreased significantly during the intervention period. CONCLUSIONS: The CQI model may be useful in modifying clinical practices such as episiotomy because it focuses on understanding the process of care and the environment in which care is provided, both of which may have a major impact on physician behaviour. Further study is needed to ascertain the sustainability of the effects of this approach and which components of the model had the greatest effect.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berwick D. M. Continuous improvement as an ideal in health care. N Engl J Med. 1989 Jan 5;320(1):53–56. doi: 10.1056/NEJM198901053200110. [DOI] [PubMed] [Google Scholar]
- Borgatta L., Piening S. L., Cohen W. R. Association of episiotomy and delivery position with deep perineal laceration during spontaneous delivery in nulliparous women. Am J Obstet Gynecol. 1989 Feb;160(2):294–297. doi: 10.1016/0002-9378(89)90428-6. [DOI] [PubMed] [Google Scholar]
- Fleissig A. Prevalence of procedures in childbirth. BMJ. 1993 Feb 20;306(6876):494–495. doi: 10.1136/bmj.306.6876.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J. R., Soohoo S. L. Factors associated with rectal injury in spontaneous deliveries. Obstet Gynecol. 1989 May;73(5 Pt 1):732–738. [PubMed] [Google Scholar]
- Henriksen T. B., Bek K. M., Hedegaard M., Secher N. J. Episiotomy and perineal lesions in spontaneous vaginal deliveries. Br J Obstet Gynaecol. 1992 Dec;99(12):950–954. doi: 10.1111/j.1471-0528.1992.tb13695.x. [DOI] [PubMed] [Google Scholar]
- Henriksen T. B., Bek K. M., Hedegaard M., Secher N. J. Methods and consequences of changes in use of episiotomy. BMJ. 1994 Nov 12;309(6964):1255–1258. doi: 10.1136/bmj.309.6964.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein M. C., Gauthier R. J., Robbins J. M., Kaczorowski J., Jorgensen S. H., Franco E. D., Johnson B., Waghorn K., Gelfand M. M., Guralnick M. S. Relationship of episiotomy to perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation. Am J Obstet Gynecol. 1994 Sep;171(3):591–598. doi: 10.1016/0002-9378(94)90070-1. [DOI] [PubMed] [Google Scholar]
- Laffel G., Blumenthal D. The case for using industrial quality management science in health care organizations. JAMA. 1989 Nov 24;262(20):2869–2873. [PubMed] [Google Scholar]
- Lomas J., Anderson G. M., Domnick-Pierre K., Vayda E., Enkin M. W., Hannah W. J. Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med. 1989 Nov 9;321(19):1306–1311. doi: 10.1056/NEJM198911093211906. [DOI] [PubMed] [Google Scholar]
- Röckner G., Olund A. The use of episiotomy in primiparas in Sweden. A descriptive study with particular focus on two hospitals. Acta Obstet Gynecol Scand. 1991;70(4-5):325–330. doi: 10.3109/00016349109007881. [DOI] [PubMed] [Google Scholar]
- Sleep J., Grant A., Garcia J., Elbourne D., Spencer J., Chalmers I. West Berkshire perineal management trial. Br Med J (Clin Res Ed) 1984 Sep 8;289(6445):587–590. doi: 10.1136/bmj.289.6445.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleep J., Grant A. West Berkshire perineal management trial: three year follow up. Br Med J (Clin Res Ed) 1987 Sep 26;295(6601):749–751. doi: 10.1136/bmj.295.6601.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soliman S. R., Burrows R. F. Cesarean section: analysis of the experience before and after the National Consensus Conference on Aspects of Cesarean Birth. CMAJ. 1993 Apr 15;148(8):1315–1320. [PMC free article] [PubMed] [Google Scholar]
- Thacker S. B., Banta H. D. Benefits and risks of episiotomy: an interpretative review of the English language literature, 1860-1980. Obstet Gynecol Surv. 1983 Jun;38(6):322–338. [PubMed] [Google Scholar]



